- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
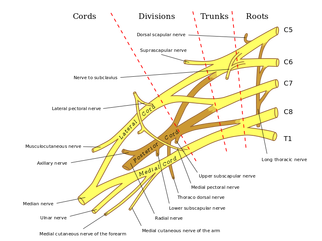
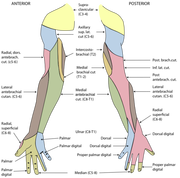
 General Overview Time and time again, the Occupational Therapists in my clinic get referrals for Carpal Tunnel Syndrome (CTS). In some of these cases, the patients also have cervical pain, shoulder pain, proximal forearm weakness, and/or palmar paresthesias. While these individuals may have compression within the carpal tunnel, many of them are suffering from nerve entrapment proximal to the carpal tunnel. Many develop adverse neural tension caused by postural dysfunctions, muscle imbalances, and systemic comorbidities which cause a breakdown of the nervous system. Am I saying CTS is over-diagnosed? That is exactly what I am saying. It has become a blanket term for pain in the wrist and hand just as lateral epicondylagia has at the elbow. Many times, the cause of someone's symptoms is not consistent with the referring diagnosis. In this mini-review, I will break down a few areas of entrapment of the median nerve and how to assess for adverse neural tension within the median nerve. Median Nerve Pathway The median nerve is formed from contributions of the spinal nerve roots C5-T1. After originating from the brachial plexus in the axilla, the medial nerve travels down the arm to the cubital fossa. Next, the nerve travels through the two heads of the pronator teres and between the flexor digitorum superficialis and flexor digitorum profundus muscles. At this point the median nerve splits into the anterior interosseous nerve (AIN) and palmar cutaneous nerve. Finally, the nerve travels through the carpal tunnel space. (Be aware there are many alternative anatomy presentations; this is simply one of the most common ones). As you can see there are many points of entrapment for the median nerve: the cervical spine, interscalene musculature, between the heads of the pronator teres, and within the carpal tunnel (among other less common ones). The patient's subjective reports and your clinical examination will point you to the correct structure and location of dysfunction. When suspecting neural tension, a clinical examination measure you should utilize is the Median Nerve ULTT. Assessing for Adverse Neural Tension & Different Sites of Entrapment We have discussed adverse neural tension several times before on The Student Physical Therapist (How to assess neural tension, Differential Dx in neural tension). At the Harris Health Orthopedic Residency, I use 3 distinguishing criteria for positive adverse neural tension testing. The symptom(s) must reproduce the patient's primary complaint, it must change by moving a component at a joint proximal or distal to the complaint, and it must be different side to side. To see the full test for adverse neural tension of the median nerve, click HERE. This test will not tell you the exact location of symptoms, but it will give you an understanding of the sensitivity of the nerve. In addition to performing neural tensioning tests, it is important to perform a thorough assessment of other potential areas of entrapment. For example, if you find muscle wasting in the FPL, pronator quadratus, and/or radial half of the FDP, the involved nerve is likely the AIN being compressed in the proximal forearm. Additionally, if the patient has comorbidities that affect the nervous system, such as a history of uncontrolled DM, this can significantly alter your patient presentation. Several clinicians I work with relate this to a form of double crush injury: the nerve is being mechanically entrapped and is also receiving compression from other intrinsic sources. Continue to use your differential diagnosis skills to determine the source of one's symptoms. It may save your patient from an unnecessary surgery. -Jim
2 Comments
 The Gait Guys recently re-posted one of their original articles, and it occurred at the beginning of the barefoot running trend. As you'll read in the article, barefoot running had advocates decades before the "vibram five-finger movement." There are many reasons for this as barefoot running has been shown to improve sensory feedback in the feet and foot intrinsic muscle control. There have been some studies that have shown decreased force translation into the lower extremity due to the development of a more efficient gait pattern. Since this article was written, quite a bit more research has been done on the topic. As you may be aware, while barefoot running may be an excellent form of running for some, it is not true for others. Some are born with anatomical foot abnormalities that make barefoot running unrealistic. With a slight change in foot structure, the majority of the force goes through one area which can lead to fractures or other overuse injuries. Even so, the article is definitely worth reading as it details how humans have used their feet over time and the response the neurological and dermatological systems have when exposed to the ground without a medium.
Next, I recommend a reassessment of the structures that were targeted during the initial evaluation. For example, if I found decreased mobility of the AA joint on the eval day, I would definitely be sure to reassess that prior to performing a manipulation - if warranted. With daily activity, joint mobility, flexibility, etc. can easily change due to something that happened between treatment sessions. And if a previously hypomobile joint is now normal, why mobilize it? Now I am not saying we should perform a complete re-examination of the objective section, but if the plan for the day involved manual therapy, I recommend assessing the targeted structures first. In cases like SIJ Dysfunction, maybe you reassess the pelvic alignment each session. How thorough you need to be is determined by dysfunction location, severity of injury, and various individual patient factors.
