- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
I recently gave a lecture, regarding adverse neural tissue tension (ANTT). With frequency of our nervous system contributing to pain, mobility/strength impairments, and overall functional deficits, I thought it would be an excellent topic to review. One of the recurring themes I talked about was how musculoskeletal injuries typically have a short time-frame for pain. Prolonged and residual pain can be secondary to neural tension and underlying non-painful neural tension can increase the likelihood of a distal entrapment. The message is that we should always assess the neural system in our examinations as a potential contributing factor. If you have any questions, don't hesitate to ask. -Chris
0 Comments
Recently, I had the opportunity to present a lecture to some first year PT students on the TMJ. I have attached the presentation below. The lecture focused primarily on biomechanics of the TMJ with basic testing of the region as well, including ROM, resisted isometrics, MMT, and a few special tests. For a little additional information, check out a quick review I did several months ago. If you have any questions, feel free to ask! -Chris  I recently read a post about how manual therapy does not really require "skill." Initially, I found the post somewhat infuriating as I have been making my way through a residency that is heavy in manual therapy. However, after reading some of the articles referenced on the post and after following The Manual Therapist blog for awhile, I realized that the popular theories behind the effectiveness of manual therapy may not be as accurate as I thought. That doesn't mean manual therapy isn't effective, but that it may have a different mechanism. This inspired me to do a review on the literature from this alternative perspective. Soft Tissue Mobilization There are various soft tissue techniques (Graston Technique, ASTYM, trigger point release, etc.) that are based on the theory of collagen deformation. Although largely based on theoretical and mathematical models, studies have shown that it requires greater forces than human ability can apply to deform fascial tissue even 1% (Chaudhry et al, 2008). This may be difficult to accept for some therapists, as many will claim feeling a tissue "release" with overpressure. However, it has been shown that the manual pressure applied by therapists actually stimulates mechanical receptors in the tissue, which lowers sympathetic tone in the tissue and a "release" of the adhesion (Schleip, 2003). Again, that doesn't mean the techniques performed don't work, just that they don't work based on the theorized mechanism. This is advantageous to understand as it may alter our technique choice and how we implement it. I have training in IASTM (Instrument-Assisted Soft Tissue Mobilization) based on this neurological effect. Why perform a technique that may injure a patient via bruising, or worse, when we can be as, or more, effective doing something less invasive? Stretching Stretching is a treatment technique that has been a foundation of physical therapy for decades. Quite a bit of research has been done on the topic. In school, the standard practice is that 30 seconds of static stretching is required to get plastic deformation on tissues. But does this actually occur? Without a doubt, it would appear that people can "stretch" their muscles further after a designed stretching program. There are many theories as to how this happens: viscoelastic deformation, plastic deformation of connective tissues, increased sarcomeres in series, and neuromuscular relaxation (Weppler & Magnusson, 2010). However, there appears to be insufficient evidence for each of these areas. With regards to the viscoelastic model, studies have shown that the changes that do occur are small and have short duration. No evidence has been found for true plastic (or permanent) deformation of muscle tissue via stretching. Many report that prolonged immobilization results in altered numbers of sarcomeres in series - on a stretch they increase in series and in a contracted position they decrease. These studies have been inappropriately applied to static stretches. In fact, it was found that after removal of the immobilization, the sarcomere number go back to the original amount. What is often ignored is that these studies are performed on animal muscle tissue by themselves. We do not truly know how sarcomere react in series to stretching in conjunction with tendons, other fascial structures, skin, etc. This is an important component as that is how the body truly functions and we cannot separate out muscle from those other structures when stretching. The neuromuscular relaxation theory is based on altering the stretch reflex to allow a muscle to relax (and thus "stretch") further. Studies have been unable to prove this theory valid with no alterations in the EMG activity of the stretched muscles. In fact, regular stretching was shown to have no significant change on joint mobility, pain, spasticity, or functional limitations in those with neurological conditions (Katalinic et al, 2011). An alternative theory that is presented is changes in muscle length are actually due to a change in perception of stretch (Weppler & Magnusson, 2010). There has been limited evidence to support this theory, but it is based upon a study that showed an increase in end-range joint angle with no change in applied force and no permanent change in length (no plastic deformation). The end-range joint position was based upon subjective sensation of a "stretch." Mobilization and Manipulation With my residency training, a significant amount of time and effort was placed into trying to isolate and locate a specific hypomobile segment to treat. Needless to say, I became somewhat defensive when I heard there was little support for being so specific. Studies have shown that there is no greater benefit for manipulation of a targeted (hypomobile/painful accessory motion based on examiner assessment) joint manipulation compared to a non-specific joint manipulation (Chiradejnant et al, 2003) (Aquino et al, 2009) (Schomacher 2009) (Nyberg & Russell Smith, 2013). However, each of the studies had limitations: chronic pain, potential patient population bias, etc. These findings lend support to the clinical prediction rules that are not specific in nature and may suggest another sign of potential neurological impact and basis for our manual therapy techniques. What exactly happens with a manipulation is difficult to understand. I remember being taught that the cavitation heard is a result of the fluid in the joint capsule quickly evaporating due to the expanded volume of the capsule (and fixed fluid) as a result of the thrust. Whether or not these capsular changes are maintained over time, or even occur, is lacking in evidence. That doesn't mean manual therapy isn't useful. Clinical predictions rules have been developed for patients with neck or low back pain that would benefit from a manipulation (Cleland et al, 2007) (Puentedura et al, 2012). There are those that suggest a mobilization can be as effective as a manipulation, with the only benefit being a manipulaiton can accomplish the same result in less time, but some research shows manipulations may actually be superior. Manipulations have been shown to have a greater effect on ROM, pain, disability and muscle performance compared to non-thrust mobilizations (Dunning JR et al, 2010). Manipulations to the thoracic spine were shown to have a more significant effect on neck pain than mobilizations. (Cleland et al, 2007). With the risk for injury to various structures in the cervical spine, many are hesitant to even consider a grade V thrust to the area. The only reason it is worth considering is that cervical manipulations had a greater effect than thoracic manipulations on neck pain (Puentedura et al, 2011). It is worth noting that with any manipulation or mobilization, we must carefully screen our patients for contraindications such as osteoporosis, RA, chronic steroid use, etc. Conclusion In summary, the results we get from our manual techniques may not be due to the theories on which we were trained, but that does not mean it isn't skilled. A level of clinical reasoning is beneficial to understanding how and why manual therapy treatments can be applied. Manipulations and mobilizations may not be as specific as we thought, but a certain level of training typically is required to be able to perform. But why do those changes occur? While the current popular theories of various manual therapy techniques may have the positive impact we desired, they may not be accurate. This is worth discussion and further investigation to make our treatments as effective as possible. Why injure our patients with certain manual therapy treatments when this can be avoided? Some evidence suggests that we may alter neuromuscular perception by activating mechanoreceptors. While this is not concrete evidence, it may be worthy a topic of research in the future and may play a role in how we can be most effective with our treatments. -Chris References:
Aquino RL, Caires PM, Furtado FC, Loureiro AV, Ferreira PH, & Ferreira ML. (2009). Applying Joint Mobilization at Different Cervical Vertebral Levels Does Not Influence Immediate Pain Reduction in Patients with Chronic Neck Pain: A Randomized Clinical Trial. Journal of Manual & Manipulative Therapy. 2009 April;17(2): 95-100. Chaudhry H, Schleip R, Ji Z, Bukiet B, Maney M, & Findley T. (2008). Three-Dimensional Mathematical Model for Deformation of Human Fasciae in Manual Therapy. Journal of American Osteopathic Medicine. 2008 Aug; 108(8):379-390. Chiradejnant A, Maher CG, Latimer J, & Stepkovitch N. (2003). Efficacy of "Therapist-Selected" Versus "Randomly-Selected" Mobilisation Techniques for the Treatment of Low Back Pain: A Randomised Controlled Trial. Australian Journal of Physiotherapy. 2003; 49(4):233-241. Cleland JA, Childs JD, Fritz JM, Whitman JM, & Eberhart SL. (2007). Development of a Clinical Prediction Rule for Guiding Treatment of a Subgroup of Patients with Neck Pain: Use of Thoracic Spine Manipulation, Exercise, and Patient Education. Physical Therapy. 2007 January;87(1):9-23. Cleland JA, Glynn P, , Whitman JM, Eberhart SL, MacDonald C, & Childs JD. (2007). Short-Term Effects of Thrust Versus Non-Thrust Mobilization/Manipulation Directed at the Thoracic Spine in Patients with Neck Pain: A Randomized Clinical Trial. Physical Therapy. 2007 April;87(4):431-440. Dunning JR, Cleland JA, Waldrop MA, Arnot C, Young I, Turner M, & Sigurdsson G. (2010). Upper Cervical and Upper Thoracic Thrust Manipulation vs Non-Thrust Mobilization in Patients with Mechanical Neck Pain: A Randomized Controlled Trial. Journal of Manual & Manipulative Therapy. 2010 December;18(4):175-180. Katalinic OM, Harvey LA, & Herbert RD. (2011). Effectiveness of Stretch in the Treatment and Prevention of Contractures in People with Neurological Conditions: A Systematic Review. Physical Therapy. 2011. Jan;91(1): 11-24. Nyberg RE & Russell Smith A. (2013). The Science of Spinal Motion Palpation: A Review and Update with Implications for Assessment and Intervention. Journal of Manual & Manipulative Therapy. 2013 Aug;21(3):160-167. Puentedura EJ, Cleland JA, Landers MR, Mintken P, Louw A, & Fernandez-de-las-penas C. (2012). Development of a Clinical Prediction Rule to Identify Patients with Neck Pain Likely to Benefit from Thrust Joint Manipulation to the Cervical Spine. JOSPT. 2012 July;42(7):577-592. Puentedura EJ, Landers MR, Cleland JA, Mintken P, Huijbregts P, & Fernandez-de-las-penas C. (2011). Thoracic Spine Thrust Manipulation Versus Cervical Spine Thrust Manipulation in Patients with Acute Neck Pain: A Randomized Clinical Trial. JOSPT. 2011 April;41(4). Schleip R. (2003). Fascial Plasticity - A New Neurobiological Explanation: Part 1. Journal of Bodywork and Movement Therapies. 2003 Jan;7(1):11-19. Schomacher J. (2009). The Effect of an Analgesic Mobilization Technique when Applied at Symptomatic or Asymptomatic Levels of the Cervical Spine in Subjects with Neck Pain: A Randomized Controlled Trial. Journal of Manual & Manipulative Therapy. 2009 April;17(2): 101-108. Weppler CH & Magnusson SP. (2010). Increasing Muscle Extensibility: A Matter of Increasing Length or Modifying Sensation? Physical Therapy. 2010 March;90(3): 438-449. Cervical spine pain is one of the more common complaints seen in outpatient orthopaedic physical therapy. With the relation to the rest of the upper quarter, the shoulder and thoracic spine, it is essential we be as proficient as possible when assessing and treating the region. While this may seem obvious, it is interesting to note how hesitant some clinicians are in treating the upper cervical spine. Why? Because it is different and there is risk for fatal injury. The upper cervical spine is made up of the Atlantooccipital Joint and the Atlantoaxis Joint. These joints have different anatomical and kinesiological considerations compared to the rest of the cervical spine. With the frequency with which the cervical spine is involved in upper quarter dysfunction, as well as temporomandibular dysfunction, it is imperative we have a solid understanding of the joints. 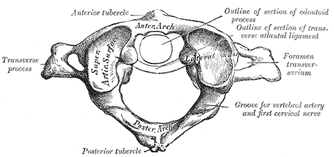 Atlantooccipital Joint The Atlantooccipital Joint (AO) is made up of the atlas and occiput. The atlas has no body, pedicles, laminae, or spinous process, unlike typical vertebrae. There is an anterior arch with an anterior tubercle for attachment of the anterior atlanto-occipital membrane (Neumann, 2010). The posterior arch is larger and has a posterior tubercle. Additionally, there are two large transverse processes that are palpable between the mastoid process and mandibular ramus. There are two large concave facets that face medially and superiorly in order to accept the occipital convex condyles that face inferiorly and laterally (Abernethy, 2014). The atlanto-occipital membrane connects the anterior portion of the foramen magnum to the anterior arch of C1 for anterior-posterior stability. The posterior atlanto-occipital ligament connects the posterior ring of C1 to the occiput at the foramen magnum as well. This ligament is important for anterior translation of C1 and vertical translation of the occiput. Additionally, there are joint capsules surrounding the AO joints that limit movement in each direction. There are 2 degrees of freedom in the AO joint: flexion/extension and frontal sidebend (Abernethy, 2014). The OA joint is responsible for 10 degrees of flexion, 25 degrees of extension, 5 degrees of sidebend, and 4 degrees of conjugate rotation. To fully comprehend the arthrokinematics of the AO joint, we must know the plane of the joint. During flexion, there is a bilateral lateral, posterior, and superior (LPS) motion, while there is a bilateral medial, inferior, and anterior motion for extension (MIA). In order to determine which part and which side of the joint is restricted, we assess sidebend. Upper cervical sidebend to the left, results in left AO MIA and right AO LPS. In other words, if you sidebend the upper cervical spine to the left, you are essentially flexing on the right and extending on the left. To determine which side is at fault for the motion restrictions, sidebending should be reassessed in flexion and extension. For example, if sidebending to the left feels restricted in neutral, it is possible that either flexion on the right or extension on the left (or both) are limited. In a normal joint, sidbending should be smooth and through an axis that runs through the tip of the nose. When placed in flexion (of the same restricted motion), sidebend to the left now biases the right joint. By initially placing the AO joints in flexion, the condyles are moved lateral, posterior and superiorly (LPS). Thus, if there is a restriction on that right side, the condyle will meet its barrier sooner compared to neutral. By placing the AO joints in extension, the condyles are then moved medially, inferiorly, anteriorly (LIPS). This forces the condyle on the left to meet its barrier sooner compared to neutral if there is a restriction. Typically, a flexion limitation is found due to the frequency with which we see forward head posture. If you find an extension limitation, I recommend re-checking the joints.
