- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 Background For the past two weeks, I have been treating a middle-aged man who sustained a compression injury to his right shoulder/ neck region (unofficially coined the schneck). When I first began treating him, his primary complaint was paresthesias in his right radial three digits with referral up the dorsum of the forearm and posterior arm. He reported a nearly constant dull or "blunted sensation" in those fingers at all times and noticed symptoms increased when looking down while at work (a combined cervical flexion and retraction movement). I was not the therapist who performed his initial evaluation, so I performed a mini-reassessment at my first visit to clear each region. Here are the pertinent positive clinical finding: CONTINUE READING
3 Comments
Good Morning!
Almost 2 years ago The Student Physical Therapist launched as a resource for students and practicing clinicians. From that time, we have over 1.2 million page views and ~2,650 followers on Facebook. We could have never expected this turn out. Next Monday, November 3rd, we will be launching a Premium version of our site. Users will have access to advanced assessment, treatment, and intervention videos performed by sports and orthopedic residency training therapists. Additionally, we will have podcasts and lectures available so you can listen or watch our content on the go. You can expect to have at least 3 new pieces of content each month! This content will advance your knowledge and clinical practice. We could not be where we are today with you! Please help us take TSPT to the next level! Sign up for our email list below & look for our premium page going live next Monday. CLICK HERE TO SIGN UP FOR OUR NEWSLETTER! Ever since my residency, I have become more aware of the advantages of using multiple resources and clinical backgrounds to treat various issues. One of the most useful resources I was exposed to was pelvic floor physical therapists. We have had guest posts and written ourselves about the various pathologies that can present as "orthopaedic" and truly be secondary to pelvic floor dysfunction. Recently, I evaluated a patient who in the initial exam reported her gynecologist instructed her to pursue pelvic floor physical therapy, yet she never did. I had already developed the opinion that this was the source of the patient's dysfunction before even treating her, but this was one of those cases where multiple issues were involved...CONTINUE READING
I was recently having a conversation with a few friends from my undergraduate schooling who all hold business degrees. I was telling them about physical therapy education- how I recently completed a residency program and how the program has helped prepare me to become an orthopedic specialist. As businessmen, the topic of money was quickly brought to the conversation. They understood I made less money last year as a resident, but assumed it would be for greater financial gain the year after. As therapists know, this is usually not the case. Being an OCS or fellow does not guarantee an increase in salary. They were dumbfounded that I would still choose to pursue specialization without the financial gain. So why do I specialize?
I choose to specialize because it will make me a more intelligent, intuitive clinician. More knowledge leads to more informed clinical decisions, clinical efficiency, and ultimately better patient outcomes. As one faculty member at the Harris Health System said, "all therapists can arrive at a diagnosis, but your residency training will help you arrive at the diagnosis much faster." The knowledge gained during my residency was unparalleled. The number of one on one mentorship hours received in one year is not attainable by many companies. I seek this knowledge because there are people living in pain that I can treat if I have the proper knowledge. I choose to specialize because I have the potential to change the profession of physical therapy. Our profession has so much potential in the present moment. We are on the horizon of taking over preventative medicine and becoming completely autonomous, direct access practitioners. It is easy to stop studying after physical therapy school and rest on a generalized education. It is easy to be uninvolved in our national organization. It is much more difficult to spend hours each week studying and collaborating with peers on ideas to better the profession. We will not get there by continuing to play the role of technician, but rather by defining ourselves as diagnosticians. I choose to specialize because of the innate satisfaction of helping another. There is an indescribable satisfaction in decreasing someone's pain and empowering them to control their pain independently. Eliminating someone's pain creates a special connection with that individual that lasts for years. Physical therapists, OTs, and SLPs are the only professions that spends 45+ minutes with their clients. This creates so much opportunity for education and change. I choose to specialize to ensure I am making those 45+ minutes as beneficial as possible. I know I would not be able to successfully treat so many people without my residency training. No, I am not going to immediately make more money, but I am going to change many peoples lives. This brings more happiness than the temporary joy of a paycheck. For those of you who cannot afford to spend one to three years doing residency, fellowship, or advanced certification training, I challenge you to think about that commitment as a long term investment. Maybe you will not make more money immediately, but you can use a specialization to market yourself for future opportunities. An advanced degree can be the difference between becoming a clinic director vs. staff therapist. It can be used as a marketing tool to draw patients to your clinic. Unfortunately at this point, physical therapy specialists are not appropriately compensated. Insurance companies value quantity over quality and therefore clinics cannot afford to pay for quality either. We can shift this paradigm by continuing to practice the highest quality care and continuing to pursue specializations. I want to conclude with a great quote from Earl Nightingale which reads, "the opposite of courage in our society