- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
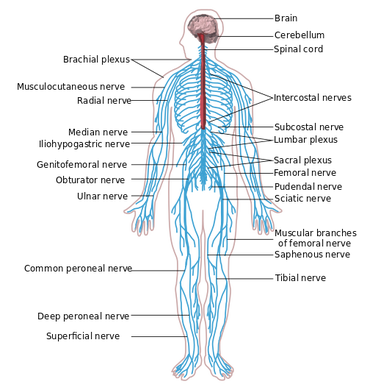
I recently had my second fellowship class which focused on joint manipulation and adverse neural tissue tension. As you may have noticed with the recent increase in posts related to the neural system, the class had quite an impact on me. The obvious benefit the manipulation portion of the course was a dramatic improvement in our technique and clinical reasoning behind when and where to do a manipulation. As beneficial as that was, the part of the course focusing on neural tension had an even greater impact. Adverse Neural Tissue Tension can be defined as: "an abnormal physiological and/or mechanical response from the nervous system that limits its normal range of motion or stretch capabilities." Due to the connections of the central and peripheral nervous systems, tests like the Slump Test and other neural tensioning exam measures can be used to identify dysfunctional neural pathways. These connections can become problematic as tension in the peripheral nervous system can be transmitted to the central nervous system as the perineum transfers tension to the spinal dura matter. Think about how a Straight Leg Raise Test works. The tension in the sciatic nerve is transferred to the lumbar spine due elevation of the leg. The systems are linked both physically and electrically. Blood supply is essential for normal nerve function and to allow the electrical signals to be transmitted. Normal neural function can be affected by compression, stretch, friction, and disease. Double crush syndrome occurs when injury occurs to one area of a nerve due to being at elevated risk secondary to an injury to another part of the same nerve/spinal segments. Normal neural flow is disrupted as pressure increases or blood flow decreases. The greater the pressure, the quicker the axonal flow is slowed. For example, pressure at 20 mmHg begins to affect nerve conduction after 8 hours while pressure at 30 mmHg takes only 2 hours. The effects of this pressure are reversible, but often take prolonged periods of relief. Pressure of 400 mmHg for 2 hours takes 1 week to recover. It is the accumulation of the slowing of a nerve at different points that truly defines double crush syndrome as may with diagnoses such as carpal tunnel syndrome also have dysfunction in the cervical spine. The patient may present with primary complaints of pain in the distal nerves, but the inclusion of a history of proximal pain or injury may be the key to returning to 100%. Next time you have a patient with "lateral epicondylitis," check for radial nerve tension and investigate the neck for any dysfunction as well.
So how do we determine if the nervous system is involved? Nerves typically have a rather vague presentation. Musculoskeletal complaints, on the other hand, tend to present with a more isolated area being affected. Some of the keys things I were taught to assess for in our class included palpation/tensioning of nerves and spinal mobility assessment. When your patient is describing their area of pain, consider what nerves typically are responsible for sensation in the area. I recognize that the graphs of nerve layouts only represent the most common presentation (~30% of the population), so we must rely on palpation of the nerves to assist us (TSPT Premium Channel members can expect videos of how to palpate the nerves in the LE's in a few weeks!). In general, the nerve diagrams can help us with those vague complaints of pain. A nerve that shows signs of irritation will be tender to palpation and present with positive findings on neural tensioning. During a neural tension test, if pain is increased with palpation, that increases the likelihood of contribution to the patient's complaints. Finally, any time you find signs of nerve pain, it is recommend you examine the spine thoroughly. Look for segmental restrictions and pain with segmental mobility testing. It may present with something as simple as being "tender," but being tender is not normal. Based on your findings in the spine, treat accordingly (improve motion is restricted areas and control motion in hypermobile areas). As always assess, treat, and reassess. We should be able to make pretty rapid gains in our patients with neural tension unless that are showing signs of central sensitization. -Chris
10 Comments
|
Copyright © The Student Physical Therapist LLC 2023

 RSS Feed
RSS Feed