The axis of rotation is through the dens. When rotating to the left, the ipsilateral side of the atlas glides posteriorly, while the contralateral side glides anteriorly (Abernethy, 2014). The AA joint is responsible for 35 degrees of rotation bilaterally, 8 degrees of flexion, and 10 degrees of extension. There are two methods that are commonly used for assessing motion at the AA joint. One is the Flexion-Rotation Test, where the cervical spine is maximally flexed (and maintained there), while rotation is performed bilaterally. The issue with this test is that it tends to also include motion at the C2-3 joint, resulting in at least 45 degrees of rotation in a normal joint bilaterally. To truly assess AA rotation, maximally sidebend the cervical spine ipsilaterally and rotate contralaterally, while maintaining chin tuck (if chin tuck is lost, isolation to C1-2 is lost). This is also a position for manipulation. It should be noted that in those with moderate degeneration of the cervical spine (and presents of significant osteophytes), cervical sidebend may be limited, resulting in decreased ability to isolate the AA joint. Ligament and Artery Testing People are often wary of treating upper cervical dysfunction manually due to some of the potential risks for fatal injury. The cervical vertebrae house the spinal cord and vertebral arteries - structures that are necessary for ordinary brain and motor function. Therefore, we must assess two areas: stability and blood flow. It is recommended that stability is assessed first due to the end range positions required for vertebral artery testing. The two ligament tests required are the Transverse Ligament Test and the Alar Ligament Test. The transverse ligament runs from one side of the arch of C1 wrapping around the dens to the other side of the arch of C1 (Abernethy, 2014). This ligament is 7-8 mm thick and keeps the dens in contact with the atlas, preventing anterior dislocation. The alar ligaments run superiorly and laterally from the dens to the occiput, resisting posteiror translation of the dens and occipital rotation contralaterally. If any of the tests are positive, a provocation of neural symptoms may occur. Structural stability of the atlas may also be assessed by compressing the transverse processes of C1 medially at the same time. If movement is detected, there lies the possibility of a Jefferson fracture. This often occurs with an axial blow to the head. Once instability has been cleared, we must check the patency of the vertebral arteries, as the vetebrobasilar system is responsible for 11% of blood flow. The vertebral artery branches off the subclavian and passes superiorly with the longis colli, enters the transverse foramen usually at C6 (but anywhere between C4-7), wraps back around the articular pillar and enters the posterior AO membrane, before entering through the foramen magnum. Here it joins the opposite vertebral artery to form the basilar artery. Vertebrobasilar Insufficiency is assessed with the Vertebral Artery Test. If you look at the diagnostic accuracy of the test, it would appear there isn't really a reason to even perform the test. With a sensitivity of 0% and a specificity of .67-.9%, a negative test means absolutely nothing and a positive test means the patient may have vertebrobasilar insufficiency. Positive symptoms include: dizziness, diplopia, dysarthria, dysphagia, drop attacks, nausea and vomiting, sensory changes, nystagmus, etc. While the diagnostic accuracy is poor for this test, there is still a common perception in the medical community that it is a "good" test for VBI. If you perform some manual therapy technique and the patient has a reaction and you did not perform the test, you will likely be found guilty of negligence. So perform the test. As with our normal exams, remember to screen for other potential non-musculoskeletal causes for dysfunction by assessing things like dermatomes, myotomes, reflexes, BP, pulse, respiratory rate, etc. As you can see, the upper cervical spine is not as difficult to assess as we make it out to be. Using the anatomy of the joints and our understanding of the kineseology, we can determine where/if any mobility restrictions exist. We can then proceed to couple that with our typical cervical spine assessment to find any strength/motor control limitations that contribute to dysfunction. The upper cervical spine is an important region to regularly assess due to its potential to contribute to TMJ and upper quarter dysfunctions. Any hypo/hyper-mobility can result in altered muscle tone or nerve firing patterns. These can result in altered kinematics in neighboring joints or altered joint alignments, such as an elevated 1st rib. Do not let the fear of VBI or instability prevent you from performing a complete evaluation and assessment. References:
Abernethy, Jeff. "Upper Cervical." Upper Cervical Spine Orthopaedic Residency Lecture. Scottsdale Healthcare Osborn Campus, Scottsdale, AZ. 9 January 2014. Lecture. Neumann, Donald. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation. 2nd edition. St. Louis, MO: Mosby Elsevier, 2010. 315-322. Print.
Anatomy: One of the first things to remember is that the thoracic spine is comprised of 12 vertebrae. These vertebrae have similar characteristics of the other vertebrae: a vertebral body (disk to vertebral body height ratio is 1:5), pedicles directed posterior from the body, lamina that connect to form a spinous process, and facets (Neumann, 2010). The transverse processes are directed posterolaterally and the spinous processes fall inferiorly (depending on the region), so that they are at the level of the transverse processes below. This is an important consideration for palpation. T1-3 and T10-12 actually have their spinous processes at the same level as the transverse processes (Egan et al, 2011). The spinous processes of T4-T6 fall half a level below the transverse processes, while T7-9 spinous processes fall a full level below the transverse processes. The pedicles actually sit directly posterior from the vertebral body, making the vertebral canal narrower here compared to other parts of the spine. T4-9 is known as the critical zone because the vertebral canal is narrowest here; it also has reduced blood supply (Egan et al, 2011). T6 is a tension point; here motion of the spinal core versus canal converge in different directions. The superior and inferior facets in the thoracic region are oriented about 60 degrees from the horizontal plane and 20 degrees from the frontal plane with the inferior facets facing anteriorly, inferiorly, and slightly medially; the superior facets face posteriorly, superiorly, and slightly lateral. Something to consider is that there is no immediate change between cervical to thoracic vertebrae and thoracic to lumbar vertebrae. The superior thoracic vertebrae bare qualities similar to the cervical spine and the inferior thoracic vertebrae resemble the lumbar spine.  Ribs: You cannot discuss the thoracic spine without considering the ribs as they attach in this region. There are 12 ribs (usually) in the body, just as there are 12 thoracic vertebrae. Ribs 1-7 are true ribs in that they attach directly to the sternum in the front of the body (Neumann, 2010). Ribs 8-12 are false ribs. Ribs 8-10 join in cartilage before attaching to the cartilage of the 7th rib. Ribs 11 and 12 are floating ribs and have no ventral attachments. Ribs 3-9 have demifacets on the thoracic vertebrae for attachment that span 2 vertebrae. Ribs 1, 11, and 12 have one facet on the corresponding vertebrae. The 2nd rib attaches to both T1 and T2 vertebrae. Additionally, ribs 1-10 have facet attachments at the costotransverse joints, while ribs 11-12 lack these as "floating ribs." Above T7, the rib portion of the costotransverse joints are concave, allowing for more rotation compared to the planar joints of the below T7 (Egan et al, 2011). The sympathetic chain lies on the anterior side of the rib heads next to the costovertebral joints. Clinical Implications: As stated previously, the fact that the thoracic spine connects the cervical spine to the lumbar spine is reason alone that this anatomical area should be considered for treatment. Think about the impact of posture. In most patients that sit for prolonged periods with a forward head posture, the anterior shift of the center of gravity places an excessive flexion moment arm to the thoracic spine, furthering the already kyphotic thoracic spine. As with any tissue, prolonged stress and creep eventually leads to pain when the tensile stiffness is no longer sufficient and the patient experiences pain. Training postural muscles is key to encouraging a more neutral posture that does not stress the tissues excessively. Consider facet restrictions: Limited joint mobility in one location often leads to hypermobility and pain in other regions, either nearby or distant. A joint dysfunction can often lead to hypertonic/painful muscle tissue near the joint as well. We can treat these restrictions with manual therapy. Two conditions less commonly discussed but seen relatively often include rib dysfunction and neural tension. Rib impairments are typically considered after a blow to the side or pain with breathing, but that is not always the case (making it harder to identify). A partially subluxed or restricted rib can be quite painful and present as thoracic paraspinal pain or even stomach pain as the tip of a floating rib presses against the anterior tissue. A potential location for pathology and treatment of neural tension is the thoracic spine. Remember that the thoracic spine contains the critical zone where the vertebral canal is narrowest. The spinal cord can easily become compressed here leading to pain/neural tension along the path of a nerve. A nerve can become irritated anywhere in the body. With the thoracic restrictions, a manipulation to the mid-thoracic spine often improves pain and neural tension by improving mobility. Think of it as a reset button as it also may have an impact on the sympathetic nervous system. References:
Egan W, Burns S, Flynn T, and Ojha H. The Thoracic Spine and Rib Cage: Physical Therapy Patient Management Utilizing Current Evidence. Current Concepts of Orthopaedic Physical Therapy, 3rd Ed. La Crosse, WI. 2011. Neumann, Donald. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation. 2nd edition. St. Louis, MO: Mosby Elsevier, 2010. 322-323. Print.  Bioenergics can be defined as "the flow of energy in a biological system, and it concerns primarily the conversion of macronutrients into biologically usable forms of energy." In other words, it is how our body utilizes energy. There are 3 main energy systems available: the phosphagen system, glycolysis, and the oxidative system. Based on the needs of a specific activity (aerobic, anaerobic, or mixed), our body selects which energy systems are required for the activity. The contribution of each system is dependent on the intensity and duration of the activity at hand. With specific exercise, each system can become more efficient and effective for a specific activity. It is for this reason, that physical therapists must understand these systems in relationship to intervention selection, dietary requirements, amount of rest, specific injury, and more to best return your client to their prior level of function (or even higher!). Part 1 is going to provide you with the background information on the physiology of each of these systems. 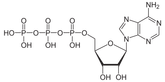 Back to the Basics The energy required to perform any physical activity will either come from 1 of 2 metabolic sources: aerobic or anaerobic systems. In short, the anaerobic system is used for quick, higher intensity activities, and the aerobic system is used during longer, lower intensities activities. The energy required for us to live comes from macronutrients: carbohydrates, proteins, and fats. Each macronutrient is broken down into a measurable metabolic unit known as ATP or adenosine triphosphate. The molecule adenosine is made of adenine (a nitrogen-containing base) and ribose, a 5-carbon sugar. Triphosphate refers to 3 phosphates that are attached. In order to acquire energy from ATP, water must be involved for hydrolysis of the molecule by adenosine triphosphatase (ATPase). So basically, energy is released when a phosphate is broken off of ATP (or ADP). The turnover rate and resynthesis of ATP depends on the intensity and duration of exercise.  The Phosphagen System Regardless of the duration and intensity of exercise (whether sprinting 100m or running a mile), the phosphagen system is always activated at the start of exercise. Energy is derived from the previously mentioned hydrolysis of ATP and breakdown of creatine phosphate (CP). When creatine phosphate is broken down, the phosphate combines with ADP to form ATP, providing another unit of energy to be used. As you can see, ATP truly is the currency of energy. Other sources, such as CP, must be converted to ATP before they can fully be utilized. The body regularly holds about 80-100g of ATP. During exercise, levels may decrease only up to around 50%, so that energy for basic cell function can be maintained. This means as ATP is used by the body, it is being converted from other sources (such as CP or the energy stores yet to be discussed) to maintain the body's normal levels. Levels of CP in the body are usually about 4-6x higher than that of ATP. The greater the amount of Type II fibers in the body, the greater the CP storage, due to Type II fibers higher concentrations of CP. With individuals who perform brief high intensity exercise, it would make sense that they want to increase their Type II fibers, so they can have more energy for that specific activity. Unfortunately, CP is stored in small amounts and used up rapidly by the body. Phospagen stores are depleted anywhere from 1-15 (Wells 2009) seconds before the body enters glycolysis. Glycolysis The next energy system in the line-up is glycolysis, the breakdown of carbohydrates from either glycogen in the muscle or glucose in the blood. Like CP, glycolysis' function is to create and maintain the body's normal levels of ATP. Glycolysis requires increased time to form ATP compared to CP, but it does create greater amounts. Depending on the presence of oxygen, the pyruvate either is converted to lactate or goes into the mitochondria to begin the oxidative system. If oxygen is absent and lactate forms, ATP formation speed is improved, but the amount is decreased compared to if oxygen were present. This is known as anaerobic or fast glycolysis. When oxygen is present, the pyruvate enters the Krebs cycle. This aerobic (or slow) glycolysis can last for prolonged periods, as long as the exercise intensity is low enough. If it's