- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
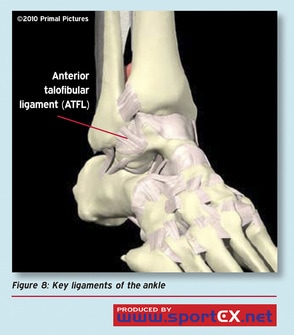 Lateral ankle sprains are among some of the most common sports medicine injuries each year. We often see this injury with basketball players as we did recently with Kawhi Leonard in the NBA playoffs. However more often than not, unless its a grade III sprain, we can get our athletes back on the court or field pretty quickly. Yet it seems like this is an injury that is often prolonged because of a few critical mistakes early on in rehabilitation. Let's talk about what you can do to quickly get your athletes back in the game. Critical Points to Consider There are a few questions you have to ask yourself when an athlete comes in to see you. First, do they have a broken ankle? Refer to the Ottawa Ankle Rules when considering if they need an X-ray. More often than not they don't if they can walk and are not tender to touch over bony areas. Second, do they have a high ankle sprain? While less common, this does occur. Be sure to take a through subjective report to understand the mechanism of injury and previous injury history. The last thing to be sure to consider is what the athlete's practice and game schedule is like. If you can get your athlete in to see you everyday for the first few days you can do a lot of good right away to get things moving in the right direction. Treatment The most important thing is to begin bringing down the swelling. Contrast baths, manual flushing, and elevation of the leg is typically very effective early on. However, one mistake I often see is therapists do not tape or compress the athlete after treatment to continue to improve the swelling. My favorite technique that I learned is a horseshoe technique that is great at improving swelling. Another technique you can use is squid taping with K-tape which is also effective. Lastly, if you don't have access to tape I would suggest having your athlete pick up a compressive sleeve. The next part of rehabilitation is the ROM and strengthening part. Range of motion should start immediately as the ankle will stiffen up from the pain and swelling. Working on ROM exercises such as ankle circles, ankle pumps, and calf stretches in the beginning are fine but as the pain tolerance improves using half kneeling ankle mobilizations against a wall or manual techniques can make big differences. As far as strengthening goes, I typically like to start manually resisted ankle strengthening quite early as I can control the range of these strengthening exercises. Typically I will start by having my athlete match my pressure so it is more of an isometric contraction but will gradually open up the range. Other exercises include towel scrunches, marbles, ankle theraband, calf raises, and lots of core and glute retraining. Many research studies have shown the importance of strengthening glutes after ankle sprains and quite frankly it just makes sense to keep the body stronger above. In addition, improving work capacity early on can make the transition back to the court/field much easier. I like to get my athletes on the bike as soon as possible. If they cannot tolerate a bike I will get them going on the upper extremity bike. Lastly, working on proprioceptive balance exercises early on is important for furthering rehab. Start with just single leg balance and progress to unstable surfaces and using arm and leg drivers to change planes of motion. Summary 1. Control swelling: - Contrast Baths, Manual flushing, Elevation of leg, compression sleeve, K-tape, Horseshoe tape technique (favorite) 2. Range of Motion: - Ankle pumps, Ankle circles, Baps board, Calf stretching (towel stretch, against wall, slantboard), Half kneeling ankle mobilizations against wall, Manual mobilizations, Bike for early movement or upper body bike to keep them in shape 3. Strengthening: - Ankle/Foot: Manually resisted 4 way ankle strengthening to ankle theraband to calf raises, towel scrunches, marbles. Glute and core retraining. 4. Balance: - Single leg balance, SL balance w/ eyes closed (stay close by), SL balance on airex, SL balance with arm and/or leg drivers to challenge further planes of motion 5. Work Capacity: - Get them on the bike or upper extremity bike (if you have access to one) ASAP to keep them moving and in shape. AlterG is great for retraining gait and running - Dr. Brian Schwabe, PT, DPT, SCS, CSCS *Check out the Insider Access video on my return to sport progression & testing for ankle sprains*
2 Comments
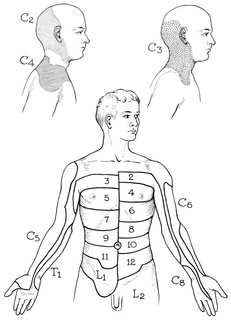
Recently, I was mentoring with Optim Manual Therapy's online case study discussion and a case was presented where there was some confusion diagnosing peripheral neuropathy versus radiculopathy. Due to the similarity in presentation sometimes, I thought it would be good to go over some of the similarities between the two and how we can differentiate as well. I am going to focus on the upper quarter region, but the same concept will apply to the lower quarter as well. Below are a couple pictures of the peripheral nerve layouts and dermatomal patterns that I will reference throughout this post. For starters, remember that both peripheral nerve lesions and radiculopathy are lower motor neuron lesions, so they can both present with corresponding weakness and hyporeflexia. Additionally, they can sometimes present with pain (or numbness/tingling) in similar regions. Think of the ulnar nerve and C8. Just because a patient has radiculopathy doesn't mean they have to have symptoms centrally/proximally as well. They both can present with symptoms along the ulnar border of the hand. Other regions have more distinct differences, for example, C7 tends to refer down the middle finger and no peripheral nerve typically presents in just that region. As you can tell, there are a lot of similarities, so how do we differentiate? There are several things to consider. An extremely useful assessment style is assessing muscle strength in muscles that have similar segmental input but different peripheral nerves. We'll go back to our C8 vs ulnar nerve example. Both are heavily innervated by the same segment and can present with symptoms in the same location. A key assessment feature is looking at the strength of Extensor Pollicis Longus. It is innervated by the radial nerve, but it's primary segmental input is C8. Should a patient have weakness here, we would be leaning more towards C8 radiculopathy. If it is strong, we would lean more towards ulnar neuropathy. The same concept can be applied