- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 I recently read a post about how manual therapy does not really require "skill." Initially, I found the post somewhat infuriating as I have been making my way through a residency that is heavy in manual therapy. However, after reading some of the articles referenced on the post and after following The Manual Therapist blog for awhile, I realized that the popular theories behind the effectiveness of manual therapy may not be as accurate as I thought. That doesn't mean manual therapy isn't effective, but that it may have a different mechanism. This inspired me to do a review on the literature from this alternative perspective. Soft Tissue Mobilization There are various soft tissue techniques (Graston Technique, ASTYM, trigger point release, etc.) that are based on the theory of collagen deformation. Although largely based on theoretical and mathematical models, studies have shown that it requires greater forces than human ability can apply to deform fascial tissue even 1% (Chaudhry et al, 2008). This may be difficult to accept for some therapists, as many will claim feeling a tissue "release" with overpressure. However, it has been shown that the manual pressure applied by therapists actually stimulates mechanical receptors in the tissue, which lowers sympathetic tone in the tissue and a "release" of the adhesion (Schleip, 2003). Again, that doesn't mean the techniques performed don't work, just that they don't work based on the theorized mechanism. This is advantageous to understand as it may alter our technique choice and how we implement it. I have training in IASTM (Instrument-Assisted Soft Tissue Mobilization) based on this neurological effect. Why perform a technique that may injure a patient via bruising, or worse, when we can be as, or more, effective doing something less invasive? Stretching Stretching is a treatment technique that has been a foundation of physical therapy for decades. Quite a bit of research has been done on the topic. In school, the standard practice is that 30 seconds of static stretching is required to get plastic deformation on tissues. But does this actually occur? Without a doubt, it would appear that people can "stretch" their muscles further after a designed stretching program. There are many theories as to how this happens: viscoelastic deformation, plastic deformation of connective tissues, increased sarcomeres in series, and neuromuscular relaxation (Weppler & Magnusson, 2010). However, there appears to be insufficient evidence for each of these areas. With regards to the viscoelastic model, studies have shown that the changes that do occur are small and have short duration. No evidence has been found for true plastic (or permanent) deformation of muscle tissue via stretching. Many report that prolonged immobilization results in altered numbers of sarcomeres in series - on a stretch they increase in series and in a contracted position they decrease. These studies have been inappropriately applied to static stretches. In fact, it was found that after removal of the immobilization, the sarcomere number go back to the original amount. What is often ignored is that these studies are performed on animal muscle tissue by themselves. We do not truly know how sarcomere react in series to stretching in conjunction with tendons, other fascial structures, skin, etc. This is an important component as that is how the body truly functions and we cannot separate out muscle from those other structures when stretching. The neuromuscular relaxation theory is based on altering the stretch reflex to allow a muscle to relax (and thus "stretch") further. Studies have been unable to prove this theory valid with no alterations in the EMG activity of the stretched muscles. In fact, regular stretching was shown to have no significant change on joint mobility, pain, spasticity, or functional limitations in those with neurological conditions (Katalinic et al, 2011). An alternative theory that is presented is changes in muscle length are actually due to a change in perception of stretch (Weppler & Magnusson, 2010). There has been limited evidence to support this theory, but it is based upon a study that showed an increase in end-range joint angle with no change in applied force and no permanent change in length (no plastic deformation). The end-range joint position was based upon subjective sensation of a "stretch." Mobilization and Manipulation With