- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
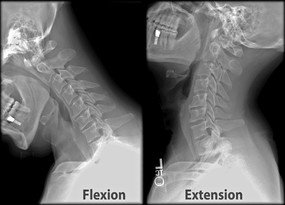
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 This is an excellent article that reviews exercise physiology, the body's response to exercise, and long-term adaptation. It does a quick summary of basic information like muscle types, metabolic response (aerobic vs anaerobic), and the activities that activate each level of metabolism. One of the initial responses to exercise is the cardiovascular response. At first, stroke volume increases alone, but at 40-60% of the VO2max, cardiac output can only increase through increased heart rate. Tissues can also improve their oxygen content by increasing oxygen extraction from the blood (arterial-venous difference). Of course, blood pressure will be found to increase as well (systolic). Additionally, hydration is a well-known component of exercise and can have significant impact on exercise performance. Dr. Noakes, on the other hand, presents the opinion of hydration levels being overly criticized as the culprit in Lore of Running. His research has found hypoglycemia and hyponatremia to be the cause of decreased athletic performance far more frequently. Regular endurance exercise has been shown to have several effects on the body. Muscles have increased mitochondria size and capillary formation. This increases blood flow to the muscle and the cells' ability to extract/utilize oxygen. Plasma volume has also been shown to increase, thus, improving the viscosity of the blood, making it easier for it to flow through the body. The increased work load results in left ventricular hypertrophy, which leads to stronger contractions. For much more, check out the article yourself! Reference: Rivera-Brown AM, Frontera WR. Principles of Exercise Physiology: Responses to Acute Exercise and Long-term Adaptations to Training (2012). PM&R: The Journal of Injury, Function, and Rehabilitation 4(11), 797-804.
3 Comments
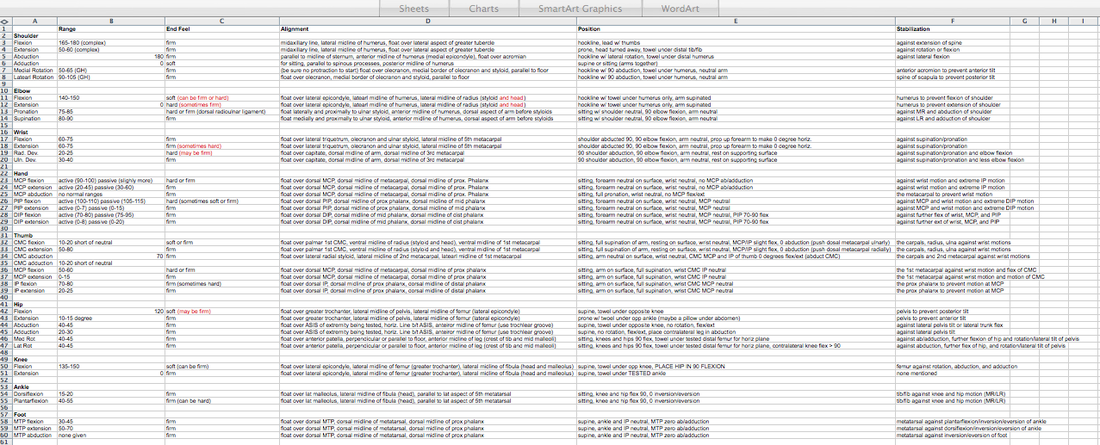
 With the success prehab has had with patients undergoing ACL reconstruction, there has been an increase in interest for prehab with total knee replacements as well. Quad strength has long been linked to functional outcomes following surgery. Given the strength deficits noted after surgery, it's possible improving strength prior to surgery may have an impact on patient outcomes. This RCT contained a placebo group and a lower body strengthening group. The placebo group performed non-specific upper body exercises, while the lower body group performed 10 minutes of warm-up and a set of exercises. The exercises included: standing calf raise, seated leg press, leg curl, and knee extension. Following prehab, increases in quadriceps strength, walking speed, and mental health were noted prior to surgery (improvements were noted in the control group as well). However, after surgery there was no difference between the control group and experimental group in these categories. Some potential limitations were a low sample size of 22 participants and a focus on open-kinetic chain exercises. It would be interesting to see the effects closed-kinetic chain exercises would have. While further research in this area is definitely still needed, it may be that prehab is not as pertinent for patients receiving a total knee replacement as compared to those preparing for ACL reconstruction. Reference: McKay C, Prapavessis H, & Doherty T. (2012). The Effect of a Prehabilitation Exercise Program on Quadriceps Strength for Patients Undergoing Total Knee Arthroplasty: A Randomized Controlled Pilot Study. PM&R: The Journal of Injury, Function and Rehabilitation, 4(9), 647-656. An essential clinical requirement is having valid and reliable Range of Motion measurements. This objective data is important not only to differentiate patients, but also for reimbursement purposes. Here is a quick review on landmarks, fulcrum placement, normal end feel, and normal Range of Motion using goniometric measurement. While not all clinics use these same anatomical landmarks, familiarizing yourself with the general concepts is important!
*Much of the information was taken from the Norkin and White Textbook. As students, we are fortunate to have access to Pubmed, Iliad, and a variety of other professional databases. The newest information in the field is spoon fed to us by our teachers. If we have questions, we can easily use the resources we are paying for through our education. As we graduate, many of these resources will be taken away. How will you continue stay on top of all the new evidence? This short youtube video gives a quick look at how to stay current with research. Additionally, Mike Reinold discusses several other strategies to stay up to date in the profession of physical therapy.
