- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
Due to the complexity of the rearfoot and movement in multiple planes, understanding the motions at the talocrural and subtalar joints can be very difficult. This 3D demonstration break down each joint and discusses movement in both the open and closed chain environments. A few take home points:
-Movement at the talocrural joint is primarily in the sagittal plane, resulting in dorsiflexion and plantarflexion. -Movement at the subtalar joint consists of pronation and supination & changes whether it is occuring in open chain or closed chain. -Open-chain pronation: dorsiflexion, eversion, and abduction of the calcaneous -Open-chain supination: plantarflexion, inversion, and adduction of the calcaneous -Closed-chain pronation: calcaneal eversion with plantarflexion and adduction -Closed-chain supination: calcaneal inversion with dorsiflexion and abduction
1 Comment
 As of May 18th, we, along with the rest of the Saint Louis University PT Class of 2013, received our DPTs. Congratulations to the recent graduates from other PT schools as well! We thought we'd take some time to discuss the upcoming plans for ourselves and the site, as we do plan to continue the development of the website with some exciting upcoming features. First, an update for where each of us will be heading off to now that we've finished PT school. Jim accepted a position in Harris Health System's Orthopaedic Residency in Houston, TX that begins in late August. Chris accepted a position in Scottsdale Healthcare's Orthopaedic Residency in Scottsdale, AZ that begins at the end of July. Brian accepted a position in University of Southern California's Sports Residency in Los Angeles, CA that begins in August. With all that we expect to learn from our residencies, we hope to bring some of that to you all through one of our additions to the website. Now that we have graduated, we tossed around the idea of changing the name of the website for awhile but decided to keep the current name. A lot of our information does cater to students, but we hope that clinicians with various levels of experience find benefit in it as well. In reality, with the push for evidence-based practice and continuing education, we should be "students" of physical therapy for our entire careers. Now check out some upcoming additions to the website: Resident's Corner: As the profession continues to advance, there is an increasing push for the pursuit of residencies from various directions. With this section of the website, we will be bringing you updates on the content/curriculum of our residencies, along with some interesting techniques and information that we learn. Since the three of us will be attending different residencies, we hope to bring you three different perspectives of what residencies can offer. Hopefully, this will give you some more insight as to whether or not a residency is right for you! Interesting Cases: We have found that one of the most useful aspects of physical therapy blogs is a section like Case of the Week by The Manual Therapist, in our opinion. The step-by-step process that displays the clinical reasoning in managing each patient's case is extremely useful for developing the understanding of the transition from subjective history to objective exam to evaluation to plan of care and so on. Hopefully we can transition some of the guidance we will be getting through our mentors to you all, so that you can gain a new perspective on care. Guest Posts: We have received multiple requests from some of you on becoming involved with our website. We love to see the excitement and passion for physical therapy! Well, with our upcoming additions, you will have the chance to contribute. In general, we will be looking for a post on the Guest page every 2-4 weeks. The author would review some material they found interesting and write up a post, along with a short bio and picture. They would then submit it to us, where we will edit grammar and such (in case that's an issue!). We will not alter the content as we recognize there is benefit to discussion of controversial material. We might attach a reflection of the post in order to help facilitate some of that discussion, but the post submitted to us will remain unchanged (apart from any grammatical/spelling errors). If you would like to contribute, shoot us an email! 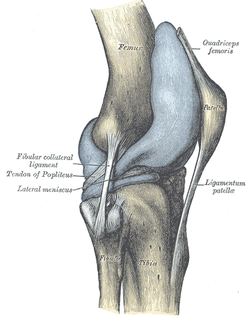 Plica! I am sure you have heard of them, but do you know the likelihood of one of these patients showing up at your clinic door? Should you consider any special treatment recommendations with this population? Keep reading to find out! Plica are inward folds of the synovial lining of the knee. Because they are embryonic deviations, plica are seen inconsistently throughout the population. Typically, they do not cause any pain and are asymptomatic, but they can become inflamed resulting in a "plica syndrome." From a clinical standpoint, it is important to note that "symptoms...are indistinguishable from other intra-articular conditions such as meniscal tears, articular cartilage injuries, or osteochondritic lesions, creating a diagnostic conundrum." There are 4 general categories of plica: suprapatellar, medial parapatellar, lateral, and infrapatellar. Lateral plica are very rarely seen and consequently little research has been conducted on them. Classification of each other type of plica becomes confusing because each one has multiple sub-groups. It is important to know that the