my residency training, a significant amount of time and effort was placed into trying to isolate and locate a specific hypomobile segment to treat. Needless to say, I became somewhat defensive when I heard there was little support for being so specific. Studies have shown that there is no greater benefit for manipulation of a targeted (hypomobile/painful accessory motion based on examiner assessment) joint manipulation compared to a non-specific joint manipulation (Chiradejnant et al, 2003) (Aquino et al, 2009) (Schomacher 2009) (Nyberg & Russell Smith, 2013). However, each of the studies had limitations: chronic pain, potential patient population bias, etc. These findings lend support to the clinical prediction rules that are not specific in nature and may suggest another sign of potential neurological impact and basis for our manual therapy techniques. What exactly happens with a manipulation is difficult to understand. I remember being taught that the cavitation heard is a result of the fluid in the joint capsule quickly evaporating due to the expanded volume of the capsule (and fixed fluid) as a result of the thrust. Whether or not these capsular changes are maintained over time, or even occur, is lacking in evidence. That doesn't mean manual therapy isn't useful. Clinical predictions rules have been developed for patients with neck or low back pain that would benefit from a manipulation (Cleland et al, 2007) (Puentedura et al, 2012). There are those that suggest a mobilization can be as effective as a manipulation, with the only benefit being a manipulaiton can accomplish the same result in less time, but some research shows manipulations may actually be superior. Manipulations have been shown to have a greater effect on ROM, pain, disability and muscle performance compared to non-thrust mobilizations (Dunning JR et al, 2010). Manipulations to the thoracic spine were shown to have a more significant effect on neck pain than mobilizations. (Cleland et al, 2007). With the risk for injury to various structures in the cervical spine, many are hesitant to even consider a grade V thrust to the area. The only reason it is worth considering is that cervical manipulations had a greater effect than thoracic manipulations on neck pain (Puentedura et al, 2011). It is worth noting that with any manipulation or mobilization, we must carefully screen our patients for contraindications such as osteoporosis, RA, chronic steroid use, etc. Conclusion In summary, the results we get from our manual techniques may not be due to the theories on which we were trained, but that does not mean it isn't skilled. A level of clinical reasoning is beneficial to understanding how and why manual therapy treatments can be applied. Manipulations and mobilizations may not be as specific as we thought, but a certain level of training typically is required to be able to perform. But why do those changes occur? While the current popular theories of various manual therapy techniques may have the positive impact we desired, they may not be accurate. This is worth discussion and further investigation to make our treatments as effective as possible. Why injure our patients with certain manual therapy treatments when this can be avoided? Some evidence suggests that we may alter neuromuscular perception by activating mechanoreceptors. While this is not concrete evidence, it may be worthy a topic of research in the future and may play a role in how we can be most effective with our treatments. -Chris References:
Aquino RL, Caires PM, Furtado FC, Loureiro AV, Ferreira PH, & Ferreira ML. (2009). Applying Joint Mobilization at Different Cervical Vertebral Levels Does Not Influence Immediate Pain Reduction in Patients with Chronic Neck Pain: A Randomized Clinical Trial. Journal of Manual & Manipulative Therapy. 2009 April;17(2): 95-100. Chaudhry H, Schleip R, Ji Z, Bukiet B, Maney M, & Findley T. (2008). Three-Dimensional Mathematical Model for Deformation of Human Fasciae in Manual Therapy. Journal of American Osteopathic Medicine. 2008 Aug; 108(8):379-390. Chiradejnant A, Maher CG, Latimer J, & Stepkovitch N. (2003). Efficacy of "Therapist-Selected" Versus "Randomly-Selected" Mobilisation Techniques for the Treatment of Low Back Pain: A Randomised Controlled Trial. Australian Journal of Physiotherapy. 2003; 49(4):233-241. Cleland JA, Childs JD, Fritz JM, Whitman JM, & Eberhart SL. (2007). Development of a Clinical Prediction Rule for Guiding Treatment of a Subgroup of Patients with Neck Pain: Use of Thoracic Spine Manipulation, Exercise, and Patient Education. Physical Therapy. 