to other areas. Another useful assessment is neural tensioning. Should the patient's exact symptom be reproduced with it, we likely would consider the nerve involvement; however, often radiculopathy does have a neural tension component to it, so it is not as helpful as we would like. Probably one of the best assessment techniques is using the cervical radiculopathy cluster developed by Wainner, et al: -Cervical Rotation <60 deg to involved side -(+) Median ULNT -(+) Cervical Distraction Test -(+) Spurling's Test This cluster has been shown to have high diagnostic accuracy for identifying those with cervical radiculopathy and is probably our best tool (3 positive: +LR = 6.1, 4 positive: +LR = 30.3). While one would think that pain with segmental mobility testing of the spine would be useful if pain is recreated, people can have symptoms in two locations as a result of Double Crush Syndrome or altered neurodynamics. Regardless, the most important thing is that we treat all impairments we are presented with. If the neck is stiff in someone with ulnar neuropathy, I'm still going to work on improving neck mobility. They key is that if there is research for a specific treatment for a specific diagnosis, it is important we try and identify these cases. Also, remember that there are other sources for symptoms other than peripheral nerves and radiculopathy. Patients can also present with symptoms in the exact same region due to trigger point referral patterns, local strains/sprains and more. Hopefully this will at least help with differentiating between two similar presentations. Check out the Insider Access Page for more information on this ! -Dr. Chris Fox, PT, DPT, OCS Reference: Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. "Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy." Spine (Phila Pa 1976) 2003 Jan 1.
A couple months ago, I did a mini-case study on one of my co-workers. As you may recall, he had pain with squatting in his left knee. Apparently, the knee had been bothering him for years, but with his recent running, the symptoms had increased. At the time, I had been able to reduce his symptoms with repeated motions to the lumbar spine and knee. While that worked for awhile, his pain significantly increased after doing a 5K a couple weeks ago. At that point, he came to me regarding to his knee pain not improving with the previously successful repeated motions, hoping for further advice. Having no longer responded to the quick treatments based off my initial brief evaluation, I recommended my colleague go through a more structured treatment plan. He had gone to a dry needling course with no change in knee pain. I told him to focus on glute strengthening and high repetition/low load training on the shuttle press for thousands of repetitions. While he did have success with reducing his knee swelling and general pain with the shuttle press, he continued to have pain and a contralateral shift with his squat. Last week, I had some extra time in the clinic, so I though I would mess around with some different equipment. For those of you regular followers, you may recall that about a month ago I took a visceral manipulation course. While I am still practicing the techniques each week, I thought I might try one for my colleague due to the theoretically and potentially odd effects. Being that my colleague's knee pain was on the left side, I thought I would try a stomach manipulation. I first performed a squat assessment of my colleague and he had pain and a contralateral shift. I then performed a couple stomach manipulation techniques and reassessed. During the squat immediately following the techniques, he actually fell posteriorly onto his glutes at the bottom of the squat. It sounds weird, but he actually did and he described his “orientation” being off. We then quickly reassessed and his squat was marginally improved. Having remembered that the primary effects of visceral treatment occur within 48 hours of the treatment, I again checked first thing the next day. It was completely normal and pain-free. Now I am not saying that the stomach treatment was the needed fix for sure, as it is difficult to identify correlation with such a long time between treatment and results; however, there was definitely an interesting change after so many less successful treatments. If anything, this case makes me more intrigued to practice and begin applying the visceral manipulation techniques, so that I may better learn patterns for which to apply them. -Dr. Chris Fox, PT, DPT, OCS
There are many jobs to advertise mentoring with few actually failing to live up to expectations. There are also different types of mentoring. Having completed a residency myself and being a residency faculty mentor, my experience has been one on one patient treatment and discussion. We problem solve various cases together and challenge each other on why we are doing what we are doing and possible alternatives. While that version of mentoring is ideal, it is unrealistic for employers to offer that regularly. Mentoring for other employers may mean journal clubs, chart audits, or case discussion with one of your co-workers. The concept of mentoring is understood in such a variety of ways that it is essential that prior to interviewing, you should make sure you understand what YOU want and what the employer is offering. Now if the job you take doesn't offer what you are looking for, there are other avenues as well. Discussion regularly occurs on social media groups regarding cases or general topics, although, you may have to put up with some preaching occasionally on specific treatment approaches. Additionally, there are services you can pay for where you pay for an expert's time to discuss cases or whatever you want (such as Dr. E at Modern Manual Therapy). If looking for advanced treatment or assessment ideas, you can check out our Insider Access Page. For those looking for a long-term commitment to mentoring and clinical reasoning development in addition to learning advanced techniques, you can look for a program to join, such as Optim Manual Therapy's COMT program or other system based or non-system based programs. These can help to develop your clinical reasoning overall and hands-on skill. Programs like Optim, offer weekly case discussion online as part of the program. The key for you is to know what you want in mentoring, and then to go find it! -Dr. Chris Fox, PT, DPT, OCS
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|















 RSS Feed
RSS Feed