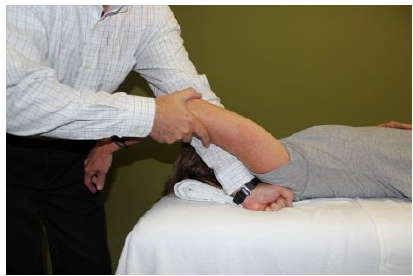
After finding the dysfunctional areas of mobility, I typically perform my manual therapy. My goal is to give the patient as much mobility in the limited structures as possible to the norm. Any limitation can lead to a compensation of hypermobility in adjacent or distant structures that may be the source of the pain. With the sedentary aspects of our lives, degeneration has become an expected normal development. While we would like to acquire true normal motion in everyone, it is not always feasible. I should note that some clinicians may prefer the patient do a warm-up prior to manual therapy or the reassessment as that may have an impact on treatment performance and clinical findings. Personally, I determine the need of a warm-up based on each individual patient. (I also should note not every patient requires manual therapy). Once I have completed my manual therapy, I go back to reassessing. Is the previous hypomobile joint now hypermobile? Is the previously painful motion or action now pain-free or less painful? We need to be certain our manual therapy had the desired outcome. As Nick Rainey states in a previous guest post, this is know as an asterisk sign (test-treat-retest). We may find that our previous assessment was inaccurate or that we need to spend a little more time with manual therapy in order to reach our goal. It is at this time that I proceed to therapeutic exercise/neuro re-ed. I truly believe it is important to complete your manual therapy first before moving this stage. With manual therapy, we often acquire new ranges of motion due to changes in joint mobility/tissue length/neural tension. While this is important, it is essential we use exercises to lock in the changes. We must retrain the body to move in those new ranges; otherwise, we are setting the patient up for re-injury. As Gray Cook has said, our bodies adapt dysfunctions often as a form of protection. If you free up the dysfunctional tissues, you are putting the patient at risk. Finally, I recommend finishing up each treatment session with another subjective portion. See how the patient immediately responds to that day's work. Some treatments have an immediate effect and again can impact our plan for the next session. As is typical, every patient is different and may require a different sequence for the treatment. This is merely an outline of how I work with my orthopaedic patients typically. There are more than a few indicators for adding, subtracting, or re-ordering the plan for that day! -Chris 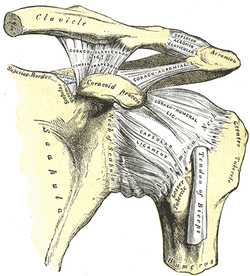 General Overview Acromioclavicular joint (ACJ) injuries are quite prevalent throughout the general population and specifically in the athletic population. In 2012 Harris et al found that ACJ disease was present in 31% of individuals who presented with shoulder pain. (Harris 2012) The ACJ is a synovial joint which connects the distal clavicle to the acromion process. The joint assists the scapulothoracic joint in full rotation to adjust for changing elevation of the humerus. Composite motion of the ACJ and sternoclavicular joint (SCJ) contributes up to 60 degrees of upward elevation, 15-30 degrees of posterior tipping, and 15-25 degrees of external rotation during arm elevation (measuring the motion at the ACJ is difficult and typically not done because the kinematics are not well defined). What we do know is that kinematics at the ACJ affect the "quality and quantity of movement at the scapulothoracic joint." (Neumann 2010) With motion occuring in 3 planes, the ACJ lacks stability and relies on 3 major ligaments for support. The acromioclavicular ligament and coracoclavicular ligaments (conoid and trapezoid) support the joint and resist horizontal stresses and limit superior translation respectively. These ligaments have fascial connections with nearby muscles, specifically the trapezius and deltoid. In a high grade AC joint separation, a clinician will often find these muscles injured as well. The resting position of the ACJ is the arm at the side and the closed packed position is full elevation. Due to the high prevalence of dysfunction, assessing the ACJ needs to be a priority during an initial evaluation with a patient who presents with shoulder pain. 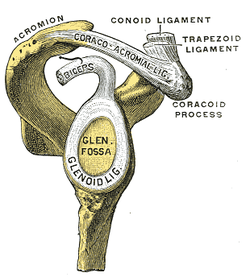 Manual Therapy Now that we know more about the ACJ, how can we treat this joint when suspecting hypomobility? Since the ACJ is a planar joint, normal concave/ convex rules of manual therapy do not apply. Therefore, we must use our clinical judgement as to when and why to perform joint mobilization or manipulation. A major factor to consider is the patient's acuity. (The novice clinician should be aware that acute ACJ separations do not require intense manual therapy because of the acuity of their symptoms and the laxity present in the region.) Generally in more acute stages, posterior to anterior ACJ mobilizations in supine with the arm resting at the side are effective (left picture below). Remember, this is the resting position of the joint as well allowing for more mobility. As the patient's ROM and strength