- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
As many of you may have heard, Optim Manual Therapy Fellowship became accredited through both AAOMPT and ABPTRFE last year. Optim originated in Houston, TX, expanded last year to Scottsdale, AZ, and is coming to Dallas, TX this year! The Houston cohort is currently full, but both the Scottsdale and Dallas cohorts are still accepting applicants. Optim Manual Therapy currently offers a 1-year COMT program in both Scottsdale, Dallas, and Houston. The program includes 6 on-site weekend long courses covering repeated motions, standardized mobility assessments, Sahrmann's Movement Impairment Syndromes (MIS), and many manual therapy assessment/treatment techniques for each region. Additionally, between classes there are different Medbridge courses assigned in addition to several online case discussion mentoring sessions regularly throughout the year. The COMT program is an excellent way to advance your clinical skills and knowledge and to prepare for the OCS. While these are excellent goals for growth as clinicians, our goal is to change your practice patterns. We don't simply want you to go home after each course and try a few new techniques. We want you to come away from each course with a different philosophy and thought process in how to address each body region and individual. Should you complete the COMT program, you can then enroll in the Fellowship part of Optim Manual Therapy. If you have interest in joining Optim, don't hesitate to contact me or any of the faculty at Optim. Next cohorts in Houston, Dallas, and Scottsdale are beginning in September! Below you will find a lecture given for the Optim COMT program on Repeated Motions for the Cervicothoracic Spine. This is just one of many theories we teach our program participants. For more information, check out Optim Manual Therapy's youtube page, Like us on Facebook at Optim Manual Therapy, or check out www.optimfellowship.com -Chris
0 Comments
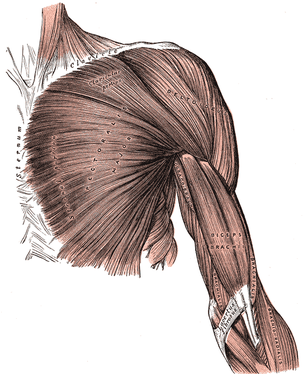
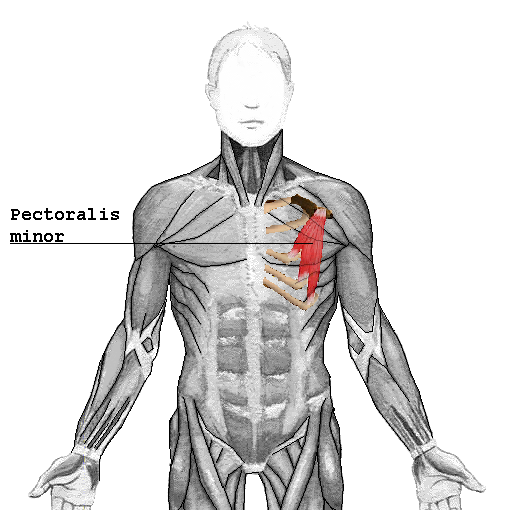
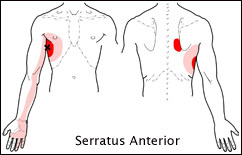
I recently had a patient with an unusual pain presentation in the right anterior chest. In general, when we see patients with chest pain, our mind jumps towards cardiac or pulmonary issues, rightfully so. However, there are musculoskeletal structures that can refer here as well. It is imperative that we are able to identify the involved structure as it may dictate how the treatment is performed. Some of the more common mechanical issues include: rib dysfunction, intercostal strain, or even thoracic disc referral. While these definitely will be seen in the clinic, they are not exclusive. The patient that inspired me to write this post described their pain as around the pectoral region but wrapping under the arm as well. This description led me to two hypotheses. Based on location alone, we should suspect some sort of pec major or minor pain. However, these muscles rarely will be the primary pain source.