2007 January;87(1):9-23. Cleland JA, Glynn P, , Whitman JM, Eberhart SL, MacDonald C, & Childs JD. (2007). Short-Term Effects of Thrust Versus Non-Thrust Mobilization/Manipulation Directed at the Thoracic Spine in Patients with Neck Pain: A Randomized Clinical Trial. Physical Therapy. 2007 April;87(4):431-440. Dunning JR, Cleland JA, Waldrop MA, Arnot C, Young I, Turner M, & Sigurdsson G. (2010). Upper Cervical and Upper Thoracic Thrust Manipulation vs Non-Thrust Mobilization in Patients with Mechanical Neck Pain: A Randomized Controlled Trial. Journal of Manual & Manipulative Therapy. 2010 December;18(4):175-180. Katalinic OM, Harvey LA, & Herbert RD. (2011). Effectiveness of Stretch in the Treatment and Prevention of Contractures in People with Neurological Conditions: A Systematic Review. Physical Therapy. 2011. Jan;91(1): 11-24. Nyberg RE & Russell Smith A. (2013). The Science of Spinal Motion Palpation: A Review and Update with Implications for Assessment and Intervention. Journal of Manual & Manipulative Therapy. 2013 Aug;21(3):160-167. Puentedura EJ, Cleland JA, Landers MR, Mintken P, Louw A, & Fernandez-de-las-penas C. (2012). Development of a Clinical Prediction Rule to Identify Patients with Neck Pain Likely to Benefit from Thrust Joint Manipulation to the Cervical Spine. JOSPT. 2012 July;42(7):577-592. Puentedura EJ, Landers MR, Cleland JA, Mintken P, Huijbregts P, & Fernandez-de-las-penas C. (2011). Thoracic Spine Thrust Manipulation Versus Cervical Spine Thrust Manipulation in Patients with Acute Neck Pain: A Randomized Clinical Trial. JOSPT. 2011 April;41(4). Schleip R. (2003). Fascial Plasticity - A New Neurobiological Explanation: Part 1. Journal of Bodywork and Movement Therapies. 2003 Jan;7(1):11-19. Schomacher J. (2009). The Effect of an Analgesic Mobilization Technique when Applied at Symptomatic or Asymptomatic Levels of the Cervical Spine in Subjects with Neck Pain: A Randomized Controlled Trial. Journal of Manual & Manipulative Therapy. 2009 April;17(2): 101-108. Weppler CH & Magnusson SP. (2010). Increasing Muscle Extensibility: A Matter of Increasing Length or Modifying Sensation? Physical Therapy. 2010 March;90(3): 438-449.
2 Comments
Cervical spine pain is one of the more common complaints seen in outpatient orthopaedic physical therapy. With the relation to the rest of the upper quarter, the shoulder and thoracic spine, it is essential we be as proficient as possible when assessing and treating the region. While this may seem obvious, it is interesting to note how hesitant some clinicians are in treating the upper cervical spine. Why? Because it is different and there is risk for fatal injury. The upper cervical spine is made up of the Atlantooccipital Joint and the Atlantoaxis Joint. These joints have different anatomical and kinesiological considerations compared to the rest of the cervical spine. With the frequency with which the cervical spine is involved in upper quarter dysfunction, as well as temporomandibular dysfunction, it is imperative we have a solid understanding of the joints. 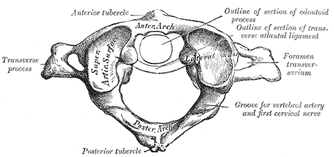 Atlantooccipital Joint The Atlantooccipital Joint (AO) is made up of the atlas and occiput. The atlas has no body, pedicles, laminae, or spinous process, unlike typical vertebrae. There is an anterior arch with an anterior tubercle for attachment of the anterior atlanto-occipital membrane (Neumann, 2010). The posterior arch is larger and has a posterior tubercle. Additionally, there are two large transverse processes that are palpable between the mastoid process and mandibular ramus. There are two large concave facets that face medially and superiorly in order to accept the occipital convex condyles that face inferiorly and laterally (Abernethy, 2014). The atlanto-occipital membrane connects the anterior portion of the foramen magnum to the anterior arch of C1 for anterior-posterior stability. The posterior atlanto-occipital ligament connects the posterior ring of C1 to the occiput at the foramen magnum as well. This ligament is important for anterior translation of C1 and vertical translation of the occiput. Additionally, there are joint capsules surrounding the AO joints that limit movement in each direction. There are 2 degrees of freedom in the AO joint: flexion/extension and frontal sidebend (Abernethy, 2014). The OA joint is