- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
In the last few months we have all gotten multiple questions on similarities and differences between orthopedic and sports residencies. In this video below, we've answered the top questions we get to hopefully help start to answer your questions.
7 Comments
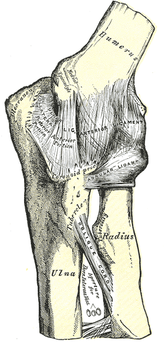 I've spoken before about one of my favorite aspects of this residency: the variety of resources. We routinely utilize the APTA Ortho Section's monograph for each joint, Shirley Sahrmann's texts, and a lecture from the clinical faculty for each joint. Recently, we covered the elbow, wrist, and hand in a couple lectures taught by a Certified Hand Therapist (CHT). CHT's are commonly known as experts in regards to assessing and treating these joints, so I was pretty excited for those lectures. If you have read the clinical practice guidelines on various elbow/wrist/hand pathologies or the monograph for those joints, you likely are aware of many of the commonly described clinical presentations, assessment and treatment techniques. If followed correctly, these patterns typically lead to good results. Recently, my mentor, the other resident, our students, and I got together for some lab practice at the end of the day (another one of my favorite parts). We got to a point where we were discussing alternative assessment, treatment, and even philosophies of the elbow. As I have mentioned before, my mentor is a FAAOMPT and he receives regular updates from his fellowship regarding new assessment and treatment techniques throughout the body. We began discussing the implications of assessing compression versus distraction at the radialhumeral joint. Many elbow injuries result from either a traction or compression force. Think about the patient swinging a tennis racket, carrying a heavy bag, or grabbing onto something superiorly when falling. These are all traction forces. Push ups, a fall on an outstretched hand, etc. are compression forces. We commonly see scripts or we diagnose elbow injuries as overuse injuries, such as tendinopathy. The theory lies in the idea that the tendon is overly stressed from those activities, resulting in pain. While this may be true in some instances, it may not always be correct. Think about how we have previously discussed the effect abnormal spinal mobility can lead to altered neural function and thus changes in muscular activity. We may find a tender or weak muscle or flaired up nerve that is ultimately the result of a poorly functioning joint in the spine. Why can't similar things happen peripherally? They can. It can be argued that either a compressed or distracted radialhumeral joint can result in an irritated radial nerve and lead to altered function of the radial nerve-innervated muscles as a result of altered joint arthrokinematics. This may be presented as "tennis elbow," radial tunnel syndrome, or PIN syndrome. Unfortunately, since this is a relatively new approach, there hasn't been much research performed on the topic. However, I challenge you to assess this joint when treating these elbow conditions in order to help determine the potential contribution for that particular individual. More importantly, we should be thorough with our exams and treat any related joint dysfunctions! The video below discusses how to assess and treat distracted and compressed radialhumeral joints. Additionally, I briefly discuss assessing elbow abduction and adduction. This again plays a role in checking joint mobility and may determine the need for some form of manual therapy or alternative treatment. -Chris  Want to know more about the life of sports physical therapy resident? How about what you should do to get into programs? Or why do a sports vs an orthopedic residency? If you are curious to any of these questions look no further than this google hangout. Representing 5 different sports residencies, you can be sure you get multiple different perspectives. Special thanks to: Joe Micca (UPMC), Michael Scalafini (Cleveland Clinic), Chelseana Davis (OSU), and Sean Bardenett (Ben Hogan) for taking the time to sit down and talk about sports residencies with me. Always great to talk sports PT with other passionate professionals.  Q&A with University of Southern California's Sports Residency Director: Dr. Aimee Diaz. Part 1: What makes your program unique? Part 2: What qualities do you look for in applicants? Part 3: What does a typical work week for residents include? Part 4: What type of jobs have resident graduates obtained? Part 5: Describe the faculty/mentors in the residency For more information on USC's Sports Physical Therapy Residency: http://pt.usc.edu/residency/sports/
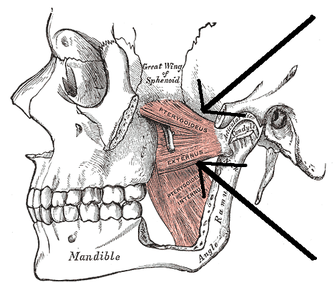
