- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
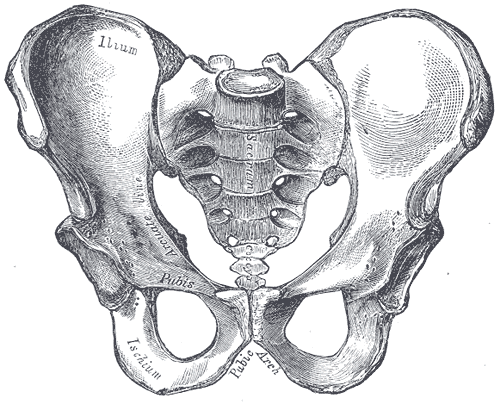
Recently, I was evaluating a patient that presented with a subjective history typical of Sacroiliac Joint Dysfunction. Additionally, she presented with an asymmetrical pelvic alignment: superior R iliac crest and PSIS along with asymmetrical pubic symphysis that was painful upon provocation. As you all know after our previous post, there is poor diagnostic accuracy when using alignment for diagnosis of SIJ Dysfunction. On the other hand, pain provocation tests are extremely effective in identifying individuals suffering from pain originating in the Sacroiliac Joint. Knowing that, I jumped to one of the SIJ clusters to rule in the pathology. I was extremely surprised to find that she was negative on all of the tests! Following a MET to restore symmetry in the pelvis, the patient's pain disappeared. Recognizing my confusion, my clinical instructor reminded me that she was currently on a steroid taper, along with a few other pain meds. In fact, the pathology was screaming at me with all of the subjective complaints, but I was too focused on the negative results of the SIJ cluster. This explained why I was unable to recreate the pain though testing. So, the lesson learned is be sure to take into account the current effects of any medications that might alter response to examination. Our tests and clusters with high evidence will not always be as effective as we think, and sometimes we have to lean more on the subjective findings.
0 Comments
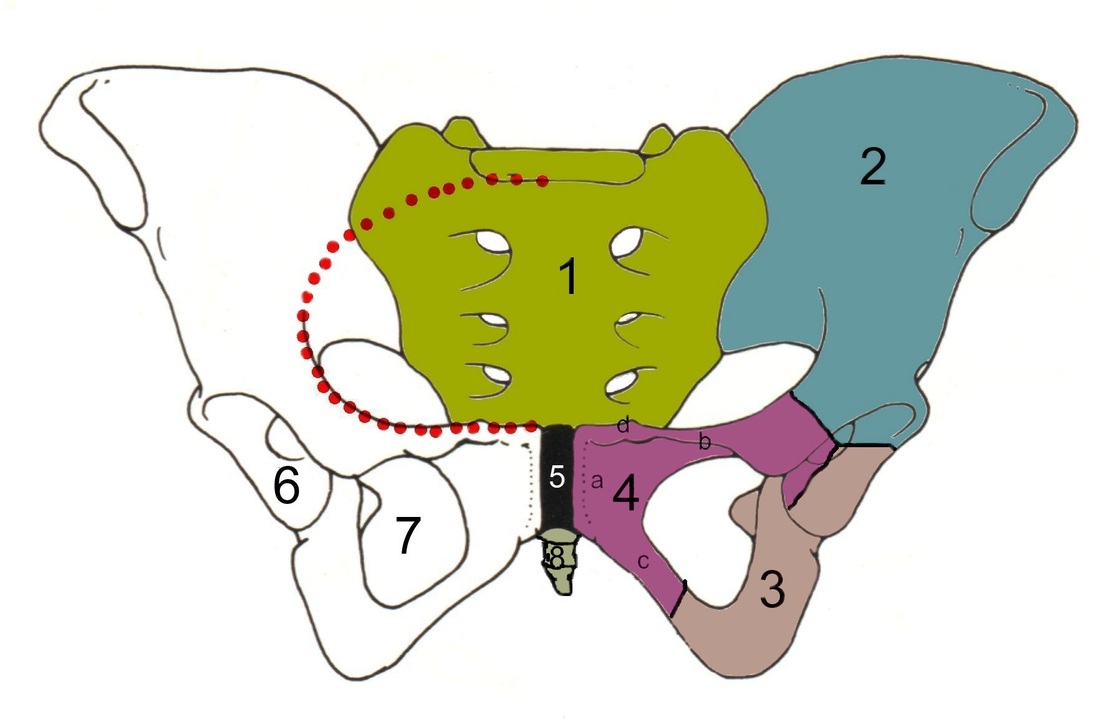
As you might be aware, there are quite a few tests out there for the Sacroiliac Joint, many of which are based on alignment. Due to the low inter-rater and intra-rater reliability of these tests based on identifying asymmetries, pain provocation tests are preferred when identifying pain arising from the Sacroiliac Joint. Unfortunately, there is not one pain provocation test that has been shown to have sufficient diagnostic accuracy by itself. This has led to the use of clusters. Two of the commonly used clusters include: a) SIJ compression, SIJ distraction, POSH Test, Sacral Clearing Test, Resisted Abduction Test; b) POSH Test, Resisted Abduction Test, FABER Test. But how do we decide which one to use? This is an example of why we need to review the literature to assess the methodological quality.