responsible for 10 degrees of flexion, 25 degrees of extension, 5 degrees of sidebend, and 4 degrees of conjugate rotation. To fully comprehend the arthrokinematics of the AO joint, we must know the plane of the joint. During flexion, there is a bilateral lateral, posterior, and superior (LPS) motion, while there is a bilateral medial, inferior, and anterior motion for extension (MIA). In order to determine which part and which side of the joint is restricted, we assess sidebend. Upper cervical sidebend to the left, results in left AO MIA and right AO LPS. In other words, if you sidebend the upper cervical spine to the left, you are essentially flexing on the right and extending on the left. To determine which side is at fault for the motion restrictions, sidebending should be reassessed in flexion and extension. For example, if sidebending to the left feels restricted in neutral, it is possible that either flexion on the right or extension on the left (or both) are limited. In a normal joint, sidbending should be smooth and through an axis that runs through the tip of the nose. When placed in flexion (of the same restricted motion), sidebend to the left now biases the right joint. By initially placing the AO joints in flexion, the condyles are moved lateral, posterior and superiorly (LPS). Thus, if there is a restriction on that right side, the condyle will meet its barrier sooner compared to neutral. By placing the AO joints in extension, the condyles are then moved medially, inferiorly, anteriorly (LIPS). This forces the condyle on the left to meet its barrier sooner compared to neutral if there is a restriction. Typically, a flexion limitation is found due to the frequency with which we see forward head posture. If you find an extension limitation, I recommend re-checking the joints.
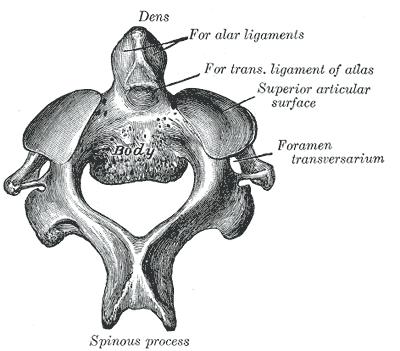
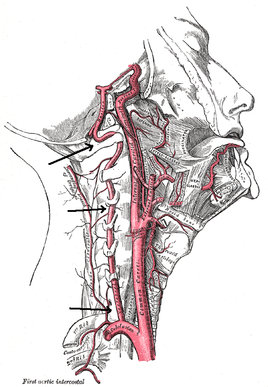
The axis of rotation is through the dens. When rotating to the left, the ipsilateral side of the atlas glides posteriorly, while the contralateral side glides anteriorly (Abernethy, 2014). The AA joint is responsible for 35 degrees of rotation bilaterally, 8 degrees of flexion, and 10 degrees of extension. There are two methods that are commonly used for assessing motion at the AA joint. One is the Flexion-Rotation Test, where the cervical spine is maximally flexed (and maintained there), while rotation is performed bilaterally. The issue with this test is that it tends to also include motion at the C2-3 joint, resulting in at least 45 degrees of rotation in a normal joint bilaterally. To truly assess AA rotation, maximally sidebend the cervical spine ipsilaterally and rotate contralaterally, while maintaining chin tuck (if chin tuck is lost, isolation to C1-2 is lost). This is also a position for manipulation. It should be noted that in those with moderate degeneration of the cervical spine (and presents of significant osteophytes), cervical sidebend may be limited, resulting in decreased ability to isolate the AA joint. Ligament and Artery Testing People are often wary of treating upper cervical dysfunction manually due to some of the potential risks for fatal injury. The cervical vertebrae house the spinal cord and vertebral arteries - structures that are necessary for ordinary brain and motor function. Therefore, we must assess two areas: stability and blood flow. It is recommended that stability is assessed first due to the end range positions required for vertebral artery testing. The two ligament tests required are the Transverse Ligament Test and the Alar Ligament Test. The transverse ligament runs from one side of the arch of C1 wrapping around the dens to the other side of the arch of C1 (Abernethy, 2014). This ligament is 7-8 mm thick and keeps the dens in contact with the atlas, preventing anterior dislocation. The alar ligaments run superiorly and laterally from the dens to the occiput, resisting posteiror translation of the dens and occipital rotation contralaterally. If any of the tests are positive, a provocation of neural symptoms may occur. Structural stability of the atlas may also be assessed by compressing the transverse processes of C1 medially at the same time. If movement is detected, there lies the possibility of a Jefferson fracture. This often occurs with an axial blow to the head. Once instability has been cleared, we must check the patency of the vertebral arteries, as the vetebrobasilar system is responsible for 11% of