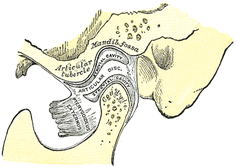 Recently, I had the pleasure of hearing Dr. Cohen, D.D.S. speak on the TMJ. Dr. Cohen is an Orofacial Pain Specialist that works out of the Phoenix area. As you may have noticed, we have not exactly covered the TMJ significantly before on this website due to what we thought was a low prevalence. However, as you'll soon see, it couldn't be further from the truth. For example, did you know that the American Dental Association does not require Dental schools to teach the temporomandibular joint? In fact, treatment techniques for TMJ issues by dentists (distraction, surgery to alter the bone/joint structure, etc.) often actually causes a greater TMJ issue or sometimes a TMJ issue that otherwise did not previously exist. As physical therapists, we are in an excellent position to screen for dysfunction at this joint and direct the patient to proper clinicians if appropriate. Anatomy and Kinesiology: The Temporomandibular Joint is made up of a posterior concave mandibular fossa and anterior convex articular eminence of the temporal bone that is combined with the convex condyle of the mandible. These surfaces are separated by an articular disc that is made primarily of fibrocartilage (this is important because this disc exhibits incredible self-healing abilities!). The disc reciprocally fits the TMJ in that the superior side is convex to match the concavity of the mandibular fossa and the inferior side is concave to match the mandibular condyle convexity (Neumann, 2010). The blood supply and innervation of the articular disc is somewhat debatable in that some say the entire disc is aneural (incapable of signaling pain), while others say only the middle third is aneural, leaving the anterior and posterior thirds with some innervation. With the joint being synovial, there obviously is a fibrous capsule that surrounds it as well. There are also several key ligaments involved with the joint, but that goes beyond the purpose of this review. There are two basic components of jaw opening and closing: rotation and translation. Basically, the first half of the motion occurs as a result of joint mechanics in the inferior side of the articular disc - the convex condyle rolls posteriorly and slides anteriorly (convex-concave rules!). During the second half, the superior part of the disc slides anteriorly on the articular eminence (Neumann, 2010). In general, the primary muscles of mastication include the temporalis, medial pterygoid, lateral pterygoid, and masster. The masseter is responsible for elevation of the mandible, slight protrusion, and, if unilateral, slight ipsilateral excursion. The temporalis elevates, retrudes, and, if unilateral, pulls the mandible ipsilaterally. The medial pterygoid is responsible for elevation and protrusion, while the lateral pterygoid is the only primary muscle that depresses the mandible (along with protrusion). Both muscles contralaterally deviate the jaw if acting unilaterally. It is worth noting that the superior head of the lateral pterygoid has fibers that attach to the capsule, suggesting an involvement with eccentric control of disc translation; however, the evidence is lacking on this. In addition, there are more than a few other muscles that are involved with TMJ function, the suprahyoid and infrahyoid muscles, but the reader is directed to other resources for further information in this area.
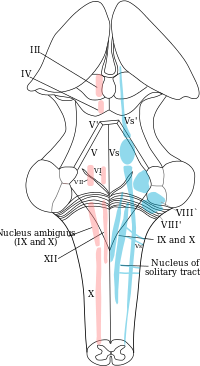
Signs and Symptoms: Some common symptoms of TMD include jaw/ear pain, headaches, ear stuffiness, dizziness, tinnitus, hearing loss, and jaw clicking. True TMJ pain can be identified by asking if the patient has pain with chewing. Remember, the disc is aneural, so the pain is not coming from the disc, but potentially the capsule, ligaments, or muscles involved. How can the ear be involved? The TMJ is connected to the ear's eustachian tube by the "Pinto's ligament." Any abnormal mechanics or pathology in the TMJ can stress the ligament causing ear pain, stuffiness, or even loss of hearing. Another potential cause for ear symptoms is the trigeminocervical nucleus and auriculotemporal nerve. (Fun Fact: Amoxicillin is often used for screening for ear infections. The problem with this is that Amoxicillin also contains an analgesic component. Antibiotics typically take 2-3 days to have effect. If a patient's ear pain subsides a couple hours after taking Amoxicillin, it's possible the TMJ was responsible for the ear pain). Headaches are often associated with TMD patients as a result of hypermobility in either the upper cervical spine or TMJ. Due to the lack of stability, the larger muscles are overused trying to hold the head up, thus causing a headache. This muscle tightness may instead exert excessive pressure over the trigeminal nerve or greater occipital nerve. When dizziness is involved, suboccipital tightness may result in compression of the greater occipital nerve or vertebrobasilar blood flow. Jaw clicking is a result of disc displacement in the TMJ typically. A history of jaw clicking can lead to the patient experiencing either an open or closed locked jaw. The closed locked jaw is related to an anteriorly displaced disc that does not reduce or a muscle spasm. Do not try and stretch these individuals open as you are likely to displace the disc even further forward. An open locked jaw is a result of a posteriorly displaced disc. The symptoms listed above are