is not cowardice, it is conformity." Are you conforming to being an average practitioner or are you currently pursuing something beyond the 9-5 work hours? "What greater wealth is there than to own your life and spend it on growing." Do something for yourself, for your profession, and for your patients. Why do you specialize? -Jim Heafner  Practice what you preach. As physical therapists, we like to lecture about how our patients need to be compliant with their Home Exercise Program (HEP) if they want to get better or prevent injury. Yet we often are some of the worst patients when faced with an injury. Not only can this apply to consistency with HEP, but also with assessment patterns. Have you ever stressed to a co-worker or student the need to "look at the whole chain," then as soon as a friend asks you to look at their shoulder you get fixated on that shoulder? I recently had an awakening similar to this as I had been treating many patients with repeated motions, but treating myself with core stabilization. About a year ago, a couple friends and I ran up and down the Grand Canyon. This was done with insufficient training as I was barely able to walk for a week afterwards and unable to run for 2 weeks. Once the initial delayed onset muscle soreness (DOMS) dissipated, I noticed I would consistently get a pain along my posterior thigh when running anything longer than 2 miles. Initially, I only noticed the pain with running at terminal swing on my left side, but I began to notice it with walking and any trunk twisting motions. I took a few weeks off running, thinking I just needed more rest. When I returned to running 3 weeks later, I continued to have pain with running (although with less severity) and with occasional trunk twisting motions. During one my of my residency lab practice sessions, I had my mentor evaluate me who initially diagnosed it as a HS strain based off subjective complaints since it was bothering me with terminal swing. He advised I shorten my stride length, which did help some, but the pain remained. Upon further examination, it was found that my exact pain was reproduced with slump sciatic nerve testing on the L side. With my history of a hypermobile lumbar spine, I began treating myself with core stabilization exercises (a la Shirley Sahrmann) and sciatic nerve glides. This significantly reduced my symptoms and got me approximately 90% better. However, I would still occasionally notice the pain, especially with running and twisting. Every once in awhile, I would ask a co-worker to do a Thoraco-Lumbar (T-L) Junction manipulation which would eliminate my pain, but only temporarily. I would joke with my patients that when I am consistent with my HEP of core stabilization exercises and sciatic nerve glides, I forget about my pain and stop doing the HEP, which leads to the return of my pain. This seemed like an ongoing cycle. One day, I was on a long car drive and noticed the pain returned. However, I had just then had a realization with my patients how frequently repeated lumbar extension reduces pain, given how most patients spend too much time in lumbar flexion anyway. I quickly did about 10 standing lumbar extensions, which initially recreated my pain, but was eliminated at completion of the repetitions. I experimented and performed the repeated extensions before running and noticed I had no pain. Now I use repeated extension prophylactically in order to keep the pain away, especially with higher level activities. Now, it is clear that the Sahrmann core stabilization method can be successful, as evidenced by the reduction of my symptoms. However, I found the repeated loading to get me over the hump and allow me to return to prior level of activity symptom-free. It's not that I choose one or the other. In practice, I actually utilize both theories, as once I have found the Directional Preference, I repeatedly load that movement and follow-that up with movement re-education to isolate movement in one region from another. The biggest issue of course is compliance. With both methods, the HEP should be performed consistently, whether symptomatic or asymptomatic. -Chris Below is a video interview of Dr. Peter O'Sullivan who discusses current beliefs around spinal stabilization is regards to low back pain. You will be surprised to hear what he has to say. Key points from the YouTube clip below: -There is no single factor to cure low back pain. -The current system leads us to believe that bracing the spine is good for our low back. This causes increased compression to the low back. -Movement is healthy and physical activity is good for low back pain, but there is currently not enough evidence to say that stabilization training is not better than other forms of therapy or exercise. -Positive thinking of the spine and developing healthy movement patterns is a fundamental component in the treatment of low back pain. -Trust the strength of the low back and do not pre-tense the low back prior to movement. -Our current society promotes that the spine is a vulnerable structure. We need to change this model. *Please see my thoughts below* My personal thoughts:
-As therapists we need to educate against the pathoanatomy as the cause of one's symptoms. For example, the MRI impression is often not the cause of the problem in mechanical low back pain. -We need to educate patients that the spine is a strong structure. -Certain individuals with low back pain are overworking the spine by performing too many core stability exercises and excessively pre-tensing. This is not a healthy movement pattern. -Motor control is a key factor in the treatment of low back pain. We need to change the timing of the muscles around the low back and in turn change the poor movement pattern. While over-engaging the abdominals and low back stabilizers can be detrimental, it is necessary for the TrA to contract prior to movement initiation. Focus on the timing of muscle activation and educate against excessive bracing of the 'core muscles.' -Gluteal muscle strength and the proper pattern of gluteal muscle activation is very important in the treatment of low back pain. Remember that each muscle needs to play a role (mobility or stability). If stabilizers are being used a prime movers or vice versa, problems will arise. -A patient's