 To some, cortisone injections are a miracle. The can play a crucial role with adhesive capsulitis, for example. I have had patients that tell me of past injuries that were "healed" with cortisone injections. For those of you unfamiliar with their use, the typical benefit involves reduction of inflammation and/or pain. Sometimes, patients come to you following an injection. Sometimes, they get them during the course of the treatment. And sometimes, patients get the injections as a result of failed physical therapy. That being said, there are several problems with the procedure and its impact on our job. As many of you know, cortisone injections can do an excellent job with pain reduction, but does not do much with any impairments that may have contributed to the original injuries. The issue with this is that patients come to us thinking they are "healed" but their body is still very much at risk for reinjury. When it comes to our testing, some patients are extremely sensitive to even ROM assessment. Coming out of school, I would still do my normal assessment of these patients (ROM, MMT, special tests, etc.) and they would come back in pain. With the patient thinking they have regressed as a result of the evaluation, it's possible the trust in the clinician-patient relationship will be shaken, affecting their prognosis. Some patients, especially with various biopsychosocial factors, may be affected by even the least aggressive stimulation of the affected region. So how do we assess and treat these patients? Personally, I try to keep things as minimal as possible with assessment. I'll usually do a ROM assessment while having the patient keep it in a range that is comfortable. And I'll assess strength of joints away from the affected region. That is typically it for patients after an injection. I'll begin with some lighter manual treatment and exercise to improve the mobility in a non-threatening way. I do absolutely no special tests looking for pain provocation. Once the patient starts moving better, I'll continue with further assessment and progress my treatment. Even in taking these precautions, every once and awhile I'll have a patient that is so hypersensitive that they will have an increase in pain. At that point, it is essential that we educate our patients on pain science in order to calm their nervous system. Personally, I think that cortisone injects can be a very beneficial tool in managing our patients, especially when the pain restricts them from fully participating in rehab. But I would prefer the injections be performed after a trial of therapy in order to not risk the clinician-patient relationship. -Chris
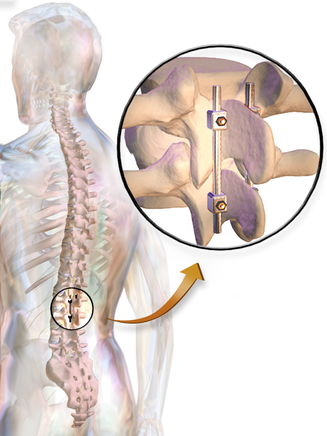
 Since starting Heafner Health (my cash based PT practice), I have started to shift my thought process on discharge planning. In my previous jobs, I would essentially discharge a patient once they could meet their pain and function related goals. In other words, I would discharge a patient when they reached their prior level of function. As an private practitioner, I have seen firsthand the downsides of this insurance based plan of care. My Soap Box: In general, people function at 60% of their full musculoskeletal capacity. Using an imaginary chart, they function slightly above the 'injury line.' Most people are never exploring their full movement potential, but instead are barely escaping pain. The reason most people operate at 60% is because they do not spend adequate time focusing on their musculoskeletal health. Our society promotes aesthetics over movement efficiency and function. The average workout is time dependent and judged by amount of weight lifted or distance travelled. Yes, injury is more common as people get older, but simply because the freedom of movement is forgotten.  Redefine Your Discharge Planning In my previous jobs, I was forced to discharge my patients back to their 60% baseline. I would eliminate their pain and restore a baseline level of function. The major joint and muscle dysfunctions were fixed, but underlying movement impairments still existed. Additionally, I would provide education and resources to hopefully prevent the injury from reoccurring. Fortunately in my current position, I can now focus on the bringing people to a higher level of movement. For me discharge planning is now about maximizing function and movement efficiency. When a patient no longer has pain, I begin treating secondary and tertiary impairments that are causing movement breakdown. During this phase, patients come to the clinic much less frequently. They are given higher level tasks that incorporate greater neural programming. The focus is now on the human movement system. Physical therapists are the movement experts. Just because someone can function in society without pain does not mean they are no longer appropriate for our services. Many people reading this are likely thinking that this will never work in their clinic. The insurance only covers 'x' amount of visits or my clinic has a policy that tries to discharge all people within 'x' amount of days. My advice: find a local strength and conditioning expert that you can trust. Once the patient has reached their discharge point, refer them to a personal trainer who understands movement and exercise progression. The physical therapy field needs to develop stronger ties with our strength and conditioning friends. We need continuity in our patient care so that we have the opportunity to bring all patients far beyond their baseline of function. -Jim Heafner  Discharge planning, manipulation, advanced clinical reasoning...OPTIM continually strives to give students the 'Monday morning applicable' experience. OPTIM COMT and Manual Therapy Fellowship is now enrolling in Scottsdale, AZ and Houston, TX. Visit optimfellowship.com for more information.  