some of the more common symptoms related to Temporomandibular Dysfunction. Another important finding to consider is that of trigger points. Dr. Cohen spent extensive time discussing the relation of trigger points to headaches, TMD, and head/neck pain in general. If you have ever reviewed some of the trigger point referral patterns by Travell and Simons, you might realize that quite a few muscles have referral patterns to the head and neck that may mimic or contribute to TMD, headaches, etc. In fact, muscles like the temporalis can even refer to teeth, simulating a toothache (dentists may proceed to inappropriately pull a tooth out as a result). Trigger point injections often alleviate these symptoms immediately. While this is useful, remember this just treats the symptoms. We must treat the cause (often abnormal posture and the associated impairments). So be sure to assess trigger point contributions in your examination. Some treatment techniques by physical therapists may also be useful for this i.e. trigger point release, dry needling. Examination: When you are assessing an individual referred for TMD and cervicalgia, your examination should include both (along with the rest of the upper quarter). Some obvious thing to include are ROM, resisted isometrics, segmental mobility, palpation, listening for joint sounds (disc displacement), cotton roll test, and posture. ROM of the TMJ can reveal potential limitations of the capsule. Normal ROM is: 45 mm for depression, lateral excursion is 1/4 of depression, protrusion is 6-9 mm and retrusion is 3 mm (Ho, 2011). Lateral deviation to one side may signify capsular restrictions ipsilaterally, potential muscle dysfunction, or an anteriorly displaced disc without reduction ipsilaterally. This may be represented as a "C-curve" when opening (an "S-curve" is associated with hypermobility). Resisted isometrics can help you to identify a particular muscle that is not functioning properly. Segmental mobility of both the TMJ and upper cervical spine can potentially assist in identifying hyper- or hypomobility in a segment related to the abnormal mechanics. Palpation can be useful for assessing trigger points or tenderness in a capsule. The cotton roll test can help differentiate between muscular and joint involvement. If a patient complains of pain when chewing on one side of the mouth, have the patient bite down on a cotton roll. By doing so, this gaps the ipsilateral TMJ. Thus, if pain is decreased, it would appear the pain is joint related, but if it doesn't change or increases, the pain is muscular (it is still possible that the pain is related to the cervical spine as well). And of course, it all comes back to posture. Knowing the resting position of the teeth is important to understand the individual's TMJ mechanics and we have already discussed the impact cervical posture can have on the TMJ. Also, be sure to check for any poor habits such as bruxism, chewing on ice, grinding teeth, etc. that impact the TMJ.  Treatment: Treatment of TMD contains many of the methods that are regularly used for other joints and vary based on the impairments found and underlying condition. We must educate the patient on the pathology, postural correction, relaxation training for hyperactive muscles, and adjusting the patient's oral habits. Aerobic exercise can be useful in allowing relaxation of TMJ musculature and managing stress (Ho, 2011). The resting position of the mouth includes having the tongue on the palate of the mouth with the mouth closed and teeth not touching in a relaxed manner. Additionally, patients should be reminded to not bite nails, chew on pens, or continue other habits that affect the TMJ. In more acute cases, the patient should consume a softer diet and transition from chewing on the unaffected side to the affected side. Modalities may be used as indicated and joint/soft tissue mobilization can be used based on findings. As discussed before, trigger points can be treated with trigger point injections, dry needling, manual release, botox, etc. The home exercise program should involve retraining the patient on proper opening of the mouth. This is done by keeping the tongue on the roof of the mouth and slowly opening the mouth. This is useful because it prevents the anterior translation phase, thus preventing additional damage to the disc. The technique should be done regularly throughout the day. Isometrics to TMJ muscles are important for improving control of the joint, enhancing stability. Something that needs to be considered in TMD cases is splint therapy. The purposes include relaxing hyperactive muscles, reducing bruxing, altering clenching behavior, redistributing occlusal forces, preventing wear of enamel, and repositioning of a condyle (Ho, 2011). These splints are worn anywhere from constantly to just at night and may last up to 3 months or more. Due to the malleable effects splints have on the mouth, they need to be regularly adjusted. This brings up the important point of how modifiable the TMJ is. Dr. Cohen states that surgery and joint manipulation are the last