suprapatellar plica does have attachments to the quadriceps tendon and depending on the size and shape, may create impingement between the patellar tendon and femoral trochlea in the range of 70-100 degrees of knee flexion. Similarly, the medial patellar plica also changes orientation with different positions of the knee. Its origin and attachment is controversial with several authors listing different anatomic variations. Finally, the infrapatellar plica is the most common plica in the population with 85% of patients presenting with one according to a study by Wachter in 1979. It runs superior-inferior from the intercondylar notch into the infrapatellar fat pad. The incidence of individuals with plica syndrome is under controversy, and some surgeons believe it is over-diagnosed. Clinically, 50% of patient's with plica syndrome will have a history of trauma or twisting at the knee joint. Once the initial injury is resolved, a patient maybe asymptomatic for a period of time, only to report back to the clinic weeks or months later with intense anterior knee pain. Anterior knee pain is known as the cardinal symtpom regardless of which plica is affected. Additionally, they may have complaints of a clicking or popping in the knee with flexion and describe the pain as intermittent, dull, and achy. Others report a tightness around the anterior medial knee joint which increases with deeper knee flexion angles. Because the incidence of plica syndrome is low, diligent differential diagnosis is a must, ruling out other possible causes of anterior knee pain. A clinical diagnosis alone is very difficult. Recent studies have shown the both MRI and Ultrasound have had good success in viewing plica shape and size. So what can we do for these patients? Unfortunately, "success rates of conservative management are generally low" with age being a predictive factor for your success. The younger patient is more likely to respond favorably to conservative treatment since they have not suffered the long-term effects of impinging plica and resulting structural changes within the knee joint. Therapy should consist of a period of rest from deep knee flexion activites, followed by a course of NSAIDs to help curb inflammation. Caution should be taken with intense exercise progression secondary to likelihood of aggravating the plica. Additionally, success rates of PT alone are variable and surgical intervention may be required with persistent symptoms. It should be noted that while this is a recent article, many of the references under conservative management are fairly dated. The therapy profession has since grown in its knowledge of conservative treatment for knee conditions and the importance of regional interdependence around the knee joint. In conclusion, plica syndome is not something you will see in the clinic everyday, but having this knowledge in your toolbox will make you a more well-rounded clinician. Reading this article would be very beneficial because there are great pictures discussing different variations and anatomic location. References:
Schindler O. 2013. 'The Sneaky Plica' revisited: morphology, pathophysiology, and treatment of synovial plicae of the knee. Knee Surg Sports Traumatol Arthrosc. 2013; 2013. Web. 14 May 2013.
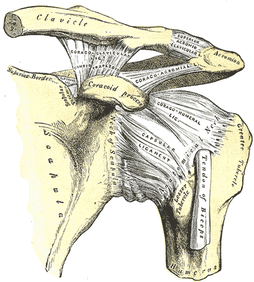
After reading these articles, it would appear that, while there are many hypotheses to the changes in shoulder impairments following thoracic spine manipulation, we still are uncertain about the mechanism. Strunce et al looked at the effect of thoracic and rib manipulations had on shoulder pain in general. The authors found both an increase in shoulder ROM and a decrease in pain. This study, like many others related to this topic, had several methodological errors. There was no blinding, randomization, or control. That doesn't mean the results of this study should be disregarded. It at least should bring the idea of regional interdependence to consideration in your differential diagnosis. Walser et al performed a systematic review for the effect of thoracic manipulations on various musculoskeletal conditions. The authors reported that significant differences were found between those who had a thoracic manipulation and those who did not, in the short-term. In the long-term, there was no difference. Scapular upward rotation is one of the usual suspects in regards to causes of subacromial impingement and rotator cuff tendinopathy. Interestingly, the literature varies on findings of decreased upward rotation to increased upward rotation in these patients (Muth et al, 2012). This study found that thoracic manipulation resulted in minimal decreases in scapular upward rotation, along with little to no change in EMG activity of the shoulder musculature. On the other hand, t-spine manipulation was found to increase shoulder elevation force production and improve both level of function and pain. While no change in shoulder elevation ROM was found, this may have been due to the fact that ROM was measured with weighted glenohumeral elevation. Strunce et al, however, did find an increase in glenohumeral motion following thoracic manipulation. Boyles et al performed an exploratory study on the effects of a single thoracic spine manipulation on subacromial impingement syndrome. While no additional treatment was performed, the authors were able to find statistically significant changes in both pain and disability scores in just 48 hours; however, these results were not found to be clinically