- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
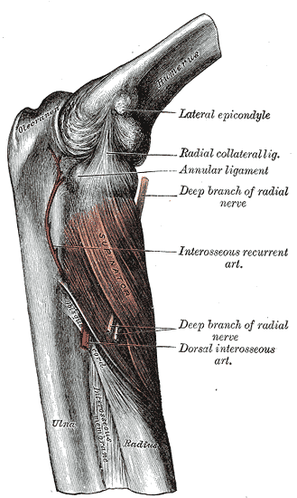
 Posterior Interosseous Nerve (PIN) Syndrome is a pathology that involves pain and/or motor weakness as a result of nerve compression. In parts of the medical community, Radial Tunnel Syndrome and PIN Syndrome are one in the same, while in other parts they are different diagnoses with the same nerve involvement (Posterior Interosseous Nerve). These health care professionals identify Radial Tunnel Syndrome as pain along the radial tunnel, while PIN Syndrome is marked weakness in the muscles innervated by the Posterior Interosseous Nerve. Due to the fact that both syndromes involve compression of the same nerve, often by the same structures, we will use the terms PIN Syndrome and Radial Tunnel Syndrome synonymously in this review, especially due to the fact that the two are managed identically.
Pathogenesis: Since the posterior interosseous nerve is a motor nerve, it may appear confusing as to why pain is often a complaint. One of the hypotheses for this pain syndrome is that the PIN also carries some afferent fibers that include C-fibers, which are relatively smaller compared to the motor component. Thus, compression would elicit pain, while still demonstrating the normal EMG findings of the larger motor component. (Naam & Nemani, 2012). Lubahn & Cermak state that the pressure disrupts local blood flow or axoplasmic flow in the nerve, thus, producing the pain we see in our patients. However, Portilla Molina et al claim that the PIN also carries sensory and proprioception fibers to the posterior capsule of the wrist (we must remember that this cadaveric study is from 1998 as well). This goes against what most of the literature reports, but should still be kept in mind as our understanding of the diagnosis continues to develop. The PIN may be compressed by the arcade of Frohse, other tissues of the supinators, the leash of Henry from the radial artery, and the edge of the ECRB muscle (Ducic et al, 2012). The arcade of Frohse is an anatomical variant that is found in about 30-50% of the population and is located at the proximal edge of the supinator (Andreisek et al, 2006). It is a fibrous adhesion that connects the brachialis and brachioradialis muscles. Tsai & Steinberg use the acronym FREAS to identify potential sites of constriction: -F: fibrous bands about the radiocapitellar joint -R: radial (artery) recurrent branches -E: extensor carpi radialis brevis muscle -A: arcade of Frohse -S: distal edge of supinator Portilla Molina et al hypothesize that the PIN is fixed in the supinator muscle and becomes elongated and compressed with pronation/supination. This suggests that PIN Syndrome is a pathology based on repetition (and it can be), but injury to the nerve can also be from a traumatic nature as well (Sueki & Brechter, 2010). While this classification system is rarely used with entrapment pathologies, classification can be made based upon the severity of injury and potential for healing. As the nerve can demonstrate severe thinning/thickening at the sites of compression, these classification levels may still prove useful: -First-Degree Neuropraxia: disruption of myelin around the Nodes of Ranvier resulting in temporary loss of nerve conduction with rapid recovery usually. -Second-Degree Axonotmesis: interruption of axon with resulting wallerian degeneration. The tissue around the axon is still intact. Full recovery is possible, but time for recovery depends on distance between the injury and the target structure. -Third-Degree Neurotmesis: disruption of the nerve and its supporting structures, especially the endoneurium. The perineurium and epineurium are still intact. -Fourth-Degree Neurotmesis: all parts of the nerve are destroyed except the epineurium. -Fifth-Degree Neurotmesis: completely severed nerve with no potential for regeneration. Clinical Presentation: Pain is typically present at the proximal dorsoradial aspect of the forearm and is increased with forearm rotation. Muscle weakness may be present