too high, the body relies on anaerobic means. Lactate is often incorrectly blamed as the cause of fatigue (metabolic acidosis as a result of elevated hydrogen ion concentrations is linked to peripheral fatigue), but it does play an important role in these energy systems. It is used as an energy substrate by type I and cardiac muscle fibers. If lactate is instead transferred to the liver, it undergoes gluconeogenesis (conversion to glucose) in the Cori cycle. In fact, lactate is produced regularly, even at rest. In aerobic situations, the lactate is usually oxidized by other tissues or converted to glucose or amino acids. Clearance of lactate can be increased by light activity after exercise. Depending on the source of glucose, glycolysis may have different ATP products. One molecule of blood glucose nets 2 ATP molecules, while muscle glycogen nets 3 ATP molecules. The difference is that blood glucose requires an additional ATP molecule to remain in its available state for energy usage. Going back to aerobic glycolysis, the pyruvate is actually transformed to Acetyl-CoA, so that it can enter the Krebs cycle. Glycolysis, like the previous system, is stimulated by elevated ADP, P, ammonia, and a decrease in pH and AMP. The opposite inhibits glycolysis. An important regulator of glycolysis is the phosphofructokinase (PFK) enzyme. With elevated ATP, PFK limits glycolysis. As lactate begins to accumulate in the bloodstream, the sudden increase is known as the lactate threshold. It corresponds well with the ventilatory threshold as well - the point at which ventilation no longer is associated with oxygen consumption (VO2). The point at which lactate threshold occurs compared to % VO2max increases with training. A second increase in lactate levels in the bloodstream is known as onset of blood lactate accumulation (OBLA). Oxidative System Following aerobic glycolysis, the products enter the oxidative system. This is the energy system primarily used at rest and low intensity exercise. At rest fat is the primary source of ATP development. As exercise begins, carbohydrates become the more significant factor; however, if the exercise is prolonged with low-intensity, fats and proteins become the source of ATP development yet again. It's important to note that even when fats are the primary energy source, it is essential that a level of carbohydrates be available as well for efficient fat processing. Without adequate carbohydrate levels to facilitate the fat breakdown, it becomes much more difficult to utilize a fat for its full potential and the body is forced to breakdown protein even more. Now for a look at the cellular level of this process. Following glycolysis, the pyruvate enters the mitochondria and begins the Krebs cycle, where 2 ATP are produced for each molecule of glucose. In addition, several transport molecules (NADH and FADH2) are produced here that bring hydrogen atoms to the electron transport chain. This is where ADP becomes ATP. Oxidative phosphorylation, from the beginning of glycolysis to the end of the electron transport chain, produces 38-39 ATP. As you can see, this method produces the greatest amount of energy! This is a very basic summary of bioenergenics, with most of the information coming from the resources listed below. Energy utilization can be broken down into much greater detail, but is beyond the purpose of this discussion. For more information about this subject, check out the sources listed below or your exercise physiology text books. Next post will discuss how we can utilize this information in designing our training programs! References:
Baechle T & Earle R. The Essentials of Strength and Conditioning: 3rd Edition. National Strength and Conditioning Association: Human Kinetics 2008. Print. Wells G., Selvadurai H, and Tein I. (2009). Bioenergic provision of energy for muscular activity. Paediatric Respiratory Reviews. 2009; 10: 83-90. Web. 11 July 2013.  As evidence-based practice is becoming a staple in physical therapy education, it is important we properly assess each piece of research before choosing whether or not to incorporate its findings into our practice. Given the breadth of science courses that consume most of our schooling, non-clinical classes like evidence-based practice often get set aside as less important. Unfortunately, we often fail to realize the significance of search strategies, article assessments, and more when we are in the didactic portion of school. Instead, this material should really be one of the largest emphases in our programs, due to the need to stay up to date with best practice methods. With the NPTE and clinical work coming up soon, we thought it would be a great time to review some of the core components of EBP. This review is by no means exhaustive, but instead is intended to give you a foundation for further review. Question Development/Performing the Search We start with a question: background or foreground. Background questions are exactly what they sound like, in that we are searching for additional information regarding a patient's pathology or need. Foreground questions, on the other hand, are directed more towards management of the patient's problem. They often contain 4 components: -patient/client details such as age, gender, diagnosis, etc. -a specific diagnostic test, clinical measure, treatment, etc. -a comparison test, predictive factor, outcome, etc. -the consequence of interest This is frequently referred to as a PICO statement. P refers to information regarding patient details (i.e. elderly patients with RA). I refers to the intervention, diagnostic test, or whatever is being studied. C is the test, interventions, etc. to which the study is comparing (this element is not always necessary). O refers to the outcomes sought (pain scores, quality of life, strength, etc.). Now that the PICO statement is formed, we are ready to input the information from the PICO statement into the search engine. There are more than a few search engines out there, so we will only review the main features of a few of them. First, it's important to know a few components of search engines. MeSH terms are words/phrases that contain information for a pathology/treatment/etc. and allow the user to obtain information that may use different terminology for the same concept. For non-MeSH terms, it's important to included synonyms in order to expand your search. After inputting your information from the PICO statement and performing a search, check to see if MeSH terms were available for your search (if applicable). This may improve your findings. Also, not every search engine follows the same rules for boolean operators (i.e. AND/OR), so be sure to figure out how that particular one utilizes the operators. One of the most commonly used search engines is PubMed. It utilizes the above-mentioned MeSH terms and allows the user to implement limits on areas like publication date, type of study, language, etc. The Clinical Queries function allows a more tailored search for studies pertaining to etiology, diagnosis, prognosis, therapy, or CPRs. It can automatically search for the best research design. One of the most useful components of PubMed is "My NCBI." By making a (free) account with PubMed, your search parameters for a topic can be saved and routinely run. The results of any new studies that match that search are then emailed to you. This is an excellent way to stay current with new evidence! CINAHL is similar to PubMed in many areas, but it includes additional studies that do not meet PubMed's inclusion criteria. Unfortunately, CINAHL requires a subscription (and has since changed names to EBSCOHost). While this search engine does not utilize MeSH terms, it does have a vocabulary system with the same general functionality. Cochrane Library contains six databases and registries: Cochrane Reviews (systematic reviews and meta-analyses by Cochrane Collaboration), Other Reviews (systematic reviews and meta-analyses by non-Cochrane Collaboration), Clinical Trials (individual RCT performed by other investigators), Methods Studies, Technology Assesments, and Economic Evaluations. It utilizes MeSH terms, but has decreased limitation and expansion of searches functionality. PEDro is a free physical therapy-focused search engine that contains RCTs, systematic reviews, and CPRs in physical therapy. Studies are rated on a 0-10 scale based on their internal validity and statistical interpretability. Hooked on Evidence is a free database of citations for physical therapy interventions based on the pathology. Four criteria must be met to be included in this database: human subjects, at least one physical therapy intervention, at least one outcome measure of the intervention, and published in an indexed English-language peer-reviewed journal. Articles are organized according to research design type (RCTs listed first). There are other search engines out there, but these are some of the more common ones seen. Analyzing the Search Results One thing we definitely need to consider is the type of study. The research design has an impact on bias contributions, applicability to larger populations, and more. According to Jewell, the hierarchy of evidence is: -1a. Systematic Review of RCTs that do not have a statistically significant variation in the direction or degrees of results -1b. Individual RCT with a narrow confidence interval -1c. All or None Study (a study in which some or all patients died before treatment became available, now none die - think a vaccine) -2a. Systematic Review of Cohort Studies that do not have a statistically significant variation in the direction or degrees of results (cohort refers to a group of individuals followed over time that sometimes have a similar characteristic) -2b. Individual Cohort Study (including low-quality RCT) -2c. Outcomes Research -3a. Systematic Review of Case-Control Studies that do not have a statistically significant variation in the direction or degrees of results (a retrospective approach when subjects known to have the outcome are compared to those without) -3b. Individual Case-Control Study -4. Case-Series Study; Cohort or Case-Control Study that did not: define comparison groups adequately or did not measure exposures and outcomes objectively or in a blinded fashion or control for confounders or have sufficient follow-up -5. Expert Opinion without explicit critical appraisal, or based on physiology, bench research or "first principles" While this hierarchy can aide in selection of evidence, we should still read and fully evaluate articles before implementing them into practice. The reason is because a high-level article, such as a systematic review, may have included poor methods: ignoring confounding variables, limited blinding, poor experience of clinicians, etc. There are many items to consider when reviewing evidence. One place that can sometimes be good to start is a literature review, because it often reviews the research up until that point of time. Things to look out for, however, include evidence being judged by date of publication, flow of article, and relation between articles selected and review topic. Each can potentially lead to eliminating useful information. Older studies may still have the best quality of evidence. Sometimes seemingly unrelated articles contain information that is actually very connected to the study. Another quality of studies not mentioned was a meta-analysis. Systematic reviews with meta-analysis incorporate summaries of the primary studies that are critically appraised and statistically combined. The result is an even higher level of evidence. Research design refers to how the study is carried out. In experimental studies, some of the subjects are manipulated with a treatment/intervention (independent variable) in order to study the effect (dependent variable). Experimental studies can have 3 variations for the control group: no treatment, placebo, or both groups get standard treatment but experimental group gets additional interventions. Quasi-experimental studies are similar in that they involve manipulation again, but either lack a second group for comparison or random assignment. There are a few methods for quasi-experimental studies: time series format (repeated measures collected over time before/after experimental intervention is introduced to a single group), non-equivalent group (similar to experimental but no random assignment), single system (one subject undergoes experimental treatment and control treatment periods in alternating fashion), and a few others. In single-system/subject designs, some common methods are A-B, A-B-A, and A-B-A-B formats. "A" refers to baseline and "B" refers to treatment. Non-experimental studies obviously are purely observational. A within-subjects study occurs when the outcome is repeatedly measured in a single group of subjects. Between-subjects refers to outcomes being compared between 2+ groups. Bias can occur in a variety of points in a study: subject recruitment/assignment/communication, calibration/use of equipment, maintenance of environmental condition, and more. It can be minimized with random assignment of subjects and masking of subjects and investigators (if both are blinded, it is referred to as a double-blind study). You may notice some time descriptors for studies as well. Cross-sectional refers to data being collected once during a single point in time. Longitudinal refers to repeated measures over an extended period of time. Retrospective is historical and obviously lacks randomization. Prospective is data being collected in real time. There are many other factors to consider when analyzing the methodological quality of evidence. Inclusion/exclusion criteria can render an otherwise well-performed study useless. We recently did a review of the Joint Line Fullness Test for meniscal injuries. While the results of the study looked promising, the researchers exluded any patients with an acute injury (within 6 weeks of exam) or presence of osteophytes, joint space loss, or arthritis. These are typically the types of patients we see in the clinic, so it doesn't really matter how accurate the test is in other conditions. We should also take note as to whether or not the inclusion/exclusion criteria is even appropriate based on the clinical question. Look at to see if participants were lost during the study (attrition), why they were lost, and if any adjustments were made in the statistical analysis. Consider how many databases/resources were used for the study. After reviewing the various search engines, it should be evident that one database doesn't contain all the information. In systematic reviews, the number of individuals reviewing research studies (and whether or not they were blinded) may impact their findings.