The rehab world has seen a lot of changes over the last decade. With the amount of bloggers, researchers, and continuing education out there, physical therapists have been able to learn so much more. However, at the same time we see PT's accepting ideas or things they read without questioning why or how things are supposed to work. For example, think about the phrases you use on a daily basis. Some of these are probably: activation, glutes, engage, core, stiffness, tightness, tension, and so on. I'm willing to bet that many of you haven't thought about what your really trying to say or achieve. One of the best examples I can use is "the glutes not turning on". I can say I am totally guilty of using this phrase myself. But are the glutes really not "ON"? What does that mean? While it may take more effort or work to do so, we must really question ideas or theories in our minds. Challenge some of the ideas out there and try to work through them. Really understand what you are trying to say or trying to achieve. By understanding what you are trying to achieve you will learn more about your own practice and clinical reasoning. We are all life long learners and should continue to question ourselves and our peers for the goal of understanding. Take some time this week and learn about what phrases you use and how that impacts your clinical reasoning or education to patients. - Brian One of the procedures that is heavily being researched these days is fusion of lumbar vertebrae. The theory revolves around the idea that a painful segment is dysfunctional due to "decreased disc space" or hypermobility. The procedure involves decompression and the fusion of the segments, so that pain and compression can, theoretically, no longer come from the segment. One of the obvious issues with this procedure is that it almost guarantees further degeneration and pain at the above and below segments (if you are looking at it pathoanatomically). Why? Because, in a given motion, like lumbar flexion, the force and mobility is supposed to be relatively evenly dispersed throughout the entire region. When one of the segments becomes fused, greater motion must occur at each joint, but especially at the ones directly above and below. This hypermobility leads to increased degeneration and then hypomobility and possibly pain (again assuming pathoanatomical perspective). The other major concern is that the surgery typically doesn't have that favorable results. Previous research had said that lumbar fusion had only a 25% success rate. With the risks of any invasive procedure, I know I wouldn't want to pursue it. More recently, a study revealed that fusion is no better than non-operative care for chronic low back pain. Again, with the risks, why go through with surgery? Personally, I recommend avoiding lumbar surgery in almost all cases. The risks and low success of surgery typically aren't with it, in my opinion. However, there are cases where I do recommend fusion of the spine. For example, worsening neurological signs that do not improve with conservative management, fracture, and other similar findings. There are cases where severe future injury can be avoided with surgery, like cauda equina syndrome. Lack of progress may indicate the need to switch treatment approaches, but progressively worsening symptoms may indicate the need for a surgical consultation. -Chris
As many of you may have heard, Optim Manual Therapy Fellowship became accredited through both AAOMPT and ABPTRFE last year. Optim originated in Houston, TX with the 3 cohorts thus far and expanded this past year to Scottsdale, AZ with its first cohort. Optim Manual Therapy currently offers a 1-year COMT program in both Scottsdale and Houston. The program includes 6 on-site weekend long courses covering repeated motions, standardized mobility assessments, Sahrmann's Movement Impairment Syndromes (MIS), and many manual therapy assessment/treatment techniques for each region. Additionally, between classes there are different Medbridge courses assigned in addition to several online case discussion mentoring sessions regularly throughout the year. The COMT program is an excellent way to advance your clinical skills and knowledge and to prepare for the OCS. Should you complete the COMT program, you can then enroll in the Fellowship part of Optim Manual Therapy. If you have interest in joining Optim, don't hesitate to contact me or any of the faculty at Optim. Next cohorts in Houston and Scottsdale are beginning in September! Below you will find a lecture given for the Optim COMT program on Sahrmann's Movement Impairment Syndromes (Foundation and Lumbar Spine). This is just one of many theories we teach our program participants. For more information, check out Optim Manual Therapy's youtube page, Like us on Facebook at Optim Manual Therapy, or