Broadhurst and Bond performed a double blind study that utilized placebo and active injections to find the effects of each test. Pain had to be decreased by 70% to be determined as originating from the SIJ. None of those injected with saline had a sufficient decrease in pain. The study found that when Resisted Abduction Test, POSH Test, and FABER Test were clustered together, there was a high likelihood of pain of SIJ origin. This test, upon initial examination, appears to have respectable methodological quality. Stuber performed a systematic review that ended up including 6 studies that looked at special tests identifying SIJ Dysfunction. Broadhurst and Bond's study was included in the review. One of the components of the study was to assess methodological quality of each one. Broadhurst and Bond's study was ranked 3rd overall, due to deficits in number of participants, drop outs, and lack of description of the examiners and tests performed. While the cluster suggested by Broadhurst and Bond may still be useful, we should be cautious given the methodological flaws. The cluster with the highest evidence according to Stuber includes: -SIJ Compression -SIJ Distraction -POSH Test -Sacral Thrust -Resisted Abduction Test When any three tests out of the five listed below are positive, there is a sensitivity of .87 and a specificity of .91  Tissue Adaptation to Physical Stress: a proposed "Physical Stress Theory" to guide Physical Therapy Practice, Education and Research, an article by Mueller and Maluf, is a must read for any physical therapy student. At SLU, I was required to read it during my first semester in the program. At the time, I did not fully understand the full extent or importance of the article. Mueller and Maluf touch on several key concepts that directly relate to our patient care. The premise behind the Physical Stress Theory (PST) is "that changes in the relative level of physical stress cause a predictable adaptive response in all biological tissues." When stresses are placed on a particular structure due to movement or posture for example, our bodies tissues must adapt to these stresses. Stress can be defined by Magnitude x Time x Direction, and it is a combination of these 3 factors that will determine our bodies response. Our goal as physical therapists is to identify patterns that lead to excessive stresses and teach the patient proper movement strategies to prevent further tissue injuries. After identifying the problem, we need to decrease pain and perceived level of disability, and then focus on increasing activity tolerance in the new pain-free movement pattern. During any initial evaluation, think about a) What factors are causing excessive stress (environmental, behavioral, etc.) and b) How can these factors be modified? A few crucial take-home points from the PST: -Movement is a significant source of physical stress. Depending on how we move can have either detrimental or beneficial effects on tissue injury. -4 Fundamental tissues that undergo stress regularly are Epithelial, Connective, Muscular, and Nervous tissue. -5 Qualities of physical stress include: Decreased stress tolerance, Maintenance (homeostasis), Increased stress tolerance (tissue overload), Injury, and Death. The article goes into great detail on each of these points. -Stress will have different effects on tissues whether it is tensile, compressive, shearing, or torsional stress. Regardless which type of stress is present, inflammation will occur immediately following tissue injury. -Postural deviations are one of the most common causes of musculoskeletal pain. -Tissues atrophy at a much faster rate than they hypertrophy. Muscle force production losses can be between 6-40% in 4-6 weeks time. -Similar to muscles, nerves can become overused due to malalignment and postural deficits. This is commonly seen in carpal tunnel sydrome and lumbar spinal stenosis. Bottom Line: Good Alignment + Good Movement = Good Musculoskeletal Health. Factors such as posture, age, movement patterns, psychological factors and environmental factors all influence this equation. It is our goal to identifty these factors to allow for normal movemen Mueller and Maluf. Tissue Adaptation to Physical Stress: a proposed "Physical Stress Theory" to guide Physical Therapy Practice, Education and Research. Physical Therapy. 2002. 84.4: 383-403. Web. 2010.
Kelly Starrett from Mobility Wod brought this issue to the light with a post last year. His findings showed that, yes, cryotherapy can be effective in reducing pain following injury, but it was inconclusive as to whether or not it improved clinical outcomes. Again, this modality can be useful in preventing the body from healing its natural way, but do we really want to do that? You might ask then about other methods of limiting pain and swelling in the area. Starrett suggests utilization of compression to limit the swelling, along with elevation at times. Another method to decrease swelling is muscle activation. Mobility (when safe) is an incredibly useful method to a) maintain strength, b) evacuate swelling through muscle pumping, and c) help to restore collagen alignment. Now we're not suggesting ice should suddenly be abandoned in physical therapy altogether, but it should be given a more serious consideration as to its appropriateness. In fact, an interesting response by Nick Heudecker was brought up to this post, questioning the analysis of the literature cited and the method of the studies as well.