Many experimental studies start off with a null hypothesis that is the common understanding at the time (therapeutic exercise = therapeutic exercise + manual therapy). The researchers develop an alternative hypothesis to challenge what is currently accepted (therapeutic exercise < therapeutic exercise + manual therapy). Tests of significance can be used to determine if any differences found in the groups are true or are due to chance. If they are true, then they may be applicable to the population. The alpha level is first set to determine the level of probability that results are not due to chance. The most common ones are .05 or .01. If the p-value is below these, there is a 5% chance that the differences in the study were due to chance (alpha level 5). Results that are "statistically significant" represent heterogeneity. If there is overlap of confidence intervals or the p-value is not below the alpha level, homogeneity is present. As with any study, there lies the risk of error at some point during the process. Type I error refers to the null hypothesis being rejected when it shouldn't have been. Type II error occurs when the null hypothesis should have been rejected when it wasn't. A t-test can be used to compare 2 different groups. It can be either one-tailed or two-tailed. One-tailed only assess one end of the population distribution. Two-tailed assesses both ends. Any time more than 3 groups need to be assessed for variance, ANOVA (analysis of variance) should be utilized. Simple ANOVAs compare only 1 variable between groups, while factorial ANOVAs compare multiple variables between groups. ANCOVA compares multiple treatment groups, while controlling for any other variables that might affect the results. T-tests, ANOVAs, and ANCOVAs are referred to as parametric tests in that they are based on the population. The calculations result in the previously described p-value to determine if the findings are statistically significant. For non-parametric tests, we can use the Chi square test. It compares actual frequencies to expected and is followed up with a p-value to again determine the likelihood that the results are true, instead of being due to chance. Some values that are regularly reported for examination techniques include sensitivity, specificity, positive/negative likelihood ratios and positive/negative predictive values. Sensitivity refers to a test's ability to accurately rule out a disease and is scored between 0 and 1.00. Tests with high Sensitivity, rule Out a disease (SnOut). Specificity refers to a test's ability to accurately rule in a disease and is scored between 0 and 1.00. Tests with high Specificity, rule In a disease (SpIn). Positive and negative likelihood ratios work in a similar way but are not limited to numbers between 0 and 1.00. They act more as "persuasive information" and are more individualized than sensitivity and specificity(Jewell, 2010). Clinicians are required to determine a patient's pretest probability, then incorporate the likelihood ratio for the test and determine how "likely" the patient has the pathology. Predictive values are used to determine the true positives (or negatives) out of those that tested positive (or negative), both true and false. Another common statistic we'll see is correlational research. These studies look to see how well two variables are related to each other; they do not signify causation. The numbers are expressed between -1.00 to 1.00. When near zero, there is a low correlation/relationship. When near 1.00 or -1.00 there is a strong relationship. Positive refers to direct correlations, while negative refers to inverse correlations. This may be referred to as "Pearson's r" for two groups or "Intraclass Correlation Coefficient (ICC)"6 for 3 or more groups. These values can be used to assess the reliability of examination techniques as well. Intra-rater reliability refers to the ability of an individual to consistently obtain the same findings given the same variables. Inter-rater reliability refers to the ability of different individuals to obtain the same findings given the same variables. As you can see there is a lot to remember when it comes to appraising evidence. Hopefully, you found this review useful for a foundation in your studies and the practice of utilizing evidence, but this does not by any means encompass everything. If you need further information for statistical analyses and research design, we recommend reviewing your notes and text books. Most of the information discussed in this review is from Jewell's Guide to Evidence-Based Physical Therapist Practice. Reference:
Jewell, Dianne. Guide to Evidence-Based Physical Therapist Practice. Sudbury, MA: Jones & Bartlett Learning 2011. Print.  Posterior Interosseous Nerve (PIN) Syndrome is a pathology that involves pain and/or motor weakness as a result of nerve compression. In parts of the medical community, Radial Tunnel Syndrome and PIN Syndrome are one in the same, while in other parts they are different diagnoses with the same nerve involvement (Posterior Interosseous Nerve). These health care professionals identify Radial Tunnel Syndrome as pain along the radial tunnel, while PIN Syndrome is marked weakness in the muscles innervated by the Posterior Interosseous Nerve. Due to the fact that both syndromes involve compression of the same nerve, often by the same structures, we will use the terms PIN Syndrome and Radial Tunnel Syndrome synonymously in this review, especially due to the fact that the two are managed identically.
Pathogenesis: Since the posterior interosseous nerve is a motor nerve, it may appear confusing as to why pain is often a complaint. One of the hypotheses for this pain syndrome is that the PIN also carries some afferent fibers that include C-fibers, which are relatively smaller compared to the motor component. Thus, compression would elicit pain, while still demonstrating the normal EMG findings of the larger motor component. (Naam & Nemani, 2012). Lubahn & Cermak state that the pressure disrupts local blood flow or axoplasmic flow in the nerve, thus, producing the pain we see in our patients. However, Portilla Molina et al claim that the PIN also carries sensory and proprioception fibers to the posterior capsule of the wrist (we must remember that this cadaveric study is from 1998 as well). This goes against what most of the literature reports, but should still be kept in mind as our understanding of the diagnosis continues to develop. The PIN may be compressed by the arcade of Frohse, other tissues of the supinators, the leash of Henry from the radial artery, and the edge of the ECRB muscle (Ducic et al, 2012). The arcade of Frohse is an anatomical variant that is found in about 30-50% of the population and is located at the proximal edge of the supinator (Andreisek et al, 2006). It is a fibrous adhesion that connects the brachialis and brachioradialis muscles. Tsai & Steinberg use the acronym FREAS to identify potential sites of constriction: -F: fibrous bands about the radiocapitellar joint -R: radial (artery) recurrent branches -E: extensor carpi radialis brevis muscle -A: arcade of Frohse -S: distal edge of supinator Portilla Molina et al hypothesize that the PIN is fixed in the supinator muscle and becomes elongated and compressed with pronation/supination. This suggests that PIN Syndrome is a pathology based on repetition (and it can be), but injury to the nerve can also be from a traumatic nature as well (Sueki & Brechter, 2010). While this classification system is rarely used with entrapment pathologies, classification can be made based upon the severity of injury and potential for healing. As the nerve can demonstrate severe thinning/thickening at the sites of compression, these classification levels may still prove useful: -First-Degree Neuropraxia: disruption of myelin around the Nodes of Ranvier resulting in temporary loss of nerve conduction with rapid recovery usually. -Second-Degree Axonotmesis: interruption of axon with resulting wallerian degeneration. The tissue around the axon is still intact. Full recovery is possible, but time for recovery depends on distance between the injury and the target structure. -Third-Degree Neurotmesis: disruption of the nerve and its supporting structures, especially the endoneurium. The perineurium and epineurium are still intact. -Fourth-Degree Neurotmesis: all parts of the nerve are destroyed except the epineurium. -Fifth-Degree Neurotmesis: completely severed nerve with no potential for regeneration. Clinical Presentation: Pain is typically present at the proximal dorsoradial aspect of the forearm and is increased with forearm rotation. Muscle weakness may be present as well (or instead) as a result of either pain inhibition or compression of the motor nerve (Naam & Nemani, 2012). Along with forearm rotation, forceful elbow extension may produce pain (Ducic et al, 2012). As stated earlier, compression may also lead to weakness in the muscles innervated by the PIN. Patients with PIN Syndrome will have a negative Tinel's sign, due to the fact that the Posterior Interosseous Nerve is a motor nerve (Andreisek et al, 2006). Patients often have difficulty maintaining finger extension, and following finger extension, you will see the fingers quickly drop back into flexion. You may also see radial deviation with wrist extension due to weakness of the extensor carpi ulnaris. If weakness is noted in the extensor carpi radialis longus/brevis or brachioradialis, the clinician should suspect a more proximal compression of the nerve (Tsai & Steinberg, 2008). Tsai & Steinberg found that 5% of patients with lateral epicondylopathy also suffer from Radial Tunnel Syndrome. Kalb et al found that 52% of patients with PIN compression had lateral epicondylopathy as well. As you can see, it's important to screen for both in patients with elbow pain. PIN Syndrome is typically due to overuse (athletes and violinists especially), external compression (such as with crutch use), radial head fracture, soft tissue tumors, and more (Andreisek et al, 2006). Certain job activities have been shown to have a link to development of Radial Tunnel Syndrome, such as handling tools with full extension of the elbow (Naam & Nemani, 2012). Using a force of at least 1 kg more than 10x/hour with the elbow extended between 0-45 degrees with frequent pronation/supination has been shown to have increased incidence of developing Radial Tunnel Syndrome. Diagnosis: One of the more distinguishing signs in diagnosing Radial Tunnel Syndrome is tenderness over the anatomical landmark of the Posterior Interosseous Nerve, 3-5 cm distal to the lateral epicondyle (Naam & Nemani, 2012). It should be noted that there is controversy surrounding the diagnosis of Radial Tunnel Syndrome due the lack of objective findings. Pain should not be increased with resisted wrist extension. Due to the proximity of the lateral epicondyle, it is important to differentiate between Lateral Epicondylopathy and Radial Tunnel Syndrome, especially since they often occur together. Local anesthetic injection can be used to aide in differentiating between these two. Lateral Epicondylopathy will be relieved by injection of an anesthetic, while Radial Tunnel Syndrome rarely has any changes. We must also be sure to check for potential cervical radiculopathy (Sueki & Brechter, 2010). In fact, there is some controversy in the literature regarding cervical radiculopathy being an ignition for Radial Tunnel Syndrome (or any upper extremity nerve entrapment); this is known as Double Crush Syndrome. The Radial Neural Tension Test will be especially useful in these cases, but may be positive with any Radial Nerve-related entrapment as well. Other potential causes of peripheral neuritis include polyarteritis, rheumatological disorders, and post-systemic illness angioneuropathy and should be considered during your differential diagnosis. When diagnosing Radial Tunnel Syndrome, be sure to rule out extensor tendon ruptures, sagittal band ruptures, and inflammatory involvement of the MCP joints as these can all have a similar clinical presentation. One suggested method of diagnosing RTS involves drawing 9 squares over the anterior forearm for location of pain. Tenderness in the lateral 3 squares supposedly is linked to RTS (Loh et al, 2004). Clinically, we may see production of pain with resisted supination in full elbow extension or pain with passive elbow extension with wrist flexion and pronation (Lubahn & Cermak, 1998). Some literature recommends the use of middle finger resisted extension to identify Radial Tunnel Syndrome, but due to the attachment at the lateral epicondyle, there remains the potential for false positives (Sueki & Brechter, 2010). As with most pathologies, the earlier the diagnosis, the better the outcomes. According to Adreisek et al, MRI can be useful in diagnosing Radial Tunnel Syndrome as well. It is well known that MRI is capable of identifying mass lesions, nerve enlargements, and neuritis. Also, signal intensity changes in the muscle, in particular muscle edema, is often used in diagnosis due to the difficulty involved with identifying changes in the nerve itself. The MRI is not useful in identifying patients with PIN Syndrome by locating the compressing structures. Instead, diagnosis is based on the pattern of muscle denervation. With Radial Tunnel Syndrome, the supinator, extensor digitorum, extensor carpi ulnaris, extensor digiti minimi, abductor pollicis longus, extensor pollicis longus/brevis, and extensor indicis may have abnormal signal intensity while the extensor carpi radialis muscles are normal. One would think that nerve conduction velocity tests and EMGs would be used widely, however, due to the lack of established diagnostic guidelines, there is rarely a large enough drop to be clinically useful. You might expect a conduction block or prolongation of radial nerve conduction; however, one theory for the lack of changes is that the testing is often done in neutral forearm position, where changes in conduction do not always occur (Portilla Molina et al, 1998). Martinoli et al reviewed the use of sonograms in diagnosing Radial Tunnel Syndrome. According to the authors, high resolution sonograms are able to identify compression of the Posterior Interosseous Nerve by the supinator. The nerve may appear swollen and hypoechoic from edema, segments of thinning and thickening, or encased by scar tissue at the distal edge of the supinator. Conservative Treatment: Conservative treatment typically consists of a variety of interventions: wrist splinting, activity modification, NSAIDs, and exercise (Naam & Nemani, 2012). A wrist cock-up splint may be useful by slackening the wrist extensors (and thus decreasing pressure in the radial tunnel) (Lubahn & Cermak, 1998). Tsai & Steinberg recommend beginning treatment with wrist/elbow splints, NSAIDs, and restriction of aggravating activities. Wrist flexion and pronation combined with elbow extension should be avoided, along with any position that aggravates symptoms. Due to the compressive nature of the pathology, the clinician should consider including soft tissue release work, myofascial release work and neural mobilization techniques (Sueki & Brechter, 2010). 