- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 At least once a year I make an attempt to argue for the benefit of reaching beyond the current clinical standards. There are many who live and die by a single pillar of evidence-based practice: research. While it is an essential component to improve our practice patterns, it has limitations. Some of the crazier techniques out there are currently impossible to standardize and accurately assess. Should this alone make them useless? The other pillars include patient beliefs and clinical experience. With the power the mind plays in pain and dysfunction, it is essential we do whatever it takes to help our patient, even if the higher level research doesn't support it. Am I saying we should abandon what decades of research have taught us? Absolutely not. This evidence should absolutely guide our decision-making, just not rule it. For example, should a patient come in with patellafemoral pain syndrome, the evidence says we should incorporate quadriceps and gluteus strengthening. However, if tibial IR mobility is limited, we may possibly significantly improve the patient's function and pain through simply addressing that. There is no research to support this concept but has been seen clinically by many clinicians who implement repeated motions. Even repeated motions has some sort of foundation of research. There are other techniques and schools of practice out there that are laughed at and have shown significant clinical success, such as visceral treatment, craniosacral, dry needling and more. I'm not sure these techniques can be categorized the same way much of the EBP followers are used to, but success can be shown with implementation of asterisk signs (even if we don't know the mechanism). Without some individuals attempting to go outside the current boundaries of evidence-based practice, we would fail to learn not only what techniques or treatment styles work, but also what doesn't work. -Dr. Chris Fox, PT, DPT, OCS
0 Comments
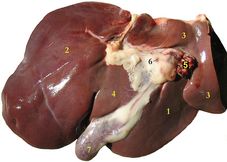 Regional interdependence is a concept regularly being taught currently, that describes how a limitation in one region can affect the movement and pain in another region. For example, limited thoracic rotation may limit overall shoulder elevation mobility and result in excessive wear/pain. With a standardized mobility examination (like the Selective Functional Movement Assessment - SFMA), we are better able to pick up some of these deficiencies. While a system like the SFMA is built more on musculoskeletal limitations, it can be useful for other systems as well. Some of you may have seen my post a couple weeks ago on my experience with visceral therapy. It is said that there is a visceral component in 80% of musculoskeletal injuries. Some of my thoracic extension mobility restrictions were secondary to visceral issues. The concept makes sense generally speaking if you think about how any tissue can theoretically resist motion. With referral patterns for pain as well, they can present with a sort of pattern. That doesn't mean visceral restrictions cannot improve without visceral treatment. However, it does mean we need to be extremely thorough with our examination. If cervical mobility is limited due to a restriction in the liver, there will unlikely be much improvement if only the neck and upper quarter observed. A system like the SFMA forces you to look at the entire body and possibly have some success through treatment. In being forced to be thorough, you will be much less likely to miss significant findings, that at first glance, appear minimal. Be sure to check out my post on my experience with visceral therapy from a couple weeks ago. I'm excited to be signed up or the level 1 course in April! Check out www.barralinstitute.com for more details on their methods of treatment/evaluation. -Dr. Chris Fox, PT, DPT, OCS
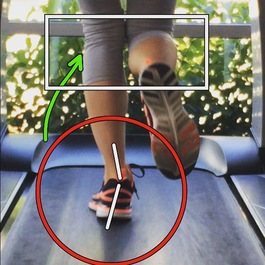
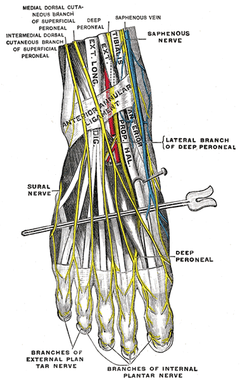
Whether a physical therapist is performing a cervical evaluation or ankle evaluation, analyzing a patient's gait pattern should be a standard aspect of every examination. The information gathered during this functional assessment will allow the clinician to quickly make educated decisions regarding the patient's overall presentation. For example, if the patient has a compensated Trendelenburg during the stance phase of gait, one can assume the strength or motor control of the Gluteus Medius is insufficient. One's ability to recognize these patterns will ultimately differentiate a novice clinician from an expert. Gait Analysis Considerations |
| If you are looking to improve upon your clinical skills, orthopaedic knowledge and clinical decision making, consider joining OPTIM's COMT program. With OPTIM, you can expect a residency-like learning experience without breaking the bank, all while learning from highly skilled physical therapists. Check out optimfellowship.com for more information! |
-Dr. Chris Fox, PT, DPT, OCS
| If you are looking to improve upon your clinical skills, orthopaedic knowledge and clinical decision making, consider joining OPTIM's COMT program. With OPTIM, you can expect a residency-like learning experience without breaking the bank, all while learning from highly skilled physical therapists. Check out optimfellowship.com for more information! |
-Chris Fox, PT, DPT, OCS
Insider Access pages
We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!
Archives
July 2019
June 2019
May 2019
March 2019
February 2019
January 2019
December 2018
November 2018
October 2018
September 2018
August 2018
July 2018
June 2018
May 2018
April 2018
March 2018
February 2018
January 2018
December 2017
November 2017
October 2017
September 2017
August 2017
July 2017
June 2017
May 2017
April 2017
March 2017
February 2017
January 2017
December 2016
November 2016
October 2016
September 2016
August 2016
July 2016
June 2016
May 2016
April 2016
March 2016
February 2016
January 2016
December 2015
November 2015
October 2015
September 2015
August 2015
July 2015
June 2015
May 2015
April 2015
March 2015
February 2015
January 2015
December 2014
November 2014
October 2014
September 2014
August 2014
July 2014
June 2014
May 2014
April 2014
March 2014
February 2014
January 2014
December 2013
November 2013
October 2013
September 2013
August 2013
July 2013
June 2013
May 2013
April 2013
March 2013
February 2013
January 2013
December 2012
November 2012
October 2012
September 2012
August 2012
Categories
All
Chest
Core Muscle
Elbow
Foot
Foot And Ankle
Hip
Knee
Manual Therapy
Modalities
Motivation
Neck
Neural Tension
Other
Research
Research Article
Shoulder
Sij
Spine
Sports
Therapeutic Exercise












 RSS Feed
RSS Feed