as well (or instead) as a result of either pain inhibition or compression of the motor nerve (Naam & Nemani, 2012). Along with forearm rotation, forceful elbow extension may produce pain (Ducic et al, 2012). As stated earlier, compression may also lead to weakness in the muscles innervated by the PIN. Patients with PIN Syndrome will have a negative Tinel's sign, due to the fact that the Posterior Interosseous Nerve is a motor nerve (Andreisek et al, 2006). Patients often have difficulty maintaining finger extension, and following finger extension, you will see the fingers quickly drop back into flexion. You may also see radial deviation with wrist extension due to weakness of the extensor carpi ulnaris. If weakness is noted in the extensor carpi radialis longus/brevis or brachioradialis, the clinician should suspect a more proximal compression of the nerve (Tsai & Steinberg, 2008). Tsai & Steinberg found that 5% of patients with lateral epicondylopathy also suffer from Radial Tunnel Syndrome. Kalb et al found that 52% of patients with PIN compression had lateral epicondylopathy as well. As you can see, it's important to screen for both in patients with elbow pain. PIN Syndrome is typically due to overuse (athletes and violinists especially), external compression (such as with crutch use), radial head fracture, soft tissue tumors, and more (Andreisek et al, 2006). Certain job activities have been shown to have a link to development of Radial Tunnel Syndrome, such as handling tools with full extension of the elbow (Naam & Nemani, 2012). Using a force of at least 1 kg more than 10x/hour with the elbow extended between 0-45 degrees with frequent pronation/supination has been shown to have increased incidence of developing Radial Tunnel Syndrome. Diagnosis: One of the more distinguishing signs in diagnosing Radial Tunnel Syndrome is tenderness over the anatomical landmark of the Posterior Interosseous Nerve, 3-5 cm distal to the lateral epicondyle (Naam & Nemani, 2012). It should be noted that there is controversy surrounding the diagnosis of Radial Tunnel Syndrome due the lack of objective findings. Pain should not be increased with resisted wrist extension. Due to the proximity of the lateral epicondyle, it is important to differentiate between Lateral Epicondylopathy and Radial Tunnel Syndrome, especially since they often occur together. Local anesthetic injection can be used to aide in differentiating between these two. Lateral Epicondylopathy will be relieved by injection of an anesthetic, while Radial Tunnel Syndrome rarely has any changes. We must also be sure to check for potential cervical radiculopathy (Sueki & Brechter, 2010). In fact, there is some controversy in the literature regarding cervical radiculopathy being an ignition for Radial Tunnel Syndrome (or any upper extremity nerve entrapment); this is known as Double Crush Syndrome. The Radial Neural Tension Test will be especially useful in these cases, but may be positive with any Radial Nerve-related entrapment as well. Other potential causes of peripheral neuritis include polyarteritis, rheumatological disorders, and post-systemic illness angioneuropathy and should be considered during your differential diagnosis. When diagnosing Radial Tunnel Syndrome, be sure to rule out extensor tendon ruptures, sagittal band ruptures, and inflammatory involvement of the MCP joints as these can all have a similar clinical presentation. One suggested method of diagnosing RTS involves drawing 9 squares over the anterior forearm for location of pain. Tenderness in the lateral 3 squares supposedly is linked to RTS (Loh et al, 2004). Clinically, we may see production of pain with resisted supination in full elbow extension or pain with passive elbow extension with wrist flexion and pronation (Lubahn & Cermak, 1998). Some literature recommends the use of middle finger resisted extension to identify Radial Tunnel Syndrome, but due to the attachment at the lateral epicondyle, there remains the potential for false positives (Sueki & Brechter, 2010). As with