72% of patients had been shown to improve following a single injection of 40 mg of triamcinolone and 2 mL of 1% lidocaine at 6 weeks, but we should consider the fact that this study contained a low number of participants. According to Lubahn & Cermak, a cortisone shot around, not into, the nerve should be considered as well. Should symptoms not improve within 90 days, the surgical approach should be considered due to the low likelihood of spontaneous recovery. After 18 months of symptoms, muscle fibrosis occurs (an irreversible condition). Surgical Treatment: Lengthening the supinator has been shown to lower the pressure inside the radial tunnel, while lengthening the extensor carpi radialis brevis and extensor digitorum communis had no effect (Naam & Nemani, 2012). The Dorsal (Henry) Approach involves exposing and pushing aside the sensory nerves, arteries, and uninvolved muscles (brachioradialis, extensor carpi radialis brevis/longus before dividing the arcade of Frohse and superficial portion of the supinator muscle. Bupivacaine is injected before dressing application. The Transmuscular Brachioradialis-Splitting Approach involves just what you would think, splitting the muscle fibers and overlying fascia before exposing the radial nerve, at which point the supinator and arcade of Frohse are divided. The Dorsal Approach Between Brachioradialis and Wrist Extensors involves indentifying and developing the interval between the brachioradialis and extensor carpi radialis longus in order to expose the arcade of Frohse. The Anterior Approach is used for when there is proximal compression as well as distal. The process involves exposing the radial nerve between the brachialis and brachioradialis then following the nerve distally until it branches to the superficial radial nerve and PIN. Here the arcade of Frohse is released, the arteries are ligated, and the entire supinator is released as well. Both the Anterior and Posterior Approaches carry the risk of damaging the PIN due to the proximity of the incision, so precision is a necessity (Mekhail et al, 1995). Ducic et al discusses an endoscopic nerve release the requires a shorter incision length. This could potentially lead to better outcomes and only requires a simple lighted retractor to help expose the desired tissue structures. General post-op care involves AROM beginning 3-5 days after surgery, strengthening at weeks 3-4, return to limited duty at work during weeks 2-3, and return to full duty at 4-6 weeks. Lubahn & Cermak recommend using a long-arm posterior splint with the wrist in neutral position with gradual ROM progression beginning 1 week after surgery, focusing on stretching the extensor muscles. Return to prior level of function may take 6-12 weeks. References:
Andreisek G, Crook DW, Burg D, Marincek B, Weishaupt D. (2006). Peripheral neuropathies of the median, radial, and ulnar nerves: MR imaging features. Radiographics. 2006 Sep-Oct;26(5):1267-87. Web. 10 May 2013. Ducic I, Felder JM 3rd, Quadri HS. (2012). Common nerve decompressions of the upper extremity: reliable exposure using shorter incisions. Ann Plast Surg. 2012 Jun;68(6):606-9. Web. 05 May 2013. Kalb K, Gruber P, Landsleitner B. (1999). [Compression syndrome of the radial nerve in the area of the supinator groove. Experiences with 110 patients]. Handchir Mikrochir Plast Chir. 1999 Sep;31(5):303-10. Web. 11 May 2013. Loh YC, Lam WL, Stanley JK, Soames RW. (2004). A new clinical test for radial tunnel syndrome--the Rule-of-Nine test: a cadaveric study. J Orthop Surg (Hong Kong). 2004 Jun;12(1):83-6. Web. 11 May 2013. Lubahn JD, Cermak MB. (1998). Uncommon nerve compression syndromes of the upper extremity. J Am Acad Orthop Surg. 1998 Nov-Dec;6(6):378-86. Web. 11 May 2013. Martinoli C, Bianchi S, Pugliese F, Bacigalupo L, Gauglio C, Valle M, Derchi LE. (2004). Sonography of entrapment neuropathies in the upper limb (wrist excluded). J Clin Ultrasound. 2004 Nov-Dec;32(9):438-50. Web. 11 May 2013. Mekhail AO, Ebraheim NA, Jackson WT, Yeasting RA. (1995). Vulnerability of the posterior interosseous nerve during proximal radius exposures. Clin Orthop Relat Res. 1995 Jun;(315):199-208. Web. 12 May 2013. Naam NH, Nemani S. (2012). Radial tunnel syndrome. Orthop Clin North Am. 2012 Oct;43(4):529-36. Web. 01 May 2013. Portilla Molina AE, Bour C, Oberlin C, Nzeusseu A, Vanwijck R. (1998). The posterior interosseous nerve and the radial tunnel syndrome: an anatomical study. Int Orthop. 1998;22(2):102-6. Web. 12 May 2013. Sueki D & Brechter J. Orthopedic Rehabilitation: Clinical Advisor. Maryland Heights, MO: Mosby Elsevier, 2010. 751-752. Print. Tsai P, Steinberg DR. (2008). Median and radial nerve compression about the elbow. J Bone Joint Surg Am. 2008 Feb;90(2):420-8. 11 May 2013.
Anatomy The ACL has a medial attachment near the anterior intercondylar area of the tibia and blends with the anterior portion of the lateral meniscus (Markatos et al, 2012). It then ascends in a posterolateral direction to attach to the posteromedial aspect of the lateral femoral condyle. In doing so, the ACL internally rotates as it ascends and is divided into two separate bundles. They are known as the anteromedial and posterolateral bundles. The names are based off tibial insertion sites. With the combination of two bundles and twisting of the fibers, the ACL is able to provide resistance in various angles of knee motion and provides 86% of the stabilization against an anterior drawer force. The anteromedial bundle is taut primarily at 90 degrees of flexion, while the posterolateral bundle increases its tautness as the knee nears full extension. The ACL is able to withstand 1,725 +/- 270 N of force. Since our bodies are impacted by forces greater than this during many athletic activities, the muscles surrounding the knee are able to dampen some of the forces. Based on the orientation of the fibers, the ACL plays a significant role in resisting anterior tibial translation, axial tibial and valgus knee motions. The ACL primarily consists of 90% Type I collagen (10% Type III) and contains many sensory nerve endings, signifying its importance for proprioception and kinesthesia. As the ligament is covered by synovium, it is referred to as extrasynovial, so blood is supplied primarily by branches from the genicular arteries. Mechanism of Injury As parts of the ACL are stressed at each angle of knee motion, the ligament is often at high risk for injury. The majority of ACL injuries are actually non-contact. Three common factors that are associated with ACL rupture include: strong contraction of the quadriceps muscle over a slightly flexed or fully extended knee, a marked valgus collapse of the knee, and excessive internal rotation of the knee (Neumann, 2010). Hyperextension of the knee, while the foot is planted, is also linked to ACL injury. As the ACL limits anterior tibial translation, a strong contraction of the quads will pull the tibia forward and tear the ACL, especially if the hamstring is unable to counteract the force of contraction. Valgus collapse is a phenomenon commonly seen in female athletes. Following landing from a vertical jump or lunge, the femur goes into adduction and internal rotation. The ACL is especially at risk here due to the MCL being lax in a flexed position. Here the ACL plays a larger role in resisting valgus motion. Hyperextension of the knee on a planted foot ruptures the ACL by having the femur slide excessively posteriorly on a fixed tibia. Something to consider is the association between ACL tears and the valgus motion that causes the injury. As a valgus restraint, the MCL plays an important role in protecting the ACL. Often, we see individuals with both ligaments injured. In individuals with sprained MCLs (and thus hypermobile knees), the ACL is placed at increased risk for injury. The MCL is actually one of the prime stabilizers of the knee. Interestingly, the MCL and ACL have different healing positions that contradict one another. If both ligaments are found to be injured, they frequently are repaired during the same procedure. The ideal healing position for the MCL is knee flexion, while the ideal position for the ACL is knee extension. Usually, the ACL's healing is prioritized and the patient has an emphasis placed on gaining extension. This results in the MCL healing into a lax state and leads to hypermobility of the knee, placing the ACL back at greater risk for injury! Perhaps these individuals should undergo one surgical procedure at a time in order to regain a truly stable knee.
When examining the patient, we will see a loss of flexion and extension, secondary to knee effusion, and quadriceps inhibition. Use of the KT1000 arthrometer has been shown to be accurate in identifying ACL tears with a presence of > 3 mm. difference between sides. Additionally, patients will present with a significant deficit with proprioception due to the ACL's large role in joint positioning. Upon suspicion of ACL rupture, an MRI is often ordered for confirmation. Along with identifying the integrity of the ligament, the MRI can aid in detecting the presence of bone contusions. It is now known that bony contusions following ACL rupture have a strong correlation to the development of knee osteoarthritis. It is for this reason, that we must address the joint effusion quickly. Van Ginckel et al performed a study looking at cartilage deformation following early return to sports. While no difference was found in cartilage thickness at 6 months post injury, the authors did find structural properties of the cartilage that put the tissue at risk for destruction, potentially leading to early development of knee osteoarthritis. It should be noted that females have been found to be at higher risk for ACL injuries compared to males. The proposed intrinsic factors that contribute to this difference include: increased Q-angle, decreased femoral notch size, smaller ACLs, and increased posterior tibial slope (Sutton & Bullock, 2013). The increased Q-angle places a significant valgus force on the knee and ACL, especially when landing from a jump. In fact, the study found that females that had an increase of 8.4 degrees of knee abduction at initial contact were predictive of ACL rupture. Whether or not there are gender differences in femoral notch size is still under discussion, but a frequent component of ACL reconstruction is simultaneous enlargement of the femoral notch. Some research has shown that females have a thinner ACL at midsubstance, but there is also evidence that there is no difference compared to male counter-parts. A posterior tibial slope theoretically places the tibia more anterior to the femur, and upon quadriceps contraction, increases the stress on the graft. There is mixed evidence on this component as well.  Surgical Management: There are almost 200,000 injuries each year involving the ACL, and over half of these require surgical intervention. However, not every individual is appropriate for ACL reconstruction. Those who would benefit from surgery include individuals with repeated episodes of knee buckling, an injury that affected several structures, and the desire to return to a high demand activity that requires knee stability. Factors that may indicate non-surgical management include: little exposure to high demand activities, age > 40 years, severe OA, prolonged coping with ACL deficiency, and those unlikely to comply with post-surgical protocol. The general sequence of surgery is graft harvest/preparation, diagnostic arthroscopy, drill tibia tunnel, drill femoral tunnel, and fixation of graft at each end. The purpose of the diagnostic arthroscopy is to identify any additional injuries in the knee, such as meniscal tears, cartilage damage, etc. Here the surgeon can perform any additional procedures necessary based on the arthroscopy's findings. Next, the physician drills the tibial and femoral tunnels. If using a BPTB graft, the patellar bone is inserted into the tibial tunnel, while the tibial bone is placed in the femoral tunnel (Manske, 2006). For alternate graft types, fixation can be either direct or indirect. Direct fixation includes interference screws, washers, cross-pins, and staples, while indirect fixation devices include suture-posts and polyester tape-titanium buttons. Tunnel enlargement has been found at 5 years after surgery, especially with use of interference screws (Dave et al, 2013). The authors found a biologic component to be involved and offered the opinion that tunnel enlargement could be decreased with accelerated rehab; however, no difference was found in clinical outcomes. Single-Bundle (SB) Technique has long been referred to as the gold standard in ACL reconstruction techniques (Xu et al, 2013). However, as the understanding of the anatomy of the ACL has developed, so has our understanding of surgical reconstruction. The SB has been shown to have good anterior stability but lacking in rotary and frontal plane stability. Since we now know the ACL is important for more than just anterior-posterior stability and with our knowledge of the ACL having an anteromedial and posterolateral bundle, there has been a push to increase utilization of the Double-Bundle (DB) Technique. With the addition of another bundle in the graft, the surgically reconstructed knee can have increased stability in multiple planes as it mimics the dual bundle form of a natural ACL. Xu et al found that DB had greater anterior and rotary stability than SB but no difference in subjective reports of stability. Some of the most common graft selections for ACL reconstruction include: autografts (hamstrings, bone patellar tendon bone (BPTB), quad tendon) and allografts (tib ant, post tib, achilles, BPTB, etc.). The advantage of BPTB include strongest early fixation due to bone healing properties and it doesn't compromise the hamstrings (an important quad force dampener). The disadvantages include direct anterior knee pain, longer early recovery, and length of graft may not match that of tunnels. Some of these disadvantages can be countered by use of a contralateral patellar tendon graft. Ipsilateral grafts have conflicting goals of increasing strength in the quads due to the donor site and increasing ROM in the knee following ACL reconstruction (Manske, 2006). The pros of hamstrings include quicker post-op quad control, easier early rehab, less painful anterior knee pain, and stronger graft. In fact, the hamstring graft can utilize multiple strands, increasing the strength of the graft to greater than all other graft types. Unfortunately, this advantage is somewhat insignificant due to the hamstring grafts having their weakest point at the attachment site. The cons include decreased hamstring activity (hamstrings are important restraint to anterior translation), decreased hamstring strength in deep flexion, graft quality is not as consistent, and the need for suspensory fixation. Allografts are useful because surgery is faster (no need to harvest graft from patient), faster rehab, and more cosmetic. Unfortunately, these grafts are more expensive, place the patient at higher risk for infection, and they don't incorporate as well or fast compared to autografts. Now that we know the theories for selecting each graft type, let's look at some of the recent evidence. The Bone Patellar Tendon Bone (BPTB) graft is commonly referred to as the gold standard in ACL reconstruction due to having 168% strength compared to the ACL and improved bone-to-bone healing