blood flow. The vertebral artery branches off the subclavian and passes superiorly with the longis colli, enters the transverse foramen usually at C6 (but anywhere between C4-7), wraps back around the articular pillar and enters the posterior AO membrane, before entering through the foramen magnum. Here it joins the opposite vertebral artery to form the basilar artery. Vertebrobasilar Insufficiency is assessed with the Vertebral Artery Test. If you look at the diagnostic accuracy of the test, it would appear there isn't really a reason to even perform the test. With a sensitivity of 0% and a specificity of .67-.9%, a negative test means absolutely nothing and a positive test means the patient may have vertebrobasilar insufficiency. Positive symptoms include: dizziness, diplopia, dysarthria, dysphagia, drop attacks, nausea and vomiting, sensory changes, nystagmus, etc. While the diagnostic accuracy is poor for this test, there is still a common perception in the medical community that it is a "good" test for VBI. If you perform some manual therapy technique and the patient has a reaction and you did not perform the test, you will likely be found guilty of negligence. So perform the test. As with our normal exams, remember to screen for other potential non-musculoskeletal causes for dysfunction by assessing things like dermatomes, myotomes, reflexes, BP, pulse, respiratory rate, etc. As you can see, the upper cervical spine is not as difficult to assess as we make it out to be. Using the anatomy of the joints and our understanding of the kineseology, we can determine where/if any mobility restrictions exist. We can then proceed to couple that with our typical cervical spine assessment to find any strength/motor control limitations that contribute to dysfunction. The upper cervical spine is an important region to regularly assess due to its potential to contribute to TMJ and upper quarter dysfunctions. Any hypo/hyper-mobility can result in altered muscle tone or nerve firing patterns. These can result in altered kinematics in neighboring joints or altered joint alignments, such as an elevated 1st rib. Do not let the fear of VBI or instability prevent you from performing a complete evaluation and assessment. References:
Abernethy, Jeff. "Upper Cervical." Upper Cervical Spine Orthopaedic Residency Lecture. Scottsdale Healthcare Osborn Campus, Scottsdale, AZ. 9 January 2014. Lecture. Neumann, Donald. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation. 2nd edition. St. Louis, MO: Mosby Elsevier, 2010. 315-322. Print.  As evidence-based practice is becoming a staple in physical therapy education, it is important we properly assess each piece of research before choosing whether or not to incorporate its findings into our practice. Given the breadth of science courses that consume most of our schooling, non-clinical classes like evidence-based practice often get set aside as less important. Unfortunately, we often fail to realize the significance of search strategies, article assessments, and more when we are in the didactic portion of school. Instead, this material should really be one of the largest emphases in our programs, due to the need to stay up to date with best practice methods. With the NPTE and clinical work coming up soon, we thought it would be a great time to review some of the core components of EBP. This review is by no means exhaustive, but instead is intended to give you a foundation for further review. Question Development/Performing the Search We start with a question: background or foreground. Background questions are exactly what they sound like, in that we are searching for additional information regarding a patient's pathology or need. Foreground questions, on the other hand, are directed more towards management of the patient's problem. They often contain 4 components: -patient/client details such as age, gender, diagnosis, etc. -a specific diagnostic test, clinical measure, treatment, etc. -a comparison test, predictive factor, outcome, etc. -the consequence of interest This is frequently referred to as a PICO statement. P refers to information regarding patient details (i.e. elderly patients with RA). I refers to the intervention, diagnostic test, or whatever is being studied. C is the test, interventions, etc. to which the study is comparing (this element is not always necessary). O refers to the outcomes sought (pain scores, quality of life, strength, etc.). Now that the PICO statement