options. The TMJ has the ability to adapt to changes and maintain full function for affected ligaments and muscles and sometimes even in cases like fractures. As stated several times before, we must include treatment of the cervical spine and entire upper quarter. Remember regional interdependence! This typically includes mobilization, manipulation, METs, etc. to restricted joints and cervical stabilization training. Anterior cervical muscles like the longus colli and longus capitis are often insufficient in patients with abnormal posture and require retraining. This strengthening/stretching/motor control training approach to postural muscles needs to be used down to the lumbar spine even, because poor core stability often leads to forward head displacement. This description of treatment techniques is a brief overview of how to manage patients with TMD. It is in no way all-inclusive. Each specific pathology may have a specific technique or exercise plan that has been shown to be especially beneficial. For example, there are specific exercise plans for displaced discs that are designed to retrain the muscles and recapture the disc in order to produce increased stability and motor control. The reader is advised to seek out other sources or the references for further information on these pathologies. Additionally, the outcome of patients with TMD can be improved with proper coordination with other health care practitioners like Orofacial Pain Specialists. The earlier these patients begin the conservative route, the more likely they will be able to avoid surgery. -Chris References:
Cohen, Richard. "Temporomandibular Dysfunction." Scottsdale Healthcare Orthopedic Residency Lecture. Scottsdale Healthcare Osborn Campus, Scottsdale, AZ. 21 Jan 2014. Lecture. Ho S. The Temporomandibular Joint: Physical Therapy Patient Management Utilizing Current Evidence. Current Concepts of Orthopaedic Physical Therapy, 3rd Ed. La Crosse, WI. 2011. Neumann, Donald. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation. 2nd edition. St. Louis, MO: Mosby Elsevier, 2010. 427-438. Print. Young PA, Young PH, Tolbert DL. Clinical Neuroscience. 2nd edition. Philadelphia PA: Lippincott Williams & Witkins, 2008. 145-149. Print. Recently one of our authors, James Heafner, did a Google+ Hangout with AAOMPT Student Sig Member, Jaime Aparicio. In the segment James and 2 other residents from the Houston Texas Area (1 Orthopedic and 1 Sports Resident) discuss the benefits of residencies, challenges you may face in the next year, and other frequently asked questions applicants may have. It is ~25 minutes long and definitely worth checking out if you are on the fence about applying to residencies! Here is the link to the Student Sig or simply check out the Youtube feed below.  My NFLPA Collegiate Bowl Coverage My NFLPA Collegiate Bowl Coverage Opportunities are everything. Half-way through USC's sports residency and I've already had so many opportunities to grow in a number of ways. Just last week I had the opportunity to cover both the practices and game for the NFL players association collegiate bowl. By far this was the most eye-opening and valuable experience. As the only physical therapist on staff, it was a unique opportunity. My experiences were vast and allowed me to learn about how the NFL works. Speaking with sports agents, NFL scouts, NFL coaches, athletic trainers, doctors, neurologists, and NFL personnel was just a small taste of what my experience was like. Taping players and covering the sidelines was also a lot of fun. Fortunate (and unfortunately for the athlete), I had to run on the field during the game to assess a player's injury. What was so unique about this experience was how you had to handle the situation afterwards. Everyone wants to know the injury but you cannot discuss these things at all with anyone, including an athlete's sports agent, unless given written consent and by going through the proper channels. Mentoring: Mentoring is what I have valued the most up to this point in the residency. Guidance, feedback, and criticism have been vital in my development as a sports physical therapist. New exercises, new manual therapy treatments, new ways to evaluate, and new ways to think have all been part of my mentoring experiences. Learning from the sports medicine doctors at Kerlan Jobe, both in the office, in the surgery room, and during the games has provided me the ability to become comfortable understanding where the doctor's point of view comes from. On-field/Training Room Experience: This area has been the second most valued part of the residency for me. I've had quite a few hours on the field by now in a variety of settings: high school football, soccer, basketball; collegiate football, basketball, baseball; Pro beach volleyball; and NFLPA football. With my future on-field/training room experiences to include the Anaheim Angels spring training and another professional team experience, my excitement and experience continues to grow. On average I spend about 4-6 hours in a collegiate training room evaluating and treating