properties as compared to ligament-to-bone (Pan et al, 2012). However, BPTB autologous grafts come with the increased chance of donor site morbidity: patellar fracture and anterior knee pain. It was found that artificial ligaments like Ligament Advanced Reinforcement System (LARS) have equal clinical outcomes without donor site morbidity. We may see increased use of artificial grafts in the future. Zelic et al & Abbas et al found there were no significant differences between patellar ligament and hamstring tendon grafts in regards to knee stability except individuals who used a pateller ligament graft had a statistically significant greater chance of developing anterior knee pain at 6 months. However, the anterior knee pain did not affect outcomes. The management of pediatric ACL ruptures is somewhat debatable. The issue of provoking growth deformities by performing transphyseal surgery in reconstruction exists (Frank & Gambacorta, 2013). This led to the approach of delaying surgery until skeletal maturity; however, due to hypermobility without a functioning ACL, the child athletes often experience increased meniscal and cartilage damage (this is also seen in the adult population (Magnussen et al, 2013)). Frank & Gambacorta found improved clinical outcomes with early surgical reconstruction versus delayed for the pediatric population. The potential for growth abnormalities can be decreased by use of soft tissue grafts in transphyseal tunnels. Tissue Healing: Following ACL reconstruction, one of the most important factors that should guide your treatment plan is the tissue healing time frame. As individuals are anxious to return to their prior levels of function, accelerated rehab protocols were developed. Unfortunately, an increase in graft failure rate was noticed and further research was needed to guide the aggressiveness of therapy. It is now known that initially, the graft is actually stronger than a normal ACL and it is the bone attachments in the tunnel that are of concern (Muller et al, 2013). Overly, aggressive activities can loosen these attachments, prolonging inflammatory reactions and leading to graft failure. Controlled motion is encouraged, however, as this can aide in improving some of the biomechanical properties of the graft. After further investigation, we now know that the graft's purpose is merely as a "scaffold" for cell proliferation to occur. There are 3 phases in graft ligamentization: Incorporation, Revascularization, and Graft Healing/Maturation. The time frame is somewhat general, but Incorporation typically occurs in the first 3 weeks. This involves an inflammatory response as the graft degenerates and fibroblasts die. The tissue that remains from this is known as a "scaffold." Revascularization occurs from week 3 to about week 16 as the capillaries invade the graft from the synovium. The host's fibroblasts migrate into the graft tissue. Without this occurring, the graft will fail. At weeks 8-10, the graft is at its weakest point, so it is important to avoid stressing the graft. Graft Healing/Maturation begins after Revascularization. The graft strength drops to as low as 11% of a normal ACL. The graft matures as there is a build-up of collagen content but will not reach normal ACL tensile strength until at least over a year (if at all). According to Rabuck et al, it would appear there may be a role for imaging to be involved with staging of the rehabilitation process in the future. As the ligament undergoes revascularization, MRI can potentially be used to detect the levels of revascularization and thus aid in determining the forces the graft can withstand at the time. CT and radiographs may be useful for detecting widened tunnels at the bony attachments. Rehabilitation: Rehabilitation is often thought of as the time following an ACL reconstruction. With these patients, let us not forget the importance of "prehabilitation"-- the time after injury but before surgery. In fact, there are several reasons surgeons elect to delay ACL reconstruction several weeks following injury. While not all patients receive pre-operative rehab, several studies have demonstrated the importance of a good quadriceps ratio and full knee extension range of motion. Adams et al found that patients with full knee extension ROM, absent or minimal joint effusion, no quadriceps lag with a straight leg raise, and a quadriceps index >90% had better post-surgical outcomes (Adams 2012). The swelling in the knee could impair the healing process following reconstruction and limit ROM. This leads to the next reason for waiting: regaining full ROM. Decreased extension is a significant complication following surgery that may be linked to further knee damage. By regaining the motion prior to surgery, the patient is more likely to return to higher level activity and decrease the chances of further knee injury. The final reason for delaying surgery is to strengthen the quadriceps. As we all know, there is a quadriceps strength deficit following joint effusion and surgery. As quadriceps strength is linked to function, it is desirable to regain as much strength as possible before surgery. Therefore, our goals prior to surgery include decreasing swelling, increasing knee ROM (especially extension) and increasing quadriceps strength. It has been shown that early rehabilitation improves knee function following ACL reconstruction (Zhu et al, 2012). That being said, there are several milestones we should look to reach in rehabbing our patients. Initially, we want to decrease knee pain and swelling, restore knee extension ROM, and improve quadriceps recruitment. These early milestones are similar to our prehabilitation goals. We usually are not the first individuals to jump to using modalities, but evidence shows Russian stim + exercise improves quadriceps strength greater than exercise alone (Kim et al, 2010). Therefore, e-stim may be a useful tool in your rehabilitation program. It's easy to see how important they are for quality outcomes. Once these goals have been achieved, we want to have the patient focus on normalizing their gait. The final items to focus on include restoring knee flexion ROM, proprioception, LE muscle performance, and return to function. These items will be expanded upon later. Following surgical reconstruction, it is essential that the patient achieves full knee extension for maximum functionality. Even a 3-5 degree loss of extension ROM has shown to negatively impact patient subjective and objective reports & an association with decreased quadriceps strength (Adams 2012). Upon failure to achieve full extension, pain with extension overpressure, or an audible clunk with extension, the clinician should consider the presence of a cyclops lesion (Silverwood et al, 2012). It can be confirmed with MRI or arthroscopic visualization. A cyclops lesion is a localized arthrofibrosis in the anterior intercondylar notch and often requires arthroscopic excision. Another reason to achieve full extension, and full ROM for that matter, is to decrease the likelihood of developing OA. Decreased knee ROM following ACL reconstruction has been shown to be associated with the development of knee osteoarthritis (Shelbourne et al, 2012). It is important to remember that "full ROM" refers to normal ROM for the individual. We can use side-to-side comparisons to determine the achievement of full motion.  An important consideration when selecting exercises for your patient is the amount of strain placed on the graft. Escamilla et al found strain on the ACL is greatest at knee flexion angles of 30 degrees and less for both Open Kinetic Chain (OKC) and Closed Kinetic Chain (CKC) exercises, especially at 10-15 degrees of flexion. OKC knee extension at angles < 30 degrees should be avoided until the graft is fully revascularized; however, quadriceps activity at 0 degrees of flexion (full extension) does not overstrain the graft, due to increased stability. This means that straight leg raises (SLR) can be a useful component to strengthening the quadriceps near extension. Be sure your patient does not have any extension lag when performing the exercise, otherwise the integrity of the graft tissue may be put at risk. While the ACL is still strained in CKC, the addition of hip muscle activity and hamstring activity dampen the forces on the graft. These muscles are more active due to the increased need for stability and are more functional than OKC exercises. In higher-level athletes that have returned to pre-injury level, it was found they had greater activation of gluteus maximus and gastrocnemius and decreased activation of the quadriceps (Nyland et al, 2013). As we already know, following ACL rupture the individual experiences decreased knee proprioception. With greater use of the hip and ankle muscles, the patient can increase prioprioception at these joints. Increased sensation and muscle activation at the joints surrounding the knee increases stability in the extremity and puts less stress on the knee (and graft). To further lessen the strain on the ACL during CKC exercises, a forward trunk lean of about 30 degrees can be used. This increases activity of the hamstrings, which we already know counters the ACL strain. When a forward trunk lean is not utilized, we often see anterior knee translation, leading to increased stress on the graft. When the knee travels 8 cm past the toes, the tissue is placed at especially high risk for failure. The review also showed those who used primarily CKC exercises experienced less knee pain during rehabilitation. CPMs are frequently known for their use following total knee arthroplasty, and there has been discussion on their potential for use following ACL reconstruction. Review of the literature has found there is no statistically significant advantage to using CPM following surgery (Lobb et al, 2012). Additionally, there has been further research on the use of bracing. No benefit was found in using bracing following reconstruction, however, it may still play a role for individuals prone to knee stiffness. Bracing can aid in ensuring full knee extension. Interestingly, the review also found no difference between home-based and supervised physical therapy. It's unsure on what level of involvement the therapist should have with home-based PT. Kruse et al also found bracing and CPM to have no benefit at all. You will still frequently see physicians and other health care practitioners prescribe functional braces for athletes following ACL reconstruction. They have been shown to limit only anterior tibia translation only at low loads. The loads in ADLs, cutting, and jumping far exceed that which the brace can protect. While mechanically the brace may have no proven benefit, there may be a role for use if if affects the psychological component of the patient. Kruse et al also found that an accelerated program had no deleterious effects when immediately post-operatively the patients could initiate weight-bearing, knee motion 0-90 degrees of flexion, and CKC exercises. After 3 weeks, eccentric quadriceps and isokinetic hamstring exercises could be included. Eccentric exercises are well known for their utilization with tendinopathy. As quadriceps strength deficits continue to exist for increased lengths of time following ACL reconstruction, therapists are eager to find a method of combating the impairment. While early progressive, high-force eccentric exercises may have been contraindicated in the past, there is evidence that they may be safe to use for these patients and could potentially improve the strength gains of the affected quadriceps muscle (Lepley & Palmieri-Smith, 2012). A potentially useful neurological component to add to the rehabilitation of these patients is cross-exercise. Cross-exercise is training of the same muscle on the uninvolved limb and seeing carryover to the involved limb's muscle. Quadriceps strength in the surgical knee has been shown to be impaired. Due to the previously discussed limitations graft healing places on quadriceps activation, we are unable to focus on the muscle's impairments as much as we would like. In order to rectify the strength deficit, cross-exercise has been shown to improve quadriceps strength and should be considered as an adjunct to your treatment plan (Papandreou et al, 2012). The point in time at which the athlete should return to sport is always a debatable topic. Of use are functional tests (single-leg hop, timed hop test, shuttle run and stair hop test) that compare the involved limb to the uninvolved limb (Baltaci et al, 2012). The role of the psychological component cannot be overstated. Individuals who express fear of re-injury typically do not return to pre-injury level (Feller & Webster, 2013). In fact, using a patient's comfortability with an exercise can be a useful tool for progression. The study showed that individuals who advanced their rehab program based on when they felt comfortable were at no greater risk for re-injury. Check out this previous post by Brian on outcome measures for return to sport! Going back to the issue of gender differences in ACL injuries, an emerging concept to decrease the gap between men and women involves neuromuscular training or movement re-training programs. The theory involves retraining the athletes to avoid vulnerable positions when exercising/competing, especially in one-legged standing, out-of-control baseline landings, and straight leg landings. Strength and power exercises, neuromuscular training, plyometric exercises, and agility exercises should be included. The females are taught to emphasize having their knee over toes when landing from a jump or cutting. Research has shown that these movement training programs can lower the incidence of female ACL rupture to equal that of males (Sutton & Bullock, 2013). To identify individuals who would benefit most from this type of program, a drop off a 31 cm box leading into a full vertical leap can be used. With this test, the examiner can assess knee motions that put the athlete at risk. Another component of ACL injury and re-injury is movement asymmetry. When forced to perform unilateral sport-specific movements, the asymmetries become even more prominent. An important component of injury prevention and rehabilitation should be restoration of movement symmetry (Hewett et al, 2013). Strength symmetry of at least 85% (compared to uninvolved side) is often advised prior to beginning cutting, pivoting, and jumping. This is especially important for quadriceps strength and quadriceps/hamstring ratio. As many of you know, rehabilitation following ACL reconstruction is typically protocol driven. While the protocols differ based on each surgeon, the principles of them are generally the same (see our earlier paragraph on goals). Rehab Webinar's Kevin Wilk has a 6-phase protocol that we have summarized below: -Pre-op: re-establish ROM, control swelling, limit activity, and restore quadriceps control (see our earlier paragraph for increased description) -Immediate Post-op (days 1-7): restore full knee extension and gradually increase flexion (do not overstress!), control swelling, patellar mobilizations, e-stim with exercise, restore quadriceps control and independent ambulation, CKC mini-squats, and ankle pumps -Early Phase (weeks 2-4): focus on hip muscles, HS curls (unless HS graft; then wait 6-8 weeks), cycling, lateral