significant, based on the established minimal change for clinical significance. The methods of this study were lacking in several areas: low participant number, no randomization, no control group, and more. The authors realized this and emphasized the fact that this study should be used as a launching point for further studies. The fact that significant changes were created after one treatment alone in just 48 hours suggests the potential for a component of care in dealing with patient suffering from subacromial impingement syndrome. Just as manual therapy + exercise was found to be greater than exercise alone for cervical pain, maybe the same applies to these conditions. Additionally, when using thoracic manipulations for cervical pain or lumbar manipulations for low back pain, there exists specific inclusion criteria in order to have the desired results. Again, maybe the same applies to thoracic manipulation for subacromial impingement (or other should pathologies) and we just need to discover the criteria. Sounds like a perfect research opportunity! Obviously, solid evidence on this topic is still lacking, but we hope that this research has at least opened your mind to the possibility of regional interdependence in your patients and maybe treating either the cervical or thoracic spine (or both) the next time you have a patient with a shoulder pathology. References:
Boyles RE, Ritland BM, Miracle BM, Barclay DM, Faul MS, Moore JH, Koppenhaver SL, Wainner RS. (2009). The short-term effects of thoracic spine thrust manipulation on patients with shoulder impingement syndrome. Man Ther. 2009 Aug;14(4):375-80. Web. 15 May 2013. Muth S, Barbe MF, Lauer R, McClure PW. (2012). The effects of thoracic spine manipulation in subjects with signs of rotator cuff tendinopathy. J Orthop Sports Phys Ther. 2012 Dec;42(12):1005-16. Web. 15 May 2013. Strunce JB, Walker MJ, Boyles RE, Young BA. (2009). The immediate effects of thoracic spine and rib manipulation on subjects with primary complaints of shoulder pain. J Man Manip Ther. 2009;17(4):230-6. Web. 15 May 2013. Walser RF, Meserve BB, Boucher TR. (2009). The effectiveness of thoracic spine manipulation for the management of musculoskeletal conditions: a systematic review and meta-analysis of randomized clinical trials. J Man Manip Ther. 2009;17(4):237-46. Web. 15 May 2013. 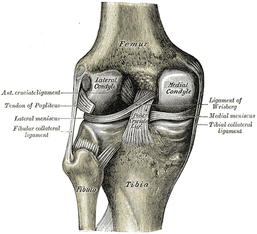 An article, discussing a new test for meniscal integrity, was recently brought to our attention. As you know, there is only one single-test for meniscus tears that has adequate diagnostic accuracy: Thessaly Test. It has a sensitivity of .89 and specificity of .92. The issue with this technique is that it can increase the tear (the test actually mimics the mechanism of injury). Another common test we see is Joint Line Tenderness, but this test has a sensitivity of .63 and specificity of .77. While this test alone is insufficient, when clustered with several other tests, the diagnostic accuracy greatly improves. The cluster includes: history of joint locking, Joint Line Tenderness, McMurray's Test, pain with flexion overpressure, and pain with extension overpressure. The article we looked at discusses using Joint Line Fullness as a clinical test. The patient is supine and the examiner palpates along the affected joint line to compare fullness to the uninjured side. If the joint line fullness causes a loss of joint compression, the test is positive. The lateral side of the knee is examined in 30-45 degrees of knee flexion to slacken the IT Band, while the medial side of the knee is examined at 70-90 degrees of knee flexion to slacken the MCL. The test had a sensitivity of .70 and specificity of .82. Again, by itself, this test's accuracy is still lacking. One might argue that it could potentially replace Joint Line Tenderness in the cluster to increase the diagnostic accuracy even more, however, we must look at the methods of the study first. The study excluded any patients with an acute injury (within 6 weeks of exam) or presence of osteophytes, joint space loss, or arthritis. Due to the fact that we often see our patients in the acute stage within 6 weeks of injury and frequently our patients have arthritis, the findings of this study become questionable. If many of our patients are bound to have the exclusion criteria, will the test still prove useful? Now, we are not suggesting that the test has no usefulness, but perhaps an additional study should be performed, where these patients are included. Reference: Couture JF, Al-Juhani W, Forsythe ME, Lenczner E, Marien R, Burman M. (2012). Joint line fullness and meniscal pathology. Sports Health. 2012 Jan;4(1):47-50. Web. 14 May 2013.  Posterior Interosseous Nerve (PIN) Syndrome is a pathology that involves pain and/or motor weakness as a result of nerve compression. In parts of the medical community, Radial Tunnel Syndrome and PIN Syndrome are one in the same, while in other parts they are different diagnoses with the same nerve involvement (Posterior Interosseous Nerve). These health care professionals identify Radial Tunnel Syndrome as pain along the radial tunnel, while PIN Syndrome is marked weakness in the muscles innervated by the Posterior Interosseous Nerve. Due to the fact that both syndromes involve compression of the same nerve, often by the same structures, we will use the terms PIN Syndrome and Radial Tunnel Syndrome synonymously in this review, especially due to the fact that the two are managed identically. CONTINUE READING... 