college athletes each week. My time covering practices and games can sometimes be up to 18 hours a week! These are all excellent opportunities to see a variety of different injury presentations and have the ability to critically think. Miscellaneous: With USC's sports residency including so many different components, it can be easy to forget the little things. For example, access to USC's libraries, pubmed, after hour labs, alumni shadowing opportunities, and the research labs are just some of the amenities I have taken advantage of at USC. Next week I'll be going to the gross anatomy lab with one of the orthopedic residents just because we want to review again. Lastly, the camaraderie with the other orthopedic and sports residents. Despite all the hard work and sacrifices, all of the residents are very close and enjoy each other's company. We all want to help each other out and have a good time along the way. These are what make a GREAT residency experience. Having a variety of opportunities is what is so vital in a sports resident's experience. What the resident takes advantage of is his/her prerogative but it certainly has been incredible for me at this point. -Brian  Each month at the Harris Health Orthopedic Residency, one of the clinicians holds a journal club. Last month, one of my fellow residents and I chose to lead the journal club. We chose the recent JOSPT editorial written by Dr. Benz and Dr. Flynn entitled, "Placebo, Nocebo, and Expectations: Leveraging Positive Outcomes." This article was a great introduction to the topic of the Placebo Effect. To begin, you must first ask yourself: "How much do I currently use the placebo effect in my practice?" or better yet, "Am I using placebo effects without knowing it?" A placebo is defined as a simulated or otherwise medically ineffectual treatment for a disease or other medical condition intended to deceive the recipient. To answer the first question, we ALL use placebos with each patient interaction, whether intentionally or not. Our clinical mannerisms, our tone of voice, how we dress, and the clinic environment are all placebo effects. BUT, in order for a placebo to be effective, the patient must be able to assign a positive meaning to these things. An interesting study looked at two groups of people given a certain medication. One group was given an Aspirin, the second group was given the generic form of Aspirin. The chemical composition was the exact same; however, the group who received Aspirin had much better results. How is this possible? The group who received Aspirin were able to assign a meaning or positive correlation with that intervention. They could both physiologically and psychologically agree with the treatment, and therefore the treatment was more effective. The placebo effect is all about expectations! Dr. Benz and Flynn conclude the editorial by saying we should use the placebo as another "tool in the proverbial tool kit." They say that the power of the mind to react positively to a genuinely weak (think sham) but perceptually agreeable intervention is far more compelling than forcing a highly evidenced based intervention on a patient who cannot assign meaning to that intervention. Next time you are trying to "sell" a patient on an intervention, think about the words you use, how you approach the subject, and the patient's expectation. Above all, act confident. If you display confidence in the treatment, the patient will have more confidence as well. -Jim
Something you may have realized by now is that you rarely get a patient with just and orthopaedic condition. Frequently, patients have multiple co-morbidities that affect how you can implement your interventions. Or maybe you get a referral for something like "balance/gait training." We have received referrals for "cervical strain," but the primary concern is the patient's balance deficits. These are just neurological examples. Consider a patient with deficits in the hand or B&B involvement. These conditions are perfect for consulting a hand therapist or pelvic floor therapist respectively. Sometimes it is essential that a patient receives multiple forms of therapy. A patient's underlying pelvic floor dysfunction may be related to the neurological symptoms in the lower extremity! In a setting like we have with hand therapists, neuro PTs, ortho PTs, pelvic floor PT, and speech therapists, we are able to consult regularly with any aspect of our case. On the flip side, you often get consulted by them for orthopaedic concerns! We have been asked to quickly examine patients of the neuro PTs, occupational therapists, and pelvic floor PTs multiple times. Often following this examination, patients may require a script for orthopaedic physical therapy or potentially they just need a quick manual therapy treatment for the problem. Either way, you can see how beneficial it is being in a multi-disciplinary setting like this. You have the ability to consult with other practitioners that could be key components to your care, along with being consultants for potential underlying orthopaedic issues!
