- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
The more patients I treat with low back pain, the more important I find the need to appropriately educate these individuals on their condition. Even patients with acute low back pain are now presenting with symptoms of chronic pain. In fact, the only thing acute about their symptoms is their date of onset. While their physical symptoms may have only began 2-3 days prior, factors such as obesity, smoking, diabetes, emotional status, unhappiness in their current social situation, and others have all been predisposing patients to low back pain. Treating these individuals is difficult. Clinicians need good knowledge of the pain matrix, neuroscience education, and chronic pain management to appropriately manage these cases. How to incorporate education into your treatment sessions? New graduates often find difficulty making education a priority during their treatment sessions. Education may not appear as a 'skilled intervention.' We need to start thinking differently about this premise. Education is perhaps the most important thing we do for people. While we may feel a bit like a psychologist, education is empowering. Additionally, education sessions often require active listening, which allows them to feel calm and relaxed (a state of mind they likely have not experienced in weeks or months). I know what you are thinking: Easy said than done in a busy clinic while managing multiple patients at a time.... One recommendation I would give you to make education seem easier: start giving education while a patient is on an aerobic machine. Educate them about why they are performing the intervention and why they are experiencing their pain. Use anatomical models, pictures on the internet, or even the video below to assist in your education. The exercise releases endorphins that allow the patient's nervous system to calm down. They can focus more on your education and less on their pain. If you feel the education is not working, step away and let the patient keep moving. With more patients presenting with chronic-type symptoms, videos like the one below can a great resource. -Jim Interested in more on Chronic Pain Management? OPTIM Physical Therapy specializes in Chronic Pain. We are now enrolling in our Phoenix and Houston cohorts.
Learn more at http://www.optimfellowship.com/
1 Comment
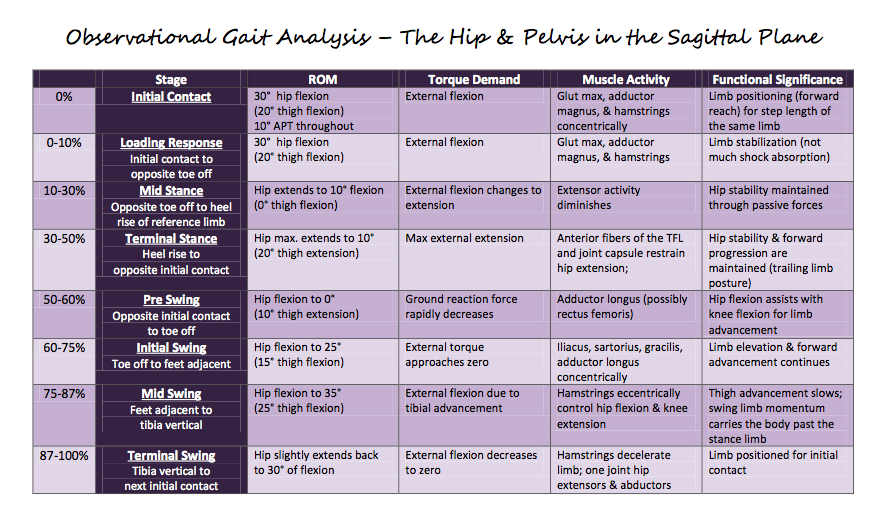
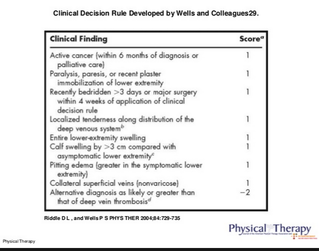
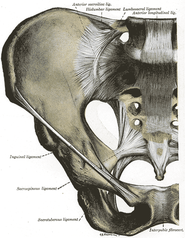
You may have seen some posts earlier on our site about OPTIM Physical Therapy. Several months ago, Chris and Jim joined OPTIM Physical Therapy to create a COMT program based out of Scottsdale, AZ. The mission of the program is to create a residency-like experience for those who are unable to make the financial and location commitment. The program consists of 6 weekend-long courses on-site, in addition to Medbridge courses and online mentoring between classes. Throughout the year, the class as a whole will improve their clinical skills and reasoning while working as a team. Additionally, with regular discussion of recent literature, you will be prepared to sit for the OCS. Below you will find a video of a google hangout where the three faculty members of the OPTIM COMT program discuss the formatting. What is not discussed in the video is how the mentoring will occur. Between each course, all participants will complete 2 mentoring forms where they summarize a patient case they are working on currently. In a google hangout, all program participants and the faculty will discuss the cases to provide guidance and alternative perspectives. For more information, check out the website at www.optimfellowship.com. One of the essential aspects of the foot that is missed during examination is the 1st toe mobility, specifically the metatarsophalangeal (MTP) joint. During healthy gait, 15 degrees of dorsiflexion (DF) is required at the talocrural joint (TC). While the joint is frequently dysfunctional, the 1st MTP joint can be limiting as well. During preswing, the 1st MTP joint can reach as much as 55 degrees of extension. Unfortunately, people are often lacking 1st MTP mobility. To assess the mobility, passively bring the joint into an extended position while stabilizing the 1st metatarsal as depicted below: Once you've identified a joint that is limited into extension, there are several manual treatments we can perform to increase the mobility. Below you will see a mobilization and manipulation technique. With the mobilization (1st row of pictures), you stabilize the metatarsal and mobilize the phalange in a dorsal direction close to the end-range of extension. With the manipulation (2nd row of pictures), you grasp the phalange close to the MTP joint while facing the patient and perform a distraction manipulation by radially deviating your wrists from an ulnarly deviated position. The