most pathologies, the earlier the diagnosis, the better the outcomes. According to Adreisek et al, MRI can be useful in diagnosing Radial Tunnel Syndrome as well. It is well known that MRI is capable of identifying mass lesions, nerve enlargements, and neuritis. Also, signal intensity changes in the muscle, in particular muscle edema, is often used in diagnosis due to the difficulty involved with identifying changes in the nerve itself. The MRI is not useful in identifying patients with PIN Syndrome by locating the compressing structures. Instead, diagnosis is based on the pattern of muscle denervation. With Radial Tunnel Syndrome, the supinator, extensor digitorum, extensor carpi ulnaris, extensor digiti minimi, abductor pollicis longus, extensor pollicis longus/brevis, and extensor indicis may have abnormal signal intensity while the extensor carpi radialis muscles are normal. One would think that nerve conduction velocity tests and EMGs would be used widely, however, due to the lack of established diagnostic guidelines, there is rarely a large enough drop to be clinically useful. You might expect a conduction block or prolongation of radial nerve conduction; however, one theory for the lack of changes is that the testing is often done in neutral forearm position, where changes in conduction do not always occur (Portilla Molina et al, 1998). Martinoli et al reviewed the use of sonograms in diagnosing Radial Tunnel Syndrome. According to the authors, high resolution sonograms are able to identify compression of the Posterior Interosseous Nerve by the supinator. The nerve may appear swollen and hypoechoic from edema, segments of thinning and thickening, or encased by scar tissue at the distal edge of the supinator. Conservative Treatment: Conservative treatment typically consists of a variety of interventions: wrist splinting, activity modification, NSAIDs, and exercise (Naam & Nemani, 2012). A wrist cock-up splint may be useful by slackening the wrist extensors (and thus decreasing pressure in the radial tunnel) (Lubahn & Cermak, 1998). Tsai & Steinberg recommend beginning treatment with wrist/elbow splints, NSAIDs, and restriction of aggravating activities. Wrist flexion and pronation combined with elbow extension should be avoided, along with any position that aggravates symptoms. Due to the compressive nature of the pathology, the clinician should consider including soft tissue release work, myofascial release work and neural mobilization techniques (Sueki & Brechter, 2010). 72% of patients had been shown to improve following a single injection of 40 mg of triamcinolone and 2 mL of 1% lidocaine at 6 weeks, but we should consider the fact that this study contained a low number of participants. According to Lubahn & Cermak, a cortisone shot around, not into, the nerve should be considered as well. Should symptoms not improve within 90 days, the surgical approach should be considered due to the low likelihood of spontaneous recovery. After 18 months of symptoms, muscle fibrosis occurs (an irreversible condition). Surgical Treatment: Lengthening the supinator has been shown to lower the pressure inside the radial tunnel, while lengthening the extensor carpi radialis brevis and extensor digitorum communis had no effect (Naam & Nemani, 2012). The Dorsal (Henry) Approach involves exposing and pushing aside the sensory nerves, arteries, and uninvolved muscles (brachioradialis, extensor carpi radialis brevis/longus before dividing the arcade of Frohse and superficial portion of the supinator muscle. Bupivacaine is injected before dressing application. The Transmuscular Brachioradialis-Splitting Approach involves just what you would think, splitting the muscle fibers and overlying fascia before exposing the radial nerve, at which point the supinator and arcade of Frohse are divided. The Dorsal Approach Between Brachioradialis and Wrist Extensors involves indentifying and developing the interval between the brachioradialis and extensor carpi radialis longus in order to expose the arcade of Frohse. The Anterior