is formed, we are ready to input the information from the PICO statement into the search engine. There are more than a few search engines out there, so we will only review the main features of a few of them. First, it's important to know a few components of search engines. MeSH terms are words/phrases that contain information for a pathology/treatment/etc. and allow the user to obtain information that may use different terminology for the same concept. For non-MeSH terms, it's important to included synonyms in order to expand your search. After inputting your information from the PICO statement and performing a search, check to see if MeSH terms were available for your search (if applicable). This may improve your findings. Also, not every search engine follows the same rules for boolean operators (i.e. AND/OR), so be sure to figure out how that particular one utilizes the operators. One of the most commonly used search engines is PubMed. It utilizes the above-mentioned MeSH terms and allows the user to implement limits on areas like publication date, type of study, language, etc. The Clinical Queries function allows a more tailored search for studies pertaining to etiology, diagnosis, prognosis, therapy, or CPRs. It can automatically search for the best research design. One of the most useful components of PubMed is "My NCBI." By making a (free) account with PubMed, your search parameters for a topic can be saved and routinely run. The results of any new studies that match that search are then emailed to you. This is an excellent way to stay current with new evidence! CINAHL is similar to PubMed in many areas, but it includes additional studies that do not meet PubMed's inclusion criteria. Unfortunately, CINAHL requires a subscription (and has since changed names to EBSCOHost). While this search engine does not utilize MeSH terms, it does have a vocabulary system with the same general functionality. Cochrane Library contains six databases and registries: Cochrane Reviews (systematic reviews and meta-analyses by Cochrane Collaboration), Other Reviews (systematic reviews and meta-analyses by non-Cochrane Collaboration), Clinical Trials (individual RCT performed by other investigators), Methods Studies, Technology Assesments, and Economic Evaluations. It utilizes MeSH terms, but has decreased limitation and expansion of searches functionality. PEDro is a free physical therapy-focused search engine that contains RCTs, systematic reviews, and CPRs in physical therapy. Studies are rated on a 0-10 scale based on their internal validity and statistical interpretability. Hooked on Evidence is a free database of citations for physical therapy interventions based on the pathology. Four criteria must be met to be included in this database: human subjects, at least one physical therapy intervention, at least one outcome measure of the intervention, and published in an indexed English-language peer-reviewed journal. Articles are organized according to research design type (RCTs listed first). There are other search engines out there, but these are some of the more common ones seen. Analyzing the Search Results One thing we definitely need to consider is the type of study. The research design has an impact on bias contributions, applicability to larger populations, and more. According to Jewell, the hierarchy of evidence is: -1a. Systematic Review of RCTs that do not have a statistically significant variation in the direction or degrees of results -1b. Individual RCT with a narrow confidence interval -1c. All or None Study (a study in which some or all patients died before treatment became available, now none die - think a vaccine) -2a. Systematic Review of Cohort Studies that do not have a statistically significant variation in the direction or degrees of results (cohort refers to a group of individuals followed over time that sometimes have a similar characteristic) -2b. Individual Cohort Study (including low-quality RCT) -2c. Outcomes Research -3a. Systematic Review of Case-Control Studies that do not have a statistically significant variation in the direction or degrees of results (a retrospective approach when subjects known to have the outcome are compared to those without) -3b. Individual Case-Control Study -4. Case-Series Study; Cohort or Case-Control Study that did not: define comparison groups adequately or did not measure exposures and outcomes objectively or in a blinded fashion or control for confounders or