manipulation brings the joint into a flexed position with distraction performed. While manual treatments are great for improving MTP mobility, it is essential an exercise be assigned as well to maintain the gains and continue to improve the extension ROM. Patients spend the majority of their time outside the clinic, so they will be responsible for locking in the changes with an exercise. Below you will find two pictures, for recommended exercises. First is a row of pictures of a 1st MTP extension stretch in closed kinetic chain. Stabilize the phalange on the ground and bring the same knee into flexion and ankle into plantarflexion, which results in extension of the MTP joint. Hold for a prolonged periods (at least 30 seconds). The second row of pictures is repeated flexion of the 1st MTP. Grasp the phalange and bring into end-range flexion repeatedly, holding for a second. Hopefully, you'll find these treatment options useful for the 1st MTP joint. Make sure to be thorough with your assessments, as a limitation here can result in changes up the change. Limited extension here results in altered mobility at the talocrural joint. If the the ankle does not dorsiflex appropriately, the knee and hip do not fully extend. This can result in decreased flexibility in hip flexors which will lead to repeated extension-rotation of the lumbar spine. This is just one example of how a limitation in one spot can affect something else much farther up the chain. It doesn't hurt to be thorough in your examination. -Chris Background Last week I was evaluating a patient 12-weeks status post rotator cuff repair. In general, the patient is progressing in her strength and function as expected. Prior to the start of the session, the patient reported she was recently having "tightness" in her calf. She denied any recent change in activity (in the past two weeks) and The reported she is an active smoker and has a history of hypertension. Below is a picture of her calf
My patient scored a 4 on the Well's DVT rule. Due to the high likelihood of a DVT I told my patient to go to the emergency room for appropriate testing. Since she was not having any immediate symptoms, I told the patient she drive herself to the hospital. Review the DVT criteria below. Blood clots are relatively uncommon in the outpatient orthopedic setting, but they do happen on occasion. Make sure you know how to treat these problems accordingly. - Jim Like this post, check out more on our Insider Access Page!
You may have seen some posts earlier on our site about OPTIM Physical Therapy. Several months ago, Chris and Jim joined OPTIM Physical Therapy to create a COMT program based out of Scottsdale, AZ. The mission of the program is to create a residency-like experience for those who are unable to make the financial and location commitment. The program consists of 6 weekend-long courses on-site, in addition to Medbridge courses and online mentoring between classes. Throughout the year, the class as a whole will improve their clinical skills and reasoning while working as a team. Additionally, with regular discussion of recent literature, you will be prepared to sit for the OCS. Below you will find a video of a google hangout where the three faculty members of the OPTIM COMT program discuss the formatting. What is not discussed in the video is how the mentoring will occur. Between each course, all participants will complete 2 mentoring forms where they summarize a patient case they are working on currently. In a google hangout, all program participants and the faculty will discuss the cases to provide guidance and alternative perspectives. For more information, check out the website at www.optimfellowship.com. When I was in school, I thought the idea of being a clinical instructor (CI) was ridiculous. Why would I want to spend time teaching a newbie? As PT's, we work long enough hours without having a student that the requirement of teaching would only lengthen our time in the clinic. The pain of doing the CPI alone wouldn't be worth it. Now that I have had a couple students, I have definitely changed my perspective. One of the obvious benefits of having a student is the development of a further grasp of the knowledge. When I have a student, I like to simulate an advanced orthopaedic seminar. Throughout the rotation we focus on the different body parts and the orthopaedic management. This requires retention of anatomical and biomechanical facts that are critical for assessment and treatment. We shouldn't teach if we don't know the material, so regular review is important. Secondly, having students challenges us as clinicians. Things we may have taken without question in previous training may not have as solid reasoning once reviewed more closely. If you're considering having a student, I recommend developing a formal plan throughout the rotation. There are many aspects of clinical