- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 Currently the doctor of physical therapy degree consists of 3 years of education with both clinical and didactic components interspersed within these 3 years. Many students are paying thousands of dollars to be enrolled in an institution even when they are absent from their school almost 1/3 of this time. Yes, the school is working to place students in clinical affiliations and someone is "grading" your performance out in the clinic, but for many students the costs do not seem to add up. To add insult injury, with lower reimbursement rates and the tightening of federal regulations, physical therapists are not being compensated adequately once they enter the professional world. In this post, John Childs discusses where he believes the future of physical therapy education needs to head. Several schools are already doing longer clinical affiliations where students are receiving scholarships or payment for their services. Mr. Childs also poses the idea of these longer clinical rotations transforming into a post professional residency model. In this model, students would sit for the NPTE after 2 years of schooling and complete a 1 year residency program, similar to medical school. Heathcare policies and models are rapidly changing, will physical therapy education be on target for this change as well? What are your thoughts?
4 Comments
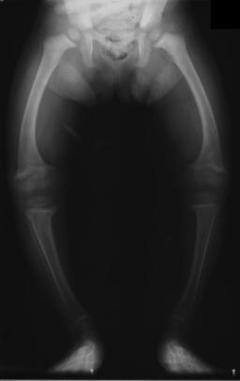 We were recently asked about treatment methods for genu varum of the knee, so we thought we would do a little literature review on the subject. We believe the request was directed towards an exercise-based approach. Unfortunately, we were unable to find much evidence regarding treating genu varum with exercise. With genu varum, the line of gravity runs farther medial to the knee than normal, putting increased stress on the medial compartment of the knee. This puts the individual at risk for developing OA. Due to the increased risk in developing unicompartmental osteoarthritis, it is desireable for the patient to restore normal alignment in order to delay the need of having a Total Knee Replacement. There are several methods of managing genu varum right now, which we will briefly review. The traditional method of treating genu varum involved an osteotomy of the proximal tibia with the goal of restoring normal knee alignment. Goutallier et al found a desirable range for realignment: 3-6 degrees of valgus. At < 3 degrees of valgus, individuals developed recurrent genu varus, while at > 6 degrees of valgus, individuals developed deterioration of the lateral tibiofemoral joint. A newer method that is currently being developed is known as the llizarov method (Park et al, 2012). During the osteotomy, the surgeon also places an external fixator on the patient. This allows gradual adjustments to be made to the knee alignment during the 24 weeks it remained on. While the method was able to restore normal alignment to the knee, there was a high level of complications to the patients. An alternative method of treating genu varum includes bracing and heel wedges. The brace under discussion is called a compartmental unloader. An individual with genu varum would want a valgus orthosis. It functions by either having a valgus stress built into it or the ability to develop the stress while donning the orthosis. With the valgus stress placed on the knee, the natural varus moment decreases, lowering the stress on the medial tibiofemoral joint. This hopefully delays the need for a Total Knee Replacement. Both a compartmental unloader and a lateral heel wedge have been shown to be effective as short-term pain relief methods (Brouwer et al, 2005). This can play a role in at least delaying the need for a Total Knee Replacement (Wilson et al, 2011). Additionally, we must consider what mechanical issues may be predisposing a patient to genu varum alignment. It is well documented that abnormal strength of the hip muscles can alter knee mechanics. Strengthening the hip external rotators and hip extensors, for example, is a key component in the rehabilitation of patients with patellofemoral pain syndrome. Zeni and Synder-Mackler discuss the importance of strengthening the contralateral limb following a total knee replacement. They also report that decreasing body mass may have an impact on forces across the knee following replacement. Other authors discuss quadriceps strength as an important measurement to consider when viewing the success of a total knee replacement. There are examples across the literature that stress the importance of a lower limb strengthening and endurance program to decrease stresses at the knee to help prolong total joint replacements. While there may not be direct evidence linking hip strengthening programs to decreasing genu varum alignment, hip strength is definitely a measure to address when working with this population. Again, unfortunately, we were unable to find much evidence on exercise as a treatment for genu varum. What about you, what has your research and experience shown in addressing the condition? References:
Brouwer RW, Jakma TS, Verhagen AP, Verhaar JA, Bierma-Zeinstra SM. (2005). Braces and orthoses for treating osteoarthritis of the knee. Cochrane Database Syst Rev. ;(1):CD004020. Web. 28 Jan 2013. Goutallier D, Hernigou P, Medevielle D, Debeyre J. (1986). Outcome at more than 10 years of 93 tibial osteotomies for internal arthritis in genu varum (or the predominant influence of the frontal angular correction. Rev Chir Orthop Reparatrice Appar Mot.;72(2):101-13. Web. 28 Jan 2013. Park YE, Song SH, Kwon HN, Refai MA, Park KW, Song HR. (2012). Gradual correction of idiopathic genu varum deformity using the Ilizarov technique. Knee Surg Sports Traumatol Arthrosc. Web. 28 Jan 2013. Wilson B, Rankin H, Barnes CL. (2011). Long-term results of an unloader brace in patients with unicompartmental knee osteoarthritis. Orthopedics. ;34(8):e334-7. Web. 28 Jan 2013. Zeni J, Synder-Mackler L. (2010). Early post-operative measures predict 1- and 2- year outcomes after unilateral total knee arthroplasty: importance of contralateral limb strength. Journal of the American Physical Therapy Association.; 90(1): 43-54. Web. 29 Jan 2013.