have sufficient follow-up -5. Expert Opinion without explicit critical appraisal, or based on physiology, bench research or "first principles" While this hierarchy can aide in selection of evidence, we should still read and fully evaluate articles before implementing them into practice. The reason is because a high-level article, such as a systematic review, may have included poor methods: ignoring confounding variables, limited blinding, poor experience of clinicians, etc. There are many items to consider when reviewing evidence. One place that can sometimes be good to start is a literature review, because it often reviews the research up until that point of time. Things to look out for, however, include evidence being judged by date of publication, flow of article, and relation between articles selected and review topic. Each can potentially lead to eliminating useful information. Older studies may still have the best quality of evidence. Sometimes seemingly unrelated articles contain information that is actually very connected to the study. Another quality of studies not mentioned was a meta-analysis. Systematic reviews with meta-analysis incorporate summaries of the primary studies that are critically appraised and statistically combined. The result is an even higher level of evidence. Research design refers to how the study is carried out. In experimental studies, some of the subjects are manipulated with a treatment/intervention (independent variable) in order to study the effect (dependent variable). Experimental studies can have 3 variations for the control group: no treatment, placebo, or both groups get standard treatment but experimental group gets additional interventions. Quasi-experimental studies are similar in that they involve manipulation again, but either lack a second group for comparison or random assignment. There are a few methods for quasi-experimental studies: time series format (repeated measures collected over time before/after experimental intervention is introduced to a single group), non-equivalent group (similar to experimental but no random assignment), single system (one subject undergoes experimental treatment and control treatment periods in alternating fashion), and a few others. In single-system/subject designs, some common methods are A-B, A-B-A, and A-B-A-B formats. "A" refers to baseline and "B" refers to treatment. Non-experimental studies obviously are purely observational. A within-subjects study occurs when the outcome is repeatedly measured in a single group of subjects. Between-subjects refers to outcomes being compared between 2+ groups. Bias can occur in a variety of points in a study: subject recruitment/assignment/communication, calibration/use of equipment, maintenance of environmental condition, and more. It can be minimized with random assignment of subjects and masking of subjects and investigators (if both are blinded, it is referred to as a double-blind study). You may notice some time descriptors for studies as well. Cross-sectional refers to data being collected once during a single point in time. Longitudinal refers to repeated measures over an extended period of time. Retrospective is historical and obviously lacks randomization. Prospective is data being collected in real time. There are many other factors to consider when analyzing the methodological quality of evidence. Inclusion/exclusion criteria can render an otherwise well-performed study useless. We recently did a review of the Joint Line Fullness Test for meniscal injuries. While the results of the study looked promising, the researchers exluded any patients with an acute injury (within 6 weeks of exam) or presence of osteophytes, joint space loss, or arthritis. These are typically the types of patients we see in the clinic, so it doesn't really matter how accurate the test is in other conditions. We should also take note as to whether or not the inclusion/exclusion criteria is even appropriate based on the clinical question. Look at to see if participants were lost during the study (attrition), why they were lost, and if any adjustments were made in the statistical analysis. Consider how many databases/resources were used for the study. After reviewing the various search engines, it should be evident that one database doesn't contain all the information. In systematic reviews, the number of individuals reviewing research studies (and whether or not they were blinded) may impact their findings.