development we want to cover and we are always short on time. Personally, when educating the patient on different techniques, I break up the rotation via body regions, with an emphasis on spine. Students will benefit from working with other PT's as well in order to gain different perspectives. There are many different ways to provide a solid setting for clinical growth, but remember to speak with your students about their individual goals. Again, I recommend taking on students, if given the opportunity. Not only will it help you as a clinician, but it will help many work their way into the profession. Schools are always looking for additional clinical locations. We should be proactive in guiding our potential colleagues into better awareness of their responsibilities in each setting. -Chris Have you ever wanted to enroll in a residency but not have the time or ability to financially commit? Jim Heafner, PT, DPT, OCS, SFMA and Chris Fox, PT, DPT, OCS, SFMA from The Student Physical Therapist have partnered with Dana Tew, PT, DPT, OCS, FAAOMPT from Optim Physical Therapy to create a COMT program starting in October! The mission of the program is to develop the clinical reasoning and manual skills of the participants over the course of a year through a structure similar to a residency, but without the financial sacrifice and significant time commitment, The program will help you to prepare for the OCS, improve your outcomes, and qualify for Fellowship enrollment. Check out the program for more details at www.optimfellowship.com and let us know if you have any questions! Like this post? For more advanced information, join the Insider Access Page now! Also, check out similar previous posts below:
 In last week's post, I discussed how functional impairments should lead to local bio mechanical testing. For example, femoral adduction/internal rotation noted during a squat should lead the practitioner to check gluteus medius strength. Another great example commonly seen in foot and ankle patients is out toeing during gait assessment. I often think about out toeing as the "too many toes" sign seen when examining a patient in standing from the posterior view. What does it mean when someone is out toeing during gait or static standing? First, out toeing can originate from several different areas. The patient may be resting in hip external rotation, tibial external rotation, or calcaneal eversion. Finding the cause of the dysfunction will allow you to better diagnose and treat the problem. Specifically, when assessing the foot and ankle, it is important to think about why the patient is moving in that manner & what muscles are not being engaged due to this compensation. Due to the out toeing pattern, many times these patients will be lacking ankle dorsiflexion (Remember dorsiflexion [DF] primarily occurs at the talocrural joint. When assessing DF in clinic, be sure to keep the motion in the sagittal plane. I often see people measuring a combined DF and eversion movement. This is not accurate.) In addition to lacking dorsiflexion, they will also have hypomobile talocrural joint mobility. Finally, if a patient is out toeing, they are not engaging their plantarflexors appropriately. These patients will out toe to avoid normal heel to toe progression. They will avoid toe off due to increased stress across the foot. To compensate for the lack of toe off, the body will out toe to complete the gait cycle
Like this post? Check out more in depth techniques on our Insider Access Page!  Interested in pursuing a COMT or Fellowship in Manual Therapy? Join Chris, Jim and the OPTIM Team in Phoenix or Houston! Click HERE to learn more information You may have seen some posts earlier on our site about OPTIM Physical Therapy. Several months ago, Chris and Jim joined OPTIM Physical Therapy to create a COMT program based out of Scottsdale, AZ. The mission of the program is to create a residency-like experience for those who are unable to make the financial and location commitment. The program consists of 6 weekend-long courses on-site, in addition to Medbridge courses and online mentoring between classes. Throughout the year, the class as a whole will improve their clinical skills and reasoning while working as a team. Additionally, with regularly discussion of recent literature, you will be prepared to sit for the OCS. Below you will find a video of a google hangout where the three faculty members of the OPTIM COMT program discuss the formatting. What is not discussed in the video is how the mentoring will occur. Between each course, all participants will complete 2 mentoring forms where they summarize a patient case they are working on currently. In a google hangout, all program participants and the faculty will discuss the cases to provide guidance and alternative perspectives. For more information, check out the website at www.optimfellowship.com.