-Chris and Jim  People always say that time goes by faster as you age, but I had never really thought about the truth of his statement until this year. When I was a student, time seemed to have no relevance. School was a protective bubble from reality. Now that I am working and have the freedom to create my own schedule, my scope of time has changed. It is hard for me to grasp that I have already been at the Harris Health System for 3 months. I am not sure if the time has gone so fast because of the hard work and long hours or simply because it has been a fun adventure. I am going to sum up my experiences thus far in 3 words: Challenging, Mentorship, and Growth. Challenging: Being part of any Orthopedic Residency program is challenging (as it should be). It is a 1-yr program that prepares someone to take a Specialty Examination. If it was not difficult, I would be questioning why I was there. But the intensity of the Harris Health Residency has been unique. I was always considered a fairly competent PT student from my clinical instructors. When first arriving at Harris Health, regardless of my clinical competence, I had to overcome the barriers of working with a complex patient population. Since I work at the county hospital, many of my patients speak Spanish as their primary language (I do not speak Spanish). They come from low socioeconomic backgrounds and have little health awareness. Little health awareness+ Low socioeconomic status + multiple comorbidities= Chronic pain. Regardless, I spent the first few weeks understanding my environment and learning how to treat this special population. As I was trying to keep my head above water in the clinic, I was also taking 3 didactic modules: Foundational Sciences, Sports/ Exercise Prescription, and Research. My residency director, Dana Tew, places these 3 modules first because of the high importance placed on differential diagnosis and understanding how to read the literature. All 3 modules were incredible learning experiences and each discussed their respective topics in much more detail than I received in PT school. The other aspect that makes Harris Health challenging (and awesome) is that everyone else in the clinic is much more intelligent than you. In the clinic gym, I am practicing around 6 or 7 OCS and FAAOMPTs. This combination of specialty degrees exists in ~1% of all physical therapists. Having a handful of them practicing next to you and mentoring you is unheard of (literally there are only a few other clinics in the entire country with this level of specialization). Every clinician is working towards or has achieved specialization. Mentorship: Mentorship is the #1 thing that separates a residency program from any typical first job. At Harris Health we receive a minimum of 5 mentor hours per week. I switch mentors every 10-12 weeks to learn different skills and see different practice styles. Essentially, they watch me treat a patient and provide critical feedback on how to become a more efficient practitioner. Aside from improving my treatment style, the mentors have also helped advance my manual techniques. If a patient does not show up to their appointment, we drop the books and practice techniques. These practice sessions have really helped hone my palpation skills and improve my diagnostic abilities. It is these 1-on-1 sessions that have helped my clinical skills the most. Growth: It is often hard to detect change in your practice or personal growth unless you take a moment to reflect on where you once were. Coming out of PT school, I knew a little on a bunch of subjects. Translating that into practice, my evaluations were all over the place. I wanted to know every impairment and practice every test. One way the residency has helped me grow is in my efficiency. For example, if a patient demonstrates a positive Trendelenburg during a gait assessment, there is no need to test their posterior gluteus medius strength. They have already demonstrated weakness during a functional test. The art of observation is such a simple skill that is constantly overlooked. Taking a step back from your patient and looking at their injury in the context of their life will do great things for your treatment session and expectations for achieving goals. I would definitely not call myself an expert, but I am getting much better at synthesizing this information and diagnosing accordingly. In summary, my first 3 months have been great. As with anything in life, the amount of hard work and dedication you put into something will correlate with how much you receive in the end. To anyone who is on the fence about pursuing a residency, I highly recommend it. If a challenging experiences, Mentorship, and Professional Growth are things you are interested in, check out the Harris Health System Residency. Applications are due Feb. 1, 2014. -Jim |
Copyright © The Student Physical Therapist LLC 2023


 RSS Feed
RSS Feed