cone high stepping (knees as high as hip), balance beam activity, lateral lunges (starting with 30 degrees of knee flexion and 45 degrees of hip flexion) at various angles), reactive squats, wobble boards, foam, wobble board squats (start as early as 3-4 weeks) progress to one leg with stationary holds and ball toss against rebounder with perturbations Intermediate Phase (weeks 4-10): stabilization muscles from above and below, can progress lateral cones with passing as well and speed, progress lateral lunges to deeper depth to facilitate quad-HS co-activation and progress to unstable surfaces with ball toss, front step down/single leg squat (week 4-5) progress to higher steps, to train hip to improve valgus do Romanian Dead Lifts (and maybe single leg deadlifts), work on dynamic Q-angle, stand on bosu ball with knee flexed to 30 degrees and ball toss, or same thing single leg kneeling, monster walks, front step downs standing on foam on box, hip strengthening in different positions, single leg squat on box on foam with on/off theraband forces, ball toss on squat on bosu, modified RDL star drill while standing on foam with ball toss, ball toss with single leg stance on bosu (progress with added perturbations), single leg stance on foam while moving medicine ball in different directions – add perturbations to ball, leg press, wall slides, front step downs, front lunges, squats (but be careful), wall slides on a box, leg press and bridging with T-band around thighs, lateral planks with hip abduction, plank with hip extension (progress to stability ball), lateral step down with half foam roller (small preferable). -Advanced Phase (weeks 10-16): Wilk recommends using an alternating day program to not overwork the involved ACL. These components include neuromuscular drills, perturbation training, strengthening, ROM, balances drills, proprioception training and more. Strengthening drills include long arc quads (90-40 degrees of flexion), hamstring exercises in an OKC, Nordic curls, and stability ball bridges. For balance, perform the STAR drill and advance single limb balance activities. Agility drills include single leg balance while performing a dynamic motion with the contralateral limb. Backwards running, light cutting, and varying acceleration speeds are all acceptable. Running is typically started around 10-12 weeks and begins unweighted or in a pool if possible. -Return to Activity Phase (weeks 16-26): Here, the athlete typically begins more sport specific drills. To initiate these higher level exercises, it's important to assure the patient has reached a certain level of knee stability. Knee arthrometer testing and isokinetic testing are commonly used to assess when to advance plyometrics and running. To advance safely, the hamstring/quadriceps ratio should be 66-72% in males and >75% in females. Additionally, the Hop Test can be used and should be 85% of the uninvolved side before progression. As you can see, there is a lot of information regarding the management of ACL injuries, a lot of which is contradictory. You will see many variations of protocols based on the surgeon. Some important basic information to guide your program are the tissue healing time and achievement of the previously listed goals. Whenever you're unsure regarding the development of your treatment program, be sure to consult with another clinician or the surgeon that worked on the patient. What are your thoughts on ACL rehabilitation? Do you have any other interesting evidence? References:
Abbas MM, Abulaban AA, Darwish HH. (2013). Functional outcomes of bone tendon bone versus soft tissue arthroscopic anterior cruciate ligament reconstruction. A comparative study. Saudi Med J;34(2):153-60. Web. 23 Feb 2013. Adams D, et al. (2012). Current concepts for Anterior Cruciate Ligament Reconstruction: A Criterion Based Rehabilitation Progression. JOSPT; 42(7): 601-614. Web. 18 Feb 2013. Baltaci G, Yilmaz G, Atay AO. (2012). The outcomes of anterior cruciate ligament reconstructed and rehabilitated knees versus healthy knees: a functional comparison. Acta Orthop Traumatol Turc;46(3):186-95. Web. 23 Feb 2013. Dave LY, Leong OK, Karim SA, Chong CH. (2013). Tunnel enlargement 5 years after anterior cruciate ligament reconstruction: a radiographic and functional evaluation. Eur J Orthop Surg Traumatol. Web. 24 Feb 2013. Escamilla RF, Macleod TD, Wilk KE, Paulos L, Andrews JR. (2012). Cruciate Ligament Loading During Common Knee Rehabilitation Exercises. Proc Inst Mech Eng H.;226(9):670-80. Web. 23 Feb 2013. Feller J, Webster KE. (2013). Return to sport following anterior cruciate ligament reconstruction. Int Orthop.;37(2): 285-90. Web. 24 Feb 2013. Frank JS, Gambacorta PL. (2013). Anterior cruciate ligament injuries in the skeletally immature athlete: diagnosis and management. J Am Acad Orthop Surg.;21(2):78-87. Web. 24 Feb 2013. Hewett TE, Di Stasi SL, Myer GD. (2013). Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013 Jan;41(1):216-24. Web. 24 Feb 2013. Kruse LM, Gray B, Wright RW. (2012). Rehabilitation after anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 3;94(19): 1737-48. Web. 24 Feb 2013. Lepley LK, Palmieri-Smith R. (2012). Effect of Eccentric Strengthening Following Anterior Cruciate Ligament Reconstruction on Quadriceps Strength. J Sport Rehabil. Web. 24 Feb 2013. Kim KM, Croy T, Hertel J, Saliba S. (2010). Effects of neuromuscular electrical stimulation after anterior cruciate ligament reconstruction on quadriceps strength, function, and patient-oriented outcomes: a systematic review. J Orthop Sports Phys Ther.;40(7):383-91. Web. 24 Feb 2013. Lobb R, Tumilty S, Claydon LS. (2012). A review of systematic reviews on anterior cruciate ligament reconstruction rehabilitation. Phys Ther Sport.;13(4):270-8. Web. 23 Feb 2013. Magnussen RA, Pedroza AD, Donaldson CT, Flanigan DC, Kaeding CC. (2013). Time from ACL injury to reconstruction and the prevalence of additional intra-articular pathology: is patient age an important factor? Knee Surg Sports Traumatol Arthrosc. Web. 24 Feb 2013. Manske, Robert C. Postsurgical Orthopedic Sports Rehabilitation: Knee & Shoulder. St. Louis, MO: Mosby Elsevier, 2006. 176-177, 191-192. Print. Markatos K, Kaseta MK, Lallos SN, Korres DS, Efstathopoulos N. (2012). The anatomy of the ACL and its importance in ACL reconstruction. Eur J Orthop Surg Traumatol. Web. 17 Feb 2013. Muller B, Bowman KF Jr, Bedi A. (2013). ACL graft healing and biologics. Clin Sports Med.; 32(1):93-109. Web. 23 Feb 2013. Neumann, Donald. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation. 2nd edition. St. Louis, MO: Mosby Elsevier, 2010. 535. Print. Nyland J, Mauser N, Caborn DN. (2013). Sports involvement following ACL reconstruction is related to lower extremity neuromuscular adaptations, subjective knee function and health locus of control. Knee Surg Sports Traumatol Arthrosc. Web. 24 Feb 2013. Pan X, Wen H, Wang L, Ge T. (2012). Bone-patellar tendon-bone autograft versus LARS artificial ligament for anterior cruciate ligament reconstruction. Eur J Orthop Surg Traumatol. Web. 24 Feb 2013. Papandreou M, Billis E, Papathanasiou G, Spyropoulos P, Papaioannou N. (2012). Cross-Exercise on Quadriceps Deficit after ACL Reconstruction. J Knee Surg. Web. 24 Feb 2013. Rabuck SJ, Baraga MG, Fu FH. (2013). Anterior cruciate ligament healing and advances in imaging. Clin Sports Med.; 32(1):13-20. Web. 23 Feb 2013. Shelbourne KD, Freeman H, Gray T. (2012). Osteoarthritis after anterior cruciate ligament reconstruction: the importance of regaining and maintaining full range of motion. Sports Health. 2012 Jan;4(1):79-85. Web. 24 Feb 2013. Silverwood R, Gordon JB, Baron R, Walmsley P, Watson J, Wood AM. (2012). Cyclops Lesions in Military Personnel: a reason for delayed return to fitness post anterior cruciate ligament reconstruction. J R Nav Med Serv; ;98(3):3-5. Web. 23 Feb 2013. Sutton KM, Bullock JM. (2013). Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg.;21(1):41-50. Web. 24 Feb 2013. Van Ginckel A, Verdonk P, Victor J, Witvrouw E. (2013). Cartilage Status in Relation to Return to Sports After Anterior Cruciate Ligament Reconstruction. Am J Sports Med. Web. 24 Feb 2013. Wilk, K. (Performer) (2012). Current concepts in the treatment of acl injuries parts 1-3. Rehab Webinars. [Audio podcast]. Retrieved from www.rehabwebinars.com Xu M, Gao S, Zeng C, Han R, Sun J, Li H, Xiong Y, Lei G. (2013). Outcomes of Anterior Cruciate Ligament Reconstruction Using Single-Bundle Versus Double-Bundle Technique: Meta-analysis of 19 Randomized Controlled Trials. Arthroscopy.;29(2):357-65. Web. 24 Feb 2013. Zelić Z, Jovanović S, Wertheimer V, Sarić G, Biuk E, Gulan G. (2012). Results of surgical reconstruction of the anterior cruciate ligament. Coll Antropol;36(1):201-6. Web. 23 Feb 2013. Zhu W, Wang D, Han Y, Zhang N, Zeng Y. (2012). Anterior cruciate ligament (ACL) autograft reconstruction with hamstring tendons: clinical research among three rehabilitation procedures. Eur J Orthop Surg Traumatol. Web. 24 Feb 2013.  Introduction: The Achilles tendon is exposed to high levels of stress during locomotion and movement. Because high forces are transmitted through this tendon, continuous physical stresses degrade and degenerate the structural integrity of the Achilles. Ruptures are most commonly seen 2-5 cm above the calcaneal joint. The ruptures most likely occur between the 3rd and 5th decade of life and 25%-30% are seen bilaterally. Although high activity and sports are correlated with an Achilles tendon rupture, "incidence of Achilles tendon ruptures in recreationists amounts to 61% (Grubor 2012)." Decreased tendon strength, increased physical activity, past history of corticosteroids, and previous history of trauma have all been attributed to possible causes. Anatomy: According to Ding et al, the Achilles tendon is about 15 in. long and has attachments at the calcaneal tuberosity and the lower 1/3 of the calf. The tendon is vascularized and has no sheath, so the reticular tissue connects it to the aponeurosis. Three muscles contribute to the Achilles tendon: gastrocnemius, soleus, and plantaris. Origin: -Gastrocnemius: (medial head) proximal and posterior part of the medial condyle and adjacent part of the femur, capsule of the knee joint; (lateral head) lateral condyle and posterior surface of the femur, capsule of the knee joint -Soleus: posterior surfaces of the head of the fibula and proximal 1/3 of its body, soleal line and middle 1/3 of the medial border of the tibia, and tendinous arch between the tibia and fibula -Plantaris: distal part of the lateral supracondylar line of the femur, adjacent part of its popliteal surface and oblique popliteal ligament of knee joint. Insertion: -All muscles join together to form the Achilles tendon and insert into the posterior surface of the calcaneus Action: -All 3 muscles plantarflex the ankle, but the plantaris and gastrocnemius aid in flexing the knee as well Innervation: -Tibial Nerve Clinical Presentation: Patients with a ruptured Achilles tendon will complain of intense pain at the time of injury, palpable indentation in the Achilles region, and a loss of plantarflexion strength. As stated above, patients aged 30-40 years have the highest incidence with men being injured more frequently than women 5:1 (Mezzarobba, 2012). The patient will have a positive calf squeeze test, and results can be confirmed using ultrasound imaging (calf squeeze test is also known as the Thompson Test). Ultrasound has been shown to be highly sensitive and specific (Grubor 2012). Additionally, patients will perform poorly with the heel rise involved in the MMT of the plantarflexors. Surgical Management: It is a common debate whether conservative treatment or surgical management is the most effective treatment in patients with a ruptured achilles tendon. One of the primary reasons that surgical repair is often chosen over the conservative approach is the hypothesis that surgical repair reduces the likelihood of Achilles tendon re-rupture. Soroceanu et al performed a meta-analysis of RCTs and found no difference in re-rupture rate between surgical repair and non-surgical approaches, so long as early ROM was performed. No significant difference was found between the groups for calf circumference, ROM, and functional outcomes as well. If the conservative group patients did not perform early ROM, surgical repair was found to be superior. With the risks surgery places on the patient, such as infection, it is important to educate clients on all options of care. It is also important to examine the effects different surgical techniques have in order to continue developing the best plan of care for the patient. Mezzarobba et al. reviewed the results of a percutaneous repair of the Achilles tendon using Tenolig. Interestingly, the authors found several changes to the involved limb. Increased dorsiflexion ROM was noted due to lengthening of the muscle, along with calf atrophy, which leads to decreased plantarflexion strength. The quadriceps volume was found to increase as well due to the compensation resulting from calf atrophy. It is still under debate as to the effectiveness of nonoperational treatment vs. surgical management (Krapf et al., 2012). There are of course various surgical styles for the repair of an Achilles tendon: open repair vs. minimally invasive (percutaneous) repair. For awhile, it was theorized that the minimally invasive approach would decrease complications and accelerate rehabilitation; however, no significant difference was found between the two approaches (Kolodzielj et al, 2012). Additionally, it was shown that immediate weight-bearing and range of motion were necessary to improve outcomes. Lack of weight bearing led to impairments, such as muscle strength, endurance, and activity. When comparing open repair to mini-open repair for Achilles tendon rupture, a significant difference was found for start times for rehab (open repair: 37 days, mini-open repair: 19 days) and return to activity (open repair: 7 months, mini-open repair: 5 months) (Klein et al, 2012). Following surgical repair of the Achilles tendon, some patients experience a tendinopathy-like pain. The standard eccentric exercises or endoscopic Achilles tenolysis have been found to be sufficient in reducing the pain (Liu, 2013). Following surgery, the traditional model was to immobilize the limb in a cast/boot for 6-8 weeks in order to protect the healing tendon; however it was found that mobility can occur as early as 10 days following surgery and improve the apposition of the tendon (Soroceanu et al, 2012). One study looked at the effect early mobility has on open repair vs. non-surgical management. Initially, Achilles tendons that underwent open repair were found to be superior in their ability to withstand biomechanical loads compared to nonoperational approaches. These differences disappeared at 8 weeks. The conservative group was found to have greater histological characteristics and tendon lengthening. At the end of the study, no functional difference was noted between the groups. While these results may be surprising, it must be noted that the study used rats in the assessment and cannot be directly correlated with human reactions. The implications of this study must be further explored under human subjects before the results can be considered in rehabilitation principles.