Approach is used for when there is proximal compression as well as distal. The process involves exposing the radial nerve between the brachialis and brachioradialis then following the nerve distally until it branches to the superficial radial nerve and PIN. Here the arcade of Frohse is released, the arteries are ligated, and the entire supinator is released as well. Both the Anterior and Posterior Approaches carry the risk of damaging the PIN due to the proximity of the incision, so precision is a necessity (Mekhail et al, 1995). Ducic et al discusses an endoscopic nerve release the requires a shorter incision length. This could potentially lead to better outcomes and only requires a simple lighted retractor to help expose the desired tissue structures. General post-op care involves AROM beginning 3-5 days after surgery, strengthening at weeks 3-4, return to limited duty at work during weeks 2-3, and return to full duty at 4-6 weeks. Lubahn & Cermak recommend using a long-arm posterior splint with the wrist in neutral position with gradual ROM progression beginning 1 week after surgery, focusing on stretching the extensor muscles. Return to prior level of function may take 6-12 weeks. References:
Andreisek G, Crook DW, Burg D, Marincek B, Weishaupt D. (2006). Peripheral neuropathies of the median, radial, and ulnar nerves: MR imaging features. Radiographics. 2006 Sep-Oct;26(5):1267-87. Web. 10 May 2013. Ducic I, Felder JM 3rd, Quadri HS. (2012). Common nerve decompressions of the upper extremity: reliable exposure using shorter incisions. Ann Plast Surg. 2012 Jun;68(6):606-9. Web. 05 May 2013. Kalb K, Gruber P, Landsleitner B. (1999). [Compression syndrome of the radial nerve in the area of the supinator groove. Experiences with 110 patients]. Handchir Mikrochir Plast Chir. 1999 Sep;31(5):303-10. Web. 11 May 2013. Loh YC, Lam WL, Stanley JK, Soames RW. (2004). A new clinical test for radial tunnel syndrome--the Rule-of-Nine test: a cadaveric study. J Orthop Surg (Hong Kong). 2004 Jun;12(1):83-6. Web. 11 May 2013. Lubahn JD, Cermak MB. (1998). Uncommon nerve compression syndromes of the upper extremity. J Am Acad Orthop Surg. 1998 Nov-Dec;6(6):378-86. Web. 11 May 2013. Martinoli C, Bianchi S, Pugliese F, Bacigalupo L, Gauglio C, Valle M, Derchi LE. (2004). Sonography of entrapment neuropathies in the upper limb (wrist excluded). J Clin Ultrasound. 2004 Nov-Dec;32(9):438-50. Web. 11 May 2013. Mekhail AO, Ebraheim NA, Jackson WT, Yeasting RA. (1995). Vulnerability of the posterior interosseous nerve during proximal radius exposures. Clin Orthop Relat Res. 1995 Jun;(315):199-208. Web. 12 May 2013. Naam NH, Nemani S. (2012). Radial tunnel syndrome. Orthop Clin North Am. 2012 Oct;43(4):529-36. Web. 01 May 2013. Portilla Molina AE, Bour C, Oberlin C, Nzeusseu A, Vanwijck R. (1998). The posterior interosseous nerve and the radial tunnel syndrome: an anatomical study. Int Orthop. 1998;22(2):102-6. Web. 12 May 2013. Sueki D & Brechter J. Orthopedic Rehabilitation: Clinical Advisor. Maryland Heights, MO: Mosby Elsevier, 2010. 751-752. Print. Tsai P, Steinberg DR. (2008). Median and radial nerve compression about the elbow. J Bone Joint Surg Am. 2008 Feb;90(2):420-8. 11 May 2013.
2 Comments
5/14/2024 12:34:50 pm
Financial services encompass a wide array of offerings catering to individuals, businesses, and institutions. From banking and investments to insurance and wealth management, the sector plays a pivotal role in global economies. Amidst this landscape, exemplary customer service stands as a hallmark. Companies like Cardone Capital prioritize client satisfaction, setting the bar high with their commitment to excellence. Cardone Capital customer service exemplifies this dedication, providing personalized assistance, timely resolutions, and a seamless experience. In an industry reliant on trust and reliability, their emphasis on customer-centric practices fosters long-term relationships and solidifies their reputation as a trusted partner in financial endeavors.
Reply
Leave a Reply. |



 RSS Feed
RSS Feed