progresses, more intense manual therapy can be performed. For example, certain patients may only have pain and limitations at end range of motion. To reach full humeral flexion and external rotation at least 30 degrees of upward rotation and 8 degrees of external rotation is needed. (Teece 2007). An example of a more advanced manual technique is a posterior to anterior mobilization at end range using the arm as a lever. In this position, the therapist's hand blocks movement of the distal clavicle so that acromion is mobilized on the stabilized clavicle. Small oscillations of the humerus are made at the end-range promoting movement at the ACJ. There are many more mobilization and manipulative techniques and positions that can be performed at the ACJ. Hopefully this post gave you an insight into a beginner and a advanced mobilization technique. -Jim References:
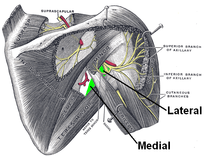
Harris, Kevin D., Gail D. Deyle, Norman W. Gill, and Robert R. Howes. "Manual Physical Therapy for Injection- Confirmed Nonacute Acromioclavicular Joint Pain." Journal of Orthopaedic & Sports Physical Therapy 42.2 (2012): 66-80. Print. Neumann, Donald A. Kinesiology of the Musculoskeletal System: Foundations for Physical Rehabilitation. St. Louis: Mosby, 2002. N. pag. Print Teece, Rachael M., Jason B. Lunden, Angela S. Lloyd, Andrew P. Kaiser, Cort J. Cieminski, and Paula M. Ludewig. "Three-Dimensional Acromioclavicular Joint Motions During Elevation of the Arm." Journal of Orthopaedic & Sports Physical Therapy 38.4 (2008): 181-90. Print. 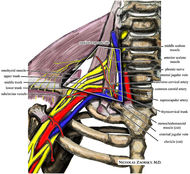 One of the greatest risks following an anterior shoulder dislocation is damage to the neurovascular structures which surround the glenohumeral joint. Due to their anatomical location, certain nerves are at a higher risk of injury than others following a dislocation. Additionally the position and displacement of the arm during the injury is another factor to consider. For example, "a fall with the arm in full abduction and internal rotation causes major tension on all nerves and cords." The Visser et al article also mentioned that concurrent fractures and the presence of a hematoma increasead the risk of nerve damage. Nerves that are at the greatest risk of injury include the axillary, suprascapular, and musculocataneous nerves. Throughout the literature, authors have found that the axillary nerve is most frequently and severely damaged (Visser). The axillary nerve originates from the upper trunk, posterior cord of the brachial plexus carrying nerve fibers from C5-C6. It courses around the surgical neck of the humerus before entering the quadrilateral space (see middle picture below to review the space boundaries). The nerve gives off muscular branches to the deltoid, teres minor, and long head of the triceps brachii. Due to the close association to the surgical neck, the axillary nerve is often compromised during an anterior-inferior shoulder dislocation. A study by Visser et al found that 42% of their 77 patients had axillary nerve insult following a low-velocity trauma anterior shoulder dislocation. Due to the high incidence of nerve related injuries, a complete neurovascular examination is warranted following a shoulder dislocation. This examination should include MMT of the shoulder and arm musculature, palpating for the brachial pulse, and examining sensation of the arm. When assessing for axillary nerve damage in particular, a clinician should look for muscle atrophy of the teres minor and deltoid muscles. One should suspect weak flexion, abduction, and external rotation of the shoulder. Observation and palpation would reveal a flat shoulder deformity due to deltoid atrophy. Additionally, they will have a lose of sensation over the upper lateral arm around the deltoid region due to denervation of the superior lateral cutaneous nerve of the arm (see right picture above). -Jim References:
Visser, C. P. J., L. N. J. E. M. Coene, R. Brand, and D. L. J. Tavy. "The Incidence of Nerve Injury in Anterior Dislocation of the Shoulder and Its Influence on Functional Recovery." The Journal of Bone and Joint Surgery 81.4 (1999): 679-85. Web. 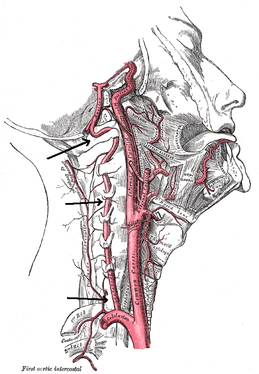 There is a common fear in treating the cervical spine (especially the upper portion) manually due to risk of injury. With the potential for damaging the vertebrobasilar artery system in the cervical spine, many people stray away from performing cervical manipulations. There have been a few situations where patients have died of ischemia following a cervical manipulation. The fatal reaction (and associated risk for lawsuit) to something that we can do as health care practitioners may discourage some from learning how to effectively apply manual therapy to the region. Is there really that much risk to injury? And what can we do to assess it? As with any fatalities in the health care system, media (and other professional disciplines) will try to make the public aware of the risk for injury following a treatment. The same case applies to cervical manipulations. Some people have a somewhat irrational fear of this technique