Perhaps it is time to consider a shift from the traditional RICE theory to a MEAT theory, as discussed by The Sports Physiotherapist. We have actually seen the MEAT protocol in practice with impressive effectiveness for returning injured athletes to play. M=movement, E=exercise, A=analgesics (non-NSAID), T=treatment. What are your thoughts on the RICE vs MEAT debate? Should we choose one or the other? Or is there a middle-ground that is more desirable? 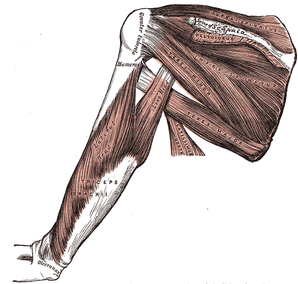 Mike Reinold is back with another post on common myths in rehabilitation. This one is in regards to rotator cuff exercises. As we frequently see patients that have some dysfunction involving these muscles, it's important to be aware of how to maximize your treatment plan to provide high quality care. The FOUR MYTHS covered include: -Rotator Cuff Exercises Are Not Functional -You Get Enough Rotator Cuff Work With Other Exercises -If You Use Heavy Weights Your Cuff Shuts Off and Larger Muscles Take Over -Use The Same Weight During All Rotator Cuff Exercises Be sure to check out Mike's post to understand his reasoning behind each myth! He also has a link on the page to his previous article on myths of scapular exercises.  While studying for the NPTE may be half the battle, figuring out how to register for exam is the other half. Below is a quick step by step breakdown on the requirements you need to complete to register for the examination. A. Log on to FSBPT website. B. On the main page, you will see shortcuts: Exam Registration. -This page gives you general information about exam registration and accessing other registration based services. C. From this page, you will see a second tab on the upper left corner also reads: Exam Registration. -The exam registration page has all the general information regarding pricing, test dates, requirements for registration. There are SIX requirements which are as follows: "1.…received and reviewed a licensure application from the licensing authority for the state in which you want to be licensed? -Remember that each jurisdiction has different requirements. 2. …determined which examination(s) you need to register for? 3.…confirmed that you meet your state's requirements to sit for an examination? 4.…notified your state if you require accommodations under the Americans with Disabilities Act? 5.…reviewed the FSBPT Candidate Handbook? Candidates who register and pay for the examination, but are not approved by their state licensing authority can withdraw their registration and receive a refund of their payment, less a processing fee." 6. After 1-5 are completed you will receive an Authorization To Test (ATT) letter from the FSBPT. -FSBPT will send you an "Authorization to Test" letter containing instructions on how to schedule an appointment with Prometric. Questions regarding registration processing may be directed to [email protected]. Schedule an appointment for the examination with Prometric. You may schedule your appointment with Prometric online at www.prometric.com/fsbpt or by calling the number given in your "Authorization to Test" letter. Sit for the examination at your chosen Prometric testing site. You must sit for the examination within your eligibility period/date as indicated on the "Authorization to Test" letter provided by FSBPT. If you do not sit for the examination, or withdraw your registration, within your eligibility, you will be removed from the eligibility list and will be required to begin the registration process again. If you are still having questions regarding the process, you may obtain assistance by contacting FSBPT Exam Services at (703) 739-9420 and select Option 1.
 Treating a shoulder patient can seem very complex and overbearing at times. This post from the Sports Physiotherapist helps breakdown different scapular dyskinesias to allow for easier diagnosis and treatment of shoulder pathologies. Reviewing each dyskinesia: Type 1: Shortening of the musculature that attaches to the coracoid process. In this dyskinesia, muscles are being shortened on the anterior side of the body (pec major and pec minor specifically). In the clinic, you will observe anterior scapular tilting and likely rounded forward shoulders. Treatment options include performing a pec minor release and pec minor stretching. Both of these techniques are demonstrated by Dr. E (the manual therapist), Mike Reinold, and Chris Johnson. Type 2: Weakness or poor activation of the Lower Trap and Serratus Anterior muscles. In the clinic, if you suspect a type 2 dyskinesia, you will likely see excessive internal rotation, "winging" of the medial border, and anterior scapular tilting. The original post has 6 great videos demonstrating how to elicit these muscles. Exercises that have shown great serratus anterior MVIC include serratus punch and push-up plus. For the lower trapezius performing prone Y's and prone shoulder external rotation is very beneficial. According to McCabe et al, Prone Shoulder External Rotation with the arm positioned at 90 degrees abduction elicited a 79% MVIC. Type 3: Excessive Superior Border Prominence. These patients often have hypertonicity of the upper trapezius muscle and likely have a poor Upper Trap: Lower Trap muscle firing ratio. From my personal experiences in the clinic, these individuals have excessively tight upper trap muscles, hypomobile first ribs, and complaints of cervical tightness as well. The Sports Physiotherapists recommends performing external rotation in neutral, upper trapezius/ levator scapulae stretching, and joint mobilization to the cervical, thoracic, and scapular regions. Additionally, Arlotta, Lovasco, and McLean found that the Modified Prone Cobra selectively recruited the lower trapezius muscle with relatively low upper trapezius muscle activation. The original article has great video demonstrations of how to perform each exercise. Check it out! References:
Arlotta M, Lovasco G, and McLean L. Selective Recruitment of the lower fibers of the Trapezius Muscle. J Electromyogr Kinesiol. 2011. 21.3: 403.410. Web. 27 Feb 2013 McCabe R, et al. Surface Electromyographic Analysis of the Lower Trapezius Muscle during exercises performed below 90 degrees of Shoulder Elevation in Healthy Subjects. N Am J Sports Phys Ther. 2007. 2.1: 34-43. Web. 27 Feb 2013. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|







 RSS Feed
RSS Feed