"What IASTM is, is not, and might be" is a recent post by Leonard van Gelder via his Dynamic Principles Blog. In this post, he discusses his usage of the EDGE Tool, why he uses it and the controversy surrounding using different instruments in his treatment sessions. First off, it is important to note that there is not a great deal of evidence surrounding IASTM. While major IASTM companies report high levels success, the amount of published articles does not directly correlate with these claims.
A few of these reported health benefits include regarding IASTM: 1. Activating the histamine response and triggering localized tissue inflammation 2. Scar Tissue (Type III Collagen) breakdown and "realigning fibers" 3. Promoting collagen synthesis by promoting fibroblast proliferation
Of those reported benefits (above), increasing fibroblast proliferation is the only property that has been consistently demonstrated through various research articles. With that said, the current studies have mainly been performed on rat MCL's with little evidence supporting long term differences in collagen synthesis whether or not IASTM was used.
In conclusion, it is important to remember that regular mobility of an affected area helps increase lubrication and maintains critical fiber distance. Whether it be from hands on techniques or the use of an instrument, it is important to keep structures mobile. As Goodman and Fuller state, "Immobilization is associated with excessive deposition of connective tissue in associated areas. This is accompanied by a loss of water and subsequent dehydration. The result is an increase in intermolecular cross-linking, which further restricts normal connective tissue flexibility and extensibility." When using Graston tools, the back edge of spoon, or the EDGE Tool, one must remember their intent behind treating with an instrument. In other words, what are you really trying to change or modify? The body of knowledge surrounding IASTM is limited, but being informed about what it is and maybe is a step in the right direction. References:
Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd Edition. St. Louis: Saunders Elsevier, 2009. Print.  Can't get enough ortho? Well, the audio recordings from the International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT) conference in Canada this year were made available (for free!) to all a couple months ago. These lectures were provided by some of the leading Ortho PTs and contain information from a wide variety of topics. Some of this material provides the latest research and topics that aren't even being presented in school yet. These could be great for listening to during long car rides during your upcoming summer break. We've only listened to a few thus far, but definitely check out the Keynote Speakers!  We all know about PubMed, but what about other electronic databases? Expand your search. Updated list of Electronic Medical Databases on Favorites page now! 1. Pubmed- U.S. National Library of Medicine's search service to Medline and Pre-Medline (database of medical and biomedical research) 2. APTA Open Door-Hooked on Evidence (database of evidence-based physical therapy practice) 3. Cochrane Database of Systematic Reviews (database of systematic reviews of RCT's; primary source for clinical effectiveness information) 4. CINAHL (database of nursing and allied health research) 5. Physiotherapy Evidence Database (PEDro) (database of physical therapy RCTs, systematic reviews, and evidence based clinical practice guidelines) 6. The Sheffield Evidence for Effectiveness and Knowledge 7. The Centre for Health Evidence 8. ERIC (database of education research) 9. Ovid (database of health and lifescience research) 10. DARE (database of abstracts of reviews of evidence from medical journals) 11. RehabDATA (database of disability and rehabilitation research) 12. Center for International Rehabilitation Research Information and Exchange (database of rehabilitation research) |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|






 RSS Feed
RSS Feed