following media coverage and word of mouth. But how much risk is there really? NSAIDS have a .0004% annual mortality rate (Vizniak 2015). There is a .00005% chance of dying from a lightning strike each year. With cervical manipulations, there is a .00002% risk of death. This means you are more likely to die from taking NSAIDS or being struck by lightning than a cervical manipulation. That being said, it is essential that proper patient selection is done before even considering this type of treatment technique. Start with patient history. Any patient with ligament laxity, rheumatoid arthritis, long-term corticosteroid use, osteoporosis/-penia, Down's Syndrome, osteoarthritis, and VBI be excluded. Naturally, we should perform our structural integrity tests and blood flow tests. We recently completed a review of the upper cervical spine that may prove beneficial reading as well. The structural integrity tests should at least include Transverse Ligament Test (and/or Sharp Purser Test), Alar Ligament Test, and a test for a Jefferson's Fracture. This last test is completed by compressing the transverse processes of the Atlas to assess for integrity. A positive test will occur with lack of stability or reproduction of neural symptoms. The artery test that is commonly performed is for Vertebrobasilar Insufficiency (VBI). While the test we show displays combined end-range motions, some say this is not necessary. With the manipulation techniques staying closer to mid-ranges, some suggest just performing complete rotation when assessing. In theory, combined rotation and extension significantly closes off the vertebral arteries greater than rotation alone. Now, the real question is: should we perform the Vertebral Artery Test? A compilation of studies revealed that there is a 0% sensitivity and .67-.90% specificity for the test (Cope et al, 1996). What this tells us is that a negative test means absolutely nothing and a positive test means a patient may have VBI. The testing we perform cannot rule out or rule in VBI. Vertebrobasilar Insufficiency is essential to consider as many of the symptoms mimic other orthopaedic cervical spine conditions: headache, neck pain, etc. (along with more traditional VBI symptoms - see link for symptoms). Even though there is poor diagnostic accuracy associated with the Vertebral Artery Test, it is recommended that the test be performed. There is a traditional thought that the vertebrobasilar artery system be tested prior to any manual therapy, no matter how poor the test is. Due to the media's perception that cervical manipulations risk VBI, any sign of "negligence" by not performing the test would likely place blame on the practitioner. As with any treatment technique, evaluate each patient individually for the potential benefit and associated risk factors prior to performing. In addition to performing the VBI test, Jim and I agree that the therapist should perform a pre-manipulative hold prior to any thrust procedure. The pre-manipulative hold allows the therapist to see how the patient will respond to the manipulative position prior to performing the thrust technique. Finally, we recommend following that process up with a "gut check" as well. Is the risk of the technique worth the reward/ benefit the patient will experience? Not everyone needs or should have a manipulation, but there are some instances where it has been shown to be highly beneficial. -Chris References:
Cote P et al. J Manipulative Physiol Ther. 1996. Vizniak, Nikita. Spinal Manual. Canada: Professional Health Systems, Inc, 2015. 156-157. Print. 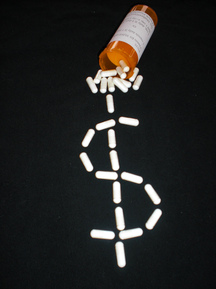 Recently, Medicare released a list of the total payments of the more than 880,000 medical providers in 2012. The total cost of these payments was ~$77 billion. While medical doctors, specifically ophthalmologists and cardiologists, were at the top of this spending list, there were a few physical therapists that had an alarmingly high number of payments. Naturally, the media latched onto this information. This past Sunday The New York Times published an article about one physical therapist in Brooklyn who billed four million dollars in Medicare in 2012. The four million dollar figure is staggering because on average physical therapists collected $49,000 in Medicare payments in that same time frame. In the article, The New York Times goes on to say "one thing is certain, physical therapy has become a Medicare gold mine." This blanket statement about the profession of physical therapy is far from true. The majority of practitioners billed within their expected range. Fortunately, the APTA was quick to react to this article. In a letter to the editor, President Paul Rockar responds to The New York Times article. Thank you to our President and the APTA for keeping everyone up to date and aware of the issues challenging our profession. -Jim References:
Creswell, Julie, and Robert Gebeloff. "One Therapist, $4 Million in 2012 Medicare Billing." The New York Times. The New York Times, 27 Apr. 2014. Web. 29 Apr. 2014. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|








 RSS Feed
RSS Feed