 In the article Evaluation of an Injured Runner, Magrum and Wilder discuss several interesting points to consider when working with an injured runner. First, you must examine the entire kinetic chain. Running is truly a full body movement, which requires symmetry between the upper and lower extremities. Forces are transmitted from one area to the next, and excessive movement in one region can create dysfunction down the chain. When working with this population, do not undermine the importance of a thorough history. Be sure to inquire about shoe type, weekly mileage, length of runs, running surface, and more. Because running is such a repetitive activity, the examiner needs to understand exactly when the pain occurs, where is occurs, and if symptoms persists or subside after exercise. Following a subjective history, they recommend beginning the evaluation in standing. Static posture is observed and any asymmetries are noted. Specifically look at patellar alignment, subtalar position, and sacroiliac joint motion. As the evaluation moves from standing to sitting, ligament stress testing of the knee can be performed as well as reflexes, neural tensioning tests, and a vascular screening. Additionally, note how the patella tracks as the patient actively extends at the knee. Next, have the patient lie in supine. It is important to assess for a potential leg length discrepancy (clues from the standing and sitting evaluation can point toward a potential leg length issue). In supine, femoral torsion, tibial torsion, and the Q-angle can all be appropriately assessed. The article continues on to discuss the sidelying evaluation and functional tests that should be performed when assessing a runner. Additionally, normal angles, pictures, and a review on how to perform different examination measures are outlined in the article. It is a great review for anyone, especially if you are expecting to evaluate a runner in the near future.
 While the thoracic spine is often not the source of a patient's symptoms, decreased mobility in this region can create problems up and down the chain. For example, in his book Movement, Gray Cook discusses the importance of thoracic mobility when assessing scapular stability. Additionally, mobility of the ribs, breathing pattern, and referred pain from the cervical spine must all be considered when working with the thoracic spine. In this post from Dr. E, he discusses several innovative techniques to mobilize the thoracic spine. Below is a direct link to the video.  Introduction: The Achilles tendon is exposed to high levels of stress during locomotion and movement. Because high forces are transmitted through this tendon, continuous physical stresses degrade and degenerate the structural integrity of the Achilles. Ruptures are most commonly seen 2-5 cm above the calcaneal joint. The ruptures most likely occur between the 3rd and 5th decade of life and 25%-30% are seen bilaterally. Although high activity and sports are correlated with an Achilles tendon rupture, "incidence of Achilles tendon ruptures in recreationists amounts to 61% (Grubor 2012)." Decreased tendon strength, increased physical activity, past history of corticosteroids, and previous history of trauma have all been attributed to possible causes. Click here to continue reading  If you're anything like us, direct access can be a confusing term, often misused around the physical therapy clinic. As students, patients ask us why it is important for us to be earning a doctorate degree. Somewhere in the answer the terms "direct access, autonomous care, primary care providers, and differential diagnosis" are jumbled out. Many patients are confused by the extent of these terms. As practitioners, we need to do a better job answering difficult questions like this one. As Alan Besselink describes it in his latest blog post, "it's all in the language." Currently the APTA recognizes 48 states that have some form of direct access. Of these 48, only 17 truly have direct access to patients. Our current language is allowing patients to believe we are more autonomous than we actually are. Let patients know that we only have 17 states with true direct access so they can stand behind us in promoting more autonomy in physical therapy! "Use of a Squatting Movement as a Clinical Marker of Function After Total Knee Arthroplasty"1/10/2013  With skyrocketing health care costs, insurance agencies are constantly looking for ways to reduce reimbursement. This includes decreasing payments to organizations that have poor outcomes. As most PTs are looking to stay in business, it is important that we have valid and reliable outcome measures in order to receive appropriate reimbursement. This study looked at the effectiveness of analyzing the symmetry of a squat as a clinical marker of function after Total Knee Arthroplasty. As many functional activities involve a squat-like maneuver, the squat may prove to be a valid measure for functional ability. The authors compared body weight % on each side in standing, 30 degree squats, and 60 degree squats. For anyone who has seen a knee replacement surgery, it's easy to understand why individuals place the majority of their weight on the uninvolved limb following surgery. The compensations caused by the asymmetries place the uninvolved limb and joints around the involved knee at risk for additional injuries due to their increased load. The study found that the 60 degree squat asymmetries was correlated with individuals who had moderate difficulty with functional activities, while standing asymmetries were not. Symmetry was found to be improved upon further rehabilitation. The squat may be a useful outcome measure when treating patients following total knee replacements. Upon further research, this may be a common tool used in the clinic for assessing patient progression.
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|








 RSS Feed
RSS Feed