check out www.optimfellowship.com -Chris I recently had a former patient return to me, unfortunately for the same thing I treated him for last time. I don't mind treating the same patient for multiple things, but hate treating them for previously addressed issues. It's a sign that I did not fully do my job. When I discharge my patients, they are given Home Exercise Programs (HEP's) to maintain or even improve upon where they are at in the management of their injury. So why are HEP's necessary? Unless it is a traumatic injury, people don't just randomly develop pains. There is a reason for this dysfunction. Typically, each individual is doing something repetitively or for prolonged periods that predisposes them to injury. The painter with his repetitive overhead painting, the warehouse worker with lifting, and, of course, the desk jockey with the prolonged sitting. I try to educate my patients that our bodies have a balance of motions each direction, and, when an excessive end of the spectrum is utilized, each individual has an elevated chance of pain or disability. When a patient comes to us with some sort of pain, our job is to not only address the pain, but also the dysfunction that led to the pain. After the patient has been "fixed" and discharged, management of their condition is not discontinued. They are given HEP's. Why is that? Even after the condition has been addressed and the pain is gone, the patient likely will return to whatever it is that contributed to developing pain. It is inevitable, even if we advise against it. By incorporating the Home Exercise Program, the opposite end of the health spectrum can be addressed to bring the patient back into balance. To speak more anatomically, if a patient is sitting in lumbar flexion all day, repeated lumbar extension and lumbar roll usage can dampen any concerns about prolonged sitting. Giving patients HEP's is the easy part, convincing them to perform them is the hard part. Typically, a patient will ask, at discharge, how long they will have to do their HEP. The answer: for life. Because our patients likely will continue with certain activities that predispose them to injury, they will continually have to exercise their defense against them. Now, I am not saying they will need to do hourly repeated motions forever, but they may need to do it before and after their normal exercise routine or occasionally throughout their work day. The goal is to help maintain each patient's balance to avoid dysfunction and pain. -Chris
The standard deadlift & squat promote a neutral spine position. The Jefferson Curl promotes segmental stability as the spine rounds into flexion. I recently heard about this exercise from a patient who had been attempting some gymnastic strength training exercises. During the exercise, he reported a sharp pain in his thoracic spine. Putting his injury aside, my patient asked... "is this exercise ok for my spine?" When watching his form, the patient had clear thoracic mobility deficits with a loss of lumbar flexion active range of motion. Additionally, the patient admitted to using a heavier weight than instructed. The Jefferson Curl has potential to be a great exercise for the spine if you have the underlying mobility and stability requirements to perform the movement. As a society, we have been told that lumbar flexion is bad for the low back. This statement is not true. Adequate lumbar flexion is a necessary movement for spinal health. Problems with lumbar flexion occur when someone attempts to lift a heavy weight from a flexed spine without adequate mobility and stability. Since treating this individual, I have started incorporating the Jefferson Curl into my workouts. In addition to improving my back strength, I have also noticed improvements in posterior chain flexibility. However, I do not think the Jefferson Curl is appropriate for all people initially. If someone has clear postural deficits (excessive thoracic kyphosis or lumbar lordosis), other mobility exercises likely need to be performed first. Additionally, if a patient is experiencing pain, and they have a directional preference into extension, this flexion based exercise will likely increase their symptoms. Finally if someone lacks segmental motor control of the thoracic and lumbar spines, the lumbar ligaments and discs may be at risk for injury. The Jefferson curl has it's role in addressing segmental strength of the spine, but it should not replace your squat or deadlift exercises. Patient's should be reminded that the best way to lift something from the floor is with your spine stacked in neutral alignment while engaging the hips and core. My Recommendation: 1) Start performing the Jefferson Curl exercise without any weight 2) Gradually add light weights once you can effectively perform the movement pattern 3) Address any hip or thoracic spine mobility deficits prior to performing the movement 4) Retrain and core stability deficits that may limit forward flexion -Jim Heafner PT, DPT, OCS  Enjoyed reading this post? These are the conversations that are regularly being discussed at OPTIM. The OPTIM COMT program is now enrolling our 2016-2017 cohorts for both Houston, TX & Scottsdale, AZ. Visit www.optimfellowship.com for more information |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|











 RSS Feed
RSS Feed