daily posture (sitting, standing, sleeping, dynamic) will affect the muscle length-tension surrounding the spine. Changing one's daily postures is a great place to start if you are having difficulty with your lumbar evals. -Jim After attending my first fellowship lecture, I did some reflection on exercise technique in my own workouts. We had talked about common substitution patterns such as scapular retraction for stabilization with both shoulder press and bench press exercises. I realized in my gym workouts, I was guilty of these same compensations. Since then, I have learned to be more critical of my exercises, whether it be protracting at the end of both my push-ups and bench press or add a shrug at the end of my shoulder press. I quickly noticed the exercises were much harder, requiring lower loads; however, I no longer was relying on compensatory stabilization methods. It's easy to understand why the most dedicated of body builders likely has abnormal scapular positioning and mechanics. This exactness of exercise applies to other parts of the body as well. No matter what exercise theory you subscribe to, the need for exact form cannot be over-emphasized. There are particular methods with each theory that need to be directly followed for each exercise type. For example, Sahrmann theory is built around relative hypermobility. A hypomobile region may lead to hypermobility at another region, and that hypermobility is the source of both degeneration and pain. Sahrmann treats this by focusing on re-training movement patterns to take the excessive movement out of the painful region. In lumbar movement impairment syndromes, a careful eye is needed to point out and critique the most miniscule movements in the affected region. This can be portrayed with a supine BKFO. If a patient is complaining of pain and you notice even a slight pelvic rotation with the exercise but the pain dissipates with stabilization, the reasoning is that even that small motion is the source of pain. We must learn to be both watchful and critical of these compensatory patterns. With McKenzie theory, repeated motions require end-range to succeed. I can't tell you how many times in the past I would assess repeated motions but not emphasize the end-range. I would either see no change or worsening of symptoms and quickly move to a different approach. Since gaining a better understanding from repeated motions, I have learned to critique the form with repeated motions and enforce end-range. This has lead to significantly greater success with a reduction in pain and improvement in motion. We cannot be lazy with our therapeutic exercises. People compensate for a reason, which often contributes to the dysfunction that injured them in the first place. If we do not focus on correcting these mistakes, we may indeed be reinforcing the dysfunction. It can become difficulty with certain populations to keep a keen eye watching for these compensations, but it remains imperative that we do if we intend to deliver quality care.
-Chris In the next few weeks, The Student Physical Therapist will be adding a weekly newsletter to bring even more content to our users! The newsletter will contain articles that we post during the week, pertinent information surrounding our profession, and special website offers. To subscribe, please see our previous post to add your email to our mailing list or click on the link HERE Please help us continue growing The Student Physical Therapist! 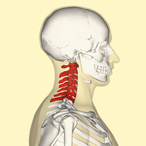 Overview As autonomous practitioners the ability to perform differential diagnosis is more important than ever. Proper differential diagnosis is the difference between treating an impairment versus treating the cause of a patient's problem. It is the difference between decreasing a patient's pain today and eliminating their movement dysfunction forever. Part of this process should include assessing the joints above or below the region of dysfunction. In this post, I want to pose this question: How do you determine if a patient is having ulnar nerve adverse neural tension or a movement dysfunction consistent with C8-T1 radiculopathy?  Common Features On initial examination, both diagnoses will have a similar presentation. In both scenarios the patient may have positive upper extremity neural tension tests, weakness and/or muscle atrophy of the hand intrinsic muscles, pain along the ulnar nerve distribution, and potentially cervical segmental nerve dysfunction. How do you differentiate? Two key features that will distinguish the difference between the peripheral nerve tension and C8-T1 radiculopathy are 1. test the strength of the extensor pollicis longus (EPL) and 2. perform specific sensation testing of the affected upper extremity. The Difference While the EPL muscle arises from the C8 nerve root (similar to ulnar nerve), it is innervated by the posterior interosseous nerve (a branch of the radial nerve). If the EPL muscle is intact, the C8 nerve root must be functioning normally. Therefore, the dysfunction is most likely a peripheral ulnar nerve entrapment. If the nerve root is the region of compromise all muscles, not only those innervated by the ulnar nerve, will be affected. The second method of assessment is checking the pattern of sensory loss. Ulnar nerve sensory loss affects the medial one and a half digits. Contrarily, the C8 nerve root can have pain from the lower scapula down the posteromedial aspect of the arm into the ring and little finger. The differences may seem subtle, but if a practitioner only suspects ulnar nerve tension, they are neglecting the cervical spine. As part of your differential diagnose make sure to assess the joint above and below the dysfunction. Now who remembers how to MMT the EPL... -Jim In the next few weeks, The Student Physical Therapist will be adding a weekly newsletter to bring even more content to our users! The newsletter will contain articles that we post during the week, pertinent information surrounding our profession, and special website offers. To subscribe, simply type in your email address below. Your email will automatically be added to our mailing list. Please help us continue growing The Student Physical Therapist! |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|







 RSS Feed
RSS Feed