 Orthopaedic medicine and therapy are traditionally rooted in the biomechanical model. If a patient has pain in their knees and they show signs of osteoarthritis, it is deemed the cause. If a patient has pain in their leg and an MRI reveals a herniated disc or bone spurs pressing on nerves, the cause is assigned again. Repetitive motion is assumed to lead to degeneration and eventually pathology. I, like many others, grasped onto these concepts and this specialty because it appears logical. With the development of pain science research, we have learned that imaging findings are not necessarily associated with pain. This means just because a patient with L sided arm pain presents with L sided stenosis in the cervical spine, we can't automatically assign a diagnosis and treat based off the pathology. Degeneration is normal aging and should not dictate treatment or expectations. This can be frustrating as many patients we see will have already seen other PT's or doctors who explained something in a biomechanical sense. It is our job to liberate our patients from their preconceived poor prognosis. That being said, we shouldn't be so quick to completely throw away various aspects of the model. As I've written about previously, I utilize the Selective Functional Movement Assessment (SFMA) in my assessments. The purpose of the examination is to identify painful and limited joints and to especially notice any asymmetries. The SFMA is built on certain landmarks for completion of a motion with less regard for quality of motion. The system is still based on a biomechanical theory, however, where the accumulation of mobility and stability from various joints results in a combined motion. The motion can often be limited by degenerative changes over time but also can be affected by neurological input/output, which contributes to the pain science theory. Because of this and the research that says we cannot be specific in our segmental joint assessment or manipulation, I took an interest to repeated motions as a treatment and assessment. They do not require much specification with diagnosis and are far easier to utilize. Based originally off McKenzie method, repeated motions has a theory built more off sensitivity of the nervous system. Injury often occurs due to a heightened nervous system and must be treated by repeatedly loading it to alter the threshold. While I have found significant success using a repeated motions approach, I haven't abandoned the manual skills from my residency and fellowship. Many of the studies that conclude inability to assess segmental restrictions include physical therapists of different skill types. The manual skills and sensitivity of a new grade compared to an experienced clinician are vastly different. The same applies to a general therapist and a FAAOMPT-credentialed therapist. I have had patients who found limited results with repeated loading and by assessing and treating any segmental restrictions the patient had greater success. Why might that be? Potentially we are focusing on treatment to the more affected region and thus improving the stimulus to alter the neural threshold. In no way am I discrediting the repeated motions approach. I think the two should regularly be utilized together and can compliment one another. Manual therapy can accelerate outcomes and repeated motions can build the patient's independence and retain the gains. It is for this reason that I encourage regular practice of one's manual skills to continue to improve sensitivity with assessment. -Chris Have you ever wanted to enroll in a residency but not have the time or ability to financially commit? Jim Heafner, PT, DPT, OCS, SFMA and Chris Fox, PT, DPT, OCS, SFMA from The Student Physical Therapist have partnered with Dana Tew, PT, DPT, OCS, FAAOMPT from Optim Physical Therapy to create a COMT program starting in October! The mission of the program is to develop the clinical reasoning and manual skills of the participants over the course of a year through a structure similar to a residency, but without the financial sacrifice and significant time commitment, The program will help you to prepare for the OCS, improve your outcomes, and qualify for Fellowship enrollment. Check out the program for more details at www.optimfellowship.com and let us know if you have any questions! One of the biggest mistakes many novice clinicians make is focusing too heavily on the site of pain. While the site of pain needs to be address for pain management purposes, many times the cause of the dysfunction is not the location of pain. For example if a patient presents with medial sided knee pain, the knee should not be the primary joint addressed. The clinician should rely more heavily on the cause of the problem which is likely at the core, hips, or ankles. In other words, instead of treating the painful region, focus on the region that is not functioning properly. How do you assess the cause of the dysfunction? First, perform specific functional movement tests including gait assessment, squat, lunge, and others. Next perform specific local biomechanical assessments of the joints surrounding the pain. Using the knee example above, during the evaluation have the patient perform the functional movements, then perform a gross AROM and strength screening of the lumbar spine, hip, and ankle. If you notice that the patient's knee moves into adduction and internal rotation during the squat & they have a positive trendelenburg while ambulating, you know you want to check the strength of the posterior gluteus medius on that side. If the patient is lacking dorsiflexion range of motion during their squat, assess dorsiflexion AROM and talocrural joint mobility. Using this same principles, if the patient exhibits normal ankle dorsiflexion during the squat, there is likely no need to check dorsiflexion range of motion. They demo'ed normal mobility functionally, it is a waste of time to assess the isolated movement. This leads to over testing and finding minute impairments unrelated to the cause of the dysfunction. With every functional deficit you see, perform specific local biomechanical tests to triangulate your findings. Please let me know if you would like more examples of functional deficits I often find that assist with my local testing. -Jim Like this post? Gain more exclusive information on our Insider Access Page!  Want TSPT information is person? Learn from Chris Fox and Jim Heafner in person starting this October! We will be starting a COMT program and are looking for serious candidates to go on this 1-year learning adventure. Take you treatment sessions to the next level! Click HERE to learn more information! |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|





















 RSS Feed
RSS Feed