How to Read Research Articles: http://www.mikereinold.com/2011/04/how-to-read-research-articles.html 3 Steps to Integrate Evidence Based Medicine Into What You Do: It Is Not That Hard: http://www.mikereinold.com/2011/01/3-steps-to-integrate-evidence-based-medicine-into-what-you-do-it-is-not-that-hard.html
 Background Information: Biceps Tendinitis encompasses a spectrum of disorders including primary biceps tendinitis, patients without primary tendinitis, and biceps tendinosis. Primary Biceps Tendinitis (5%) is inflammation of the biceps tendon in the intertubercular groove caused by mechanical stresses and overuse. Some clinicians identify biceps tendinitis simply by individuals who exhibit anterior shoulder pain that is exacerbated by shoulder and elbow flexion (Mitra et al, 2011). Mechanical stresses can include entrapment, instability, and spontaneous rupture of the long head of the biceps tendon. These patients often suffer from secondary impingement because of scapular instability, anterior capsule laxity, or posterior joint capsule tightness. Patients suffering from secondary impingement are often your younger athletic population between 18-35 years old. Primary tendinitis is much less common than those without primary tendonitis (95%). The patients without primary tendonitis have biceps tendon pathology secondary to a rotator cuff injury or labral tear. Interestingly, biceps tendinopathy is rarely found alone. It usually occurs secondary to or a cause of another pathology (Zhang et al, 2011). 85% of patients with long head of the biceps tendon partial tears have associated rotator cuff pathologies (Gazillo 2011). Additionally the umbrella term biceps tendinitis includes biceps tendinosis, which is caused by primary impingement of the shoulder and overuse. This usually involves your older population >35 years of age. Due to their age and primary impingement, these patients are also at risk for rotator cuff pathology. CLICK HERE TO CONTINUE READING  This post come to us from in touch physical therapy blog. The author highlights 3 important components of every successful treatment session. 1) Decrease the patients pain or symptoms rating. He says a clinically meaningful change in pain is 2 points (for example changing pain from a 7/10 to a 5/10). It is also important to consider the pain during movement, and not while the patient is at rest. 2) Patient understands how to manage their symptoms One of our teachers consistently told us in class, "Your manual skills and treatment sessions are only as good as your home exercise program." She is correct. It is great if we can reduce the patient's pain, but if the patient cannot sustain that reduction in symptoms, what good have we really done? Providing good education and a strong home exercise is crucial to the patient's success. 3) Know that the patient's time and money was well spent A happy patient will hopefully be a compliant patient. It is important to remember that the patient is choosing to come see you. Many of them have high co-pays as well. As therapists we need to respect their time and money. Go above and beyond for them, and I am sure you will see positive results. Some practitioners may think they'll never encounter a patient with lymphedema based on the setting. With the fragility of the lymphatic system, a patient can develop lymphedema with surgery, treatment, trauma, and more, relatively easily. With the impedance it can place on the patient's rehabilitation, it is imperative we are aware of the best treatment methods regarding lymphedema so that we can acceleration the patient's healing process. This study reviews the evidence behind Complete Decongestive Therapy (CDT). CDT is performed daily until tissue normalization occurs. It consists of: - ~60 minutes daily of Manual Lymph Drainage (MLD) - Multi-layer, short-stretch compression bandaging with foam or layers of fabric padding of the affected limbs - Exercises to enhance lymphatic pumping - Skin care of affected areas - Compression garments for maintenance following reductions 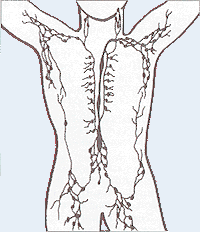 The lymphatic system is made up of a collection of lymph vessels and nodes that transport a protein rich fluid known as lymph. After undergoing trauma, the lymphatic system has the potential to become overwhelmed. Either there is too much lymph on the body or the lymphatic system can no longer support the load. This leads to the pathology known as lymphedema. The increase in fluid impairs mobility, increases limb weight, and puts the integumentary system at risk for infection. As physical therapists, we have the tools to facilitate the rehabilitation of our patients. CDT as a whole has been shown to improve quality of life and decrease limb girth. When looking at each component of CDT, however, the evidence is lacking in determining the level of effectiveness, due to poor study design and the ethical issue of withholding care. One of the most important factors is patient adherence. CDT can be extremely effective early on, but in order to maintain the results the patient must be compliant with compression garments and exercises for maintenance. While CDT has been shown to be beneficial in treating lymphedema, there is definitely room for research to improve upon the effectiveness and efficiency of our care by developing better protocols and separating the effective components of CDT from the non-effective ones. Reference:
Lasinski BB, McKillip Thrift K, Squire D, Austin MK, Smith KM, Wanchai A, Green JM, Stewart BR, Cormier JN, Armer JM. (2012). A Systematic Review of the Evidence for Complete Decongestive Therapy in the Treatment of Lymphedema from 2004 to 2011. PM&R: The Journal of Injury, Function and Rehabilitation, 4(8), 580-599.  Introduction: Low Back Pain is one of the most common musculoskeletal conditions with a lifetime prevalence between 70-85%. Ninety percent of the population will improve, but the other 10% will go on to develop chronic low back pain (cLBP). Known as a "Western Epidemic," it is estimated that the total costs of LBP each year amount to 100 billion dollars in the United States alone (Tsoa 2008). Chronic pain is defined as pain lasting longer than 6 months that is not related to a malignancy. Our current belief of pain roots from the traditional medical model that pain is a "physical response to an organic dysfunction (Wolff 1991)." Throughout the medical community there has been a push to change that traditional thinking pattern. New pain models are being produced with reliable data to support their findings. CLICK HERE TO READ MORE ABOUT THE MANAGEMENT AND TREATMENT OF CHRONIC PAIN |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|






 RSS Feed
RSS Feed