References:
Ding W, Yan W, Zhu Y, Liu Z. (2012). Treatment of acute and closed Achilles tendon ruptures by minimally invasive tenocutaneous suturing. Ulus Travma Acil Cerrahi Derg., 18(5):405-10. Web. 12 Jan 2012. Grubor P, Grubor M. (2012). Treatment of Achilles tendon rupture using different methods. Vojnosanit Pregl, 69.8: 663-668. Web. 22 Dec 2012. Kendall FP, McCreary EK, Provance PG, Rodgers MM, & Romani WA. (2005). Muscles: Testing and Function with Posture and Pain. (5th ed., pp. 414-415). Baltimore: Lippincott Williams & Wilkins. Klein EE, Weil L Jr, Baker JR, Weil LS Sr, Sung W, Knight J. (2012). Retrospective Analysis of Mini-Open Repair Versus Open Repair for Acute Achilles Tendon Ruptures. Foot Ankle Spec. Web. 12 Jan 2013. Kołodziej L, Bohatyrewicz A, Kromuszczyńska J, Jezierski J, Biedroń M. (2012). Efficacy and complications of open and minimally invasive surgery in acute Achilles tendon rupture: a prospective randomised clinical study-preliminary report. Int Orthop. Web. 12 Jan 2013. Krapf D, Kaipel M, Majewski M. (2012). Structural and biomechanical characteristics after early mobilization in an Achilles tendon rupture model: operative versus nonoperative treatment. Orthopedics, 35(9):e1383-8. Web. 8 Jan 2013. Lui TH. (2013). Endoscopic Achilles Tenolysis for Management of Heel Cord Pain after Repair of Acute Rupture of Achilles Tendon. J Foot Ankle Surg., 52(1):125-7. Web. 12 Jan 2013. Mezzarobba S, Bortolato S, Giacomazzi A, Fancellu G, Marcovich R, Valentini R. (2012). Percutaneous repair of Achilles tendon ruptures with Tenolig: Quantitative analysis of postural control and gait pattern. Foot (Edinb), 22(4):303-9. Web. 8 Jan 2013. Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. (2012). Surgical versus nonsurgical treatment of acute achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am, 94(23):2136-43. Web. 12 Jan 2013. |
Copyright © The Student Physical Therapist LLC 2023

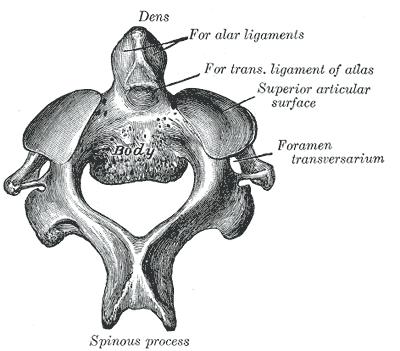
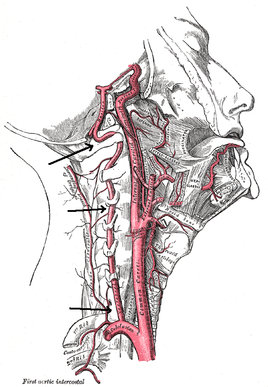
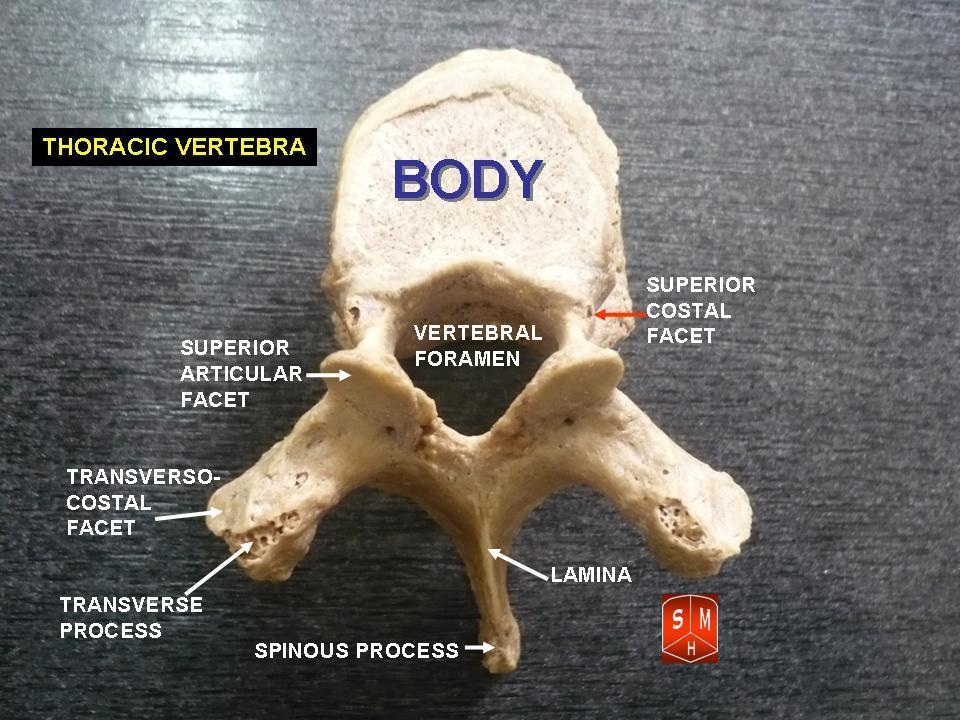
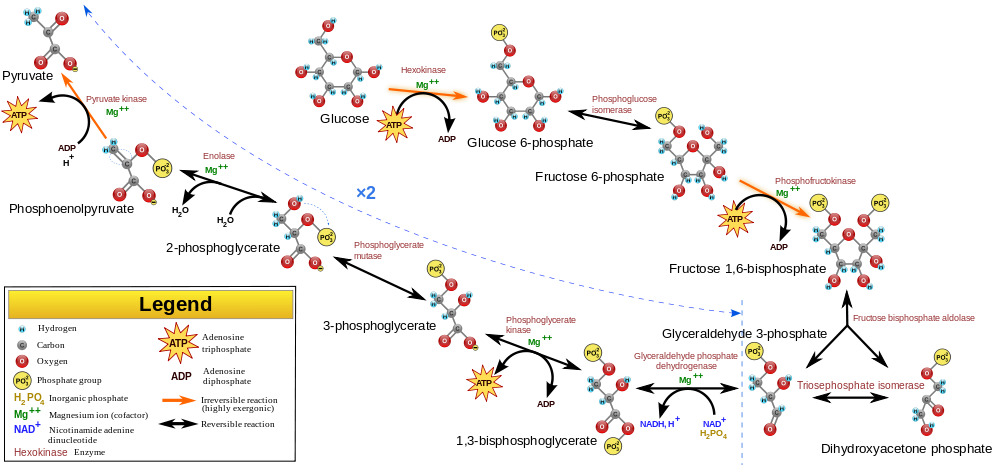
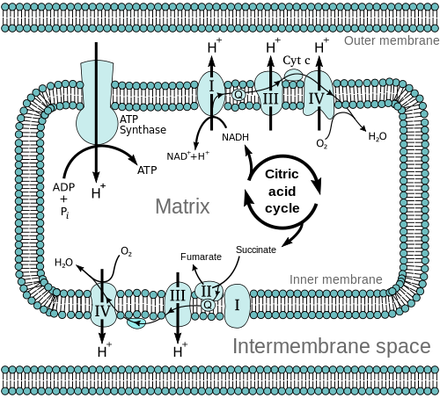


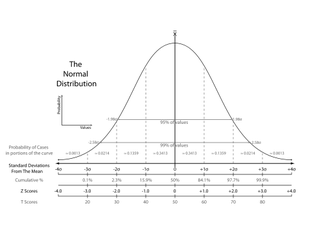
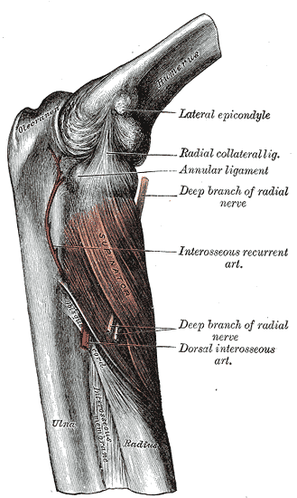


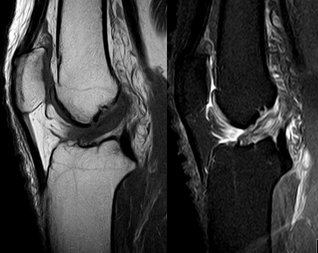
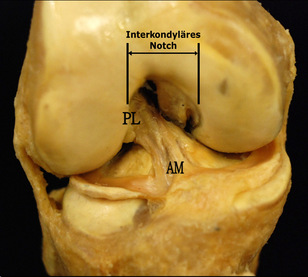


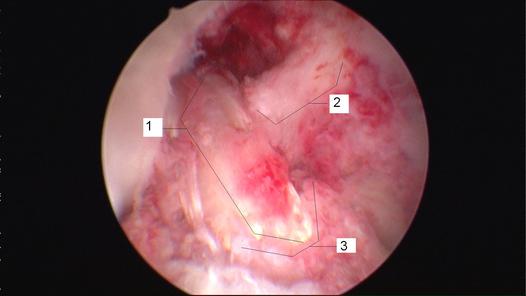



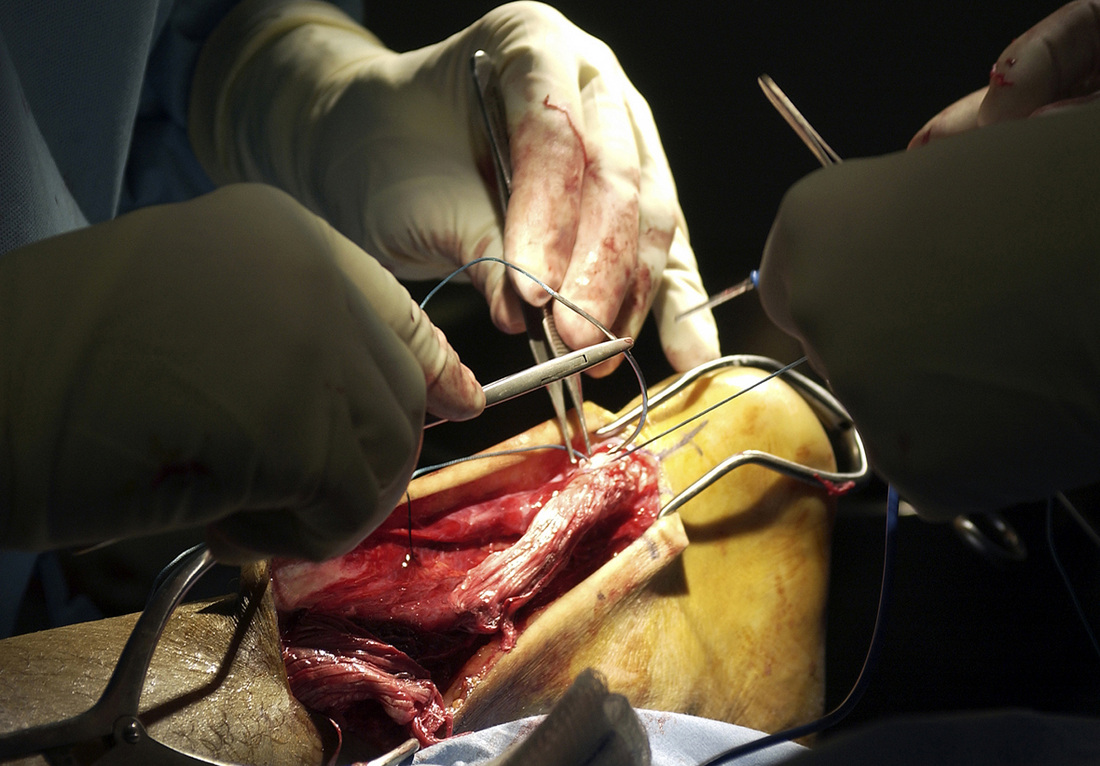
 RSS Feed
RSS Feed