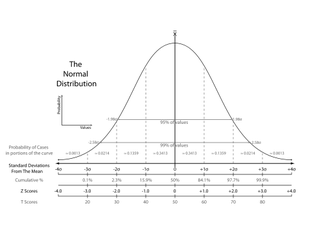
Many experimental studies start off with a null hypothesis that is the common understanding at the time (therapeutic exercise = therapeutic exercise + manual therapy). The researchers develop an alternative hypothesis to challenge what is currently accepted (therapeutic exercise < therapeutic exercise + manual therapy). Tests of significance can be used to determine if any differences found in the groups are true or are due to chance. If they are true, then they may be applicable to the population. The alpha level is first set to determine the level of probability that results are not due to chance. The most common ones are .05 or .01. If the p-value is below these, there is a 5% chance that the differences in the study were due to chance (alpha level 5). Results that are "statistically significant" represent heterogeneity. If there is overlap of confidence intervals or the p-value is not below the alpha level, homogeneity is present. As with any study, there lies the risk of error at some point during the process. Type I error refers to the null hypothesis being rejected when it shouldn't have been. Type II error occurs when the null hypothesis should have been rejected when it wasn't. A t-test can be used to compare 2 different groups. It can be either one-tailed or two-tailed. One-tailed only assess one end of the population distribution. Two-tailed assesses both ends. Any time more than 3 groups need to be assessed for variance, ANOVA (analysis of variance) should be utilized. Simple ANOVAs compare only 1 variable between groups, while factorial ANOVAs compare multiple variables between groups. ANCOVA compares multiple treatment groups, while controlling for any other variables that might affect the results. T-tests, ANOVAs, and ANCOVAs are referred to as parametric tests in that they are based on the population. The calculations result in the previously described p-value to determine if the findings are statistically significant. For non-parametric tests, we can use the Chi square test. It compares actual frequencies to expected and is followed up with a p-value to again determine the likelihood that the results are true, instead of being due to chance. Some values that are regularly reported for examination techniques include sensitivity, specificity, positive/negative likelihood ratios and positive/negative predictive values. Sensitivity refers to a test's ability to accurately rule out a disease and is scored between 0 and 1.00. Tests with high Sensitivity, rule Out a disease (SnOut). Specificity refers to a test's ability to accurately rule in a disease and is scored between 0 and 1.00. Tests with high Specificity, rule In a disease (SpIn). Positive and negative likelihood ratios work in a similar way but are not limited to numbers between 0 and 1.00. They act more as "persuasive information" and are more individualized than sensitivity and specificity(Jewell, 2010). Clinicians are required to determine a patient's pretest probability, then incorporate the likelihood ratio for the test and determine how "likely" the patient has the pathology. Predictive values are used to determine the true positives (or negatives) out of those that tested positive (or negative), both true and false. Another common statistic we'll see is correlational research. These studies look to see how well two variables are related to each other; they do not signify causation. The numbers are expressed between -1.00 to 1.00. When near zero, there is a low correlation/relationship. When near 1.00 or -1.00 there is a strong relationship. Positive refers to direct correlations, while negative refers to inverse correlations. This may be referred to as "Pearson's r" for two groups or "Intraclass Correlation Coefficient (ICC)"6 for 3 or more groups. These values can be used to assess the reliability of examination techniques as well. Intra-rater reliability refers to the ability of an individual to consistently obtain the same findings given the same variables. Inter-rater reliability refers to the ability of different individuals to obtain the same findings given the same variables. As you can see there is a lot to remember when it comes to appraising evidence. Hopefully, you found this review useful for a foundation in your studies and the practice of utilizing evidence, but this does not by any means encompass everything. If you need further information for statistical analyses and research design, we recommend reviewing your notes and text books. Most of the information discussed in this review is from Jewell's Guide to Evidence-Based Physical Therapist Practice. Reference:
Jewell, Dianne. Guide to Evidence-Based Physical Therapist Practice. Sudbury, MA: Jones & Bartlett Learning 2011. Print. |
Copyright © The Student Physical Therapist LLC 2023



 RSS Feed
RSS Feed