- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
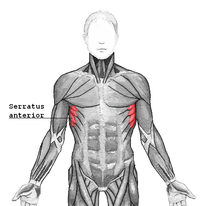
A couple weeks ago, a video was discussed on some forums about allowing lumbar flexion during deadlifts. While I believe people have always had some lumbar flexion during deadlifts and squats, traditionally, many believe a "neutral spine" is required to safely load the spine during the movement. Recently, there has been an increase in education and awareness of the flexion motion of the lumbar spine during deadlifts and squats in order to help prove the normalcy of the movement pattern. It is in conjunction with the development and understanding of pain science research that we are learning how little abnormal movement patterns may matter. Does this mean we should change our complete philosophy of movements with strength training? A couple years ago, I wrote a blog about changing scapular positioning during pressing motions. Many recommend performing a bench press with scapulae adducted in order to improve stability and open subacromial space. I proposed that we should consider altering the positions by adding protraction at the end of the bench press and shrug at the end of the military press in order to fully apply the strengthening exercise to the motions of the muscle fibers. The serratus anterior and pectoralis muscles have the function of protraction (SA also upwardly rotates the scapula). Why should we ignore that component of the muscle's function? There was some significant rebuttal from some clinicians out there on the basis of potentially damaging the rotator cuff by decreasing subacromial space. However, with the development of research showing the lack of correlation between pain and pathoanatomical findings, any "damage" that might be done with this movement pattern (if it actually occurs) can be deemed insignificant. Now, I am not suggesting that you immediately start training these alternative movement patterns with the load you typically use for your usual exercises. A new motion requires a new start. You will likely have to use significantly less weight when doing your first Jefferson curl compared to a typical deadlift. The same applies to the military press when you add a shrug at the top of the motion. Initially you will be weaker with these motions, but by training them, you will improve your strength and stability for positions that some might label as "unsafe" or "faulty." The real question that should come from these finding is should we decreasing our focus on research that emphasizes the biomechanical approach? If a RTC tear is not correlated with pain or possibly strength, why should we worry about how RTC tears develop? If a herniated disc doesn't correlate with pain or weakness, should we bother looking at studies focused on disc pressure? Personally, I believe we should still consider these concepts to some degree. Some disc herniations are significant enough to cause urinary retention. Arthritis may be significant enough to severely limit motion in a joint, decreasing the function of that joint. I am not saying that we should worry about every pathoanatomical finding either. I believe that there is possibly a middle ground to be met where pathology should still be considered, but shouldn't be the guiding force. I do not have the answer, but hopefully the research WILL continue in the mechanical area. Dr. Chris Fox, PT, DPT, OCS
1 Comment
 Yes, I said it. I train knee valgus. But hear me out before you jump to conclusions. Instead, watch a basketball game. Look at a basketball player grabbing a rebound or taking a shot. If I'm a betting man I say you will see valgus at least 10 times a game. Yes, valgus can be bad, but it doesn't mean it shouldn't be trained to control it. Let's say you get a referral for a goalie who just had ACL reconstruction. How many of you would say you wouldn't train your goalie for return to sport activities? Well, part of that return to sport is training the goalie to get back to what they do best. Sometimes that means they prefer the "butterfly" position. In case you haven't seen what this looks like, its complete valgus. Yet, this is functional for their position. So do we train valgus in the basketball athlete and the hockey goalie? In my opinion, we need to help them learn how to control those positions. If the glutes help externally rotate the femur that means it slows down internal rotation. Why not eccentrically train these muscles and also get the athlete into a "safe" position to learn how to control it toward the terminal phase of rehab? if they are going to do it anyway, then we should be helping them control the position to minimize the risk of injury. Dr. Brian Schwabe, PT, DPT, SCS, COMT, CSCS
Board Certified Sports Physical Therapist LEARN HOW TO TRAIN SPECIFIC SPORTS & POSITIONS FOR RETURN TO SPORT WITH INSIDER ACCESS The April 2018 National Physical Therapy Examination is quickly approaching. Since >50% of the examination covers musculoskeletal and neuromuscular content, it is important to spend ample time reviewing Orthopedic evaluation and examination. A portion of the Orthopedic examination is the special tests. While many of these special tests do not demonstrate good reliability individually, the diagnostic accuracy improves when clustered together. In this post, I outline the top 5 most important tests to know for the NPTE. NPTE Studying PostsImportant Special Tests for NPTE5. Lachman TestImportance of Test: The anterior cruciate ligament stabilizes against anterior translation of the tibia on the femur, due to the attachment at the anterior tibial plateau and posteriorly on the medial side of the lateral femoral condyle (Neumann 534). The force applied by the examiner stresses the ligament, and is a better test for assessing the integrity of the ACL in acute injuries compared to the Anterior Drawer Test for various reasons. The position of 20 degrees of knee flexion is a less painful position than the 90 degrees required for the Anterior Drawer Test; thus, there is a lower chance of protective spasms from the hamstrings. Also, in 20 degrees of flexion, the ACL is more maximally stressed and can be assessed more accurately, because other tissues due not limit anterior translation of the tibia ("Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis"). It should be noted that patients with a torn PCL may test positive with a Lachman test. In the starting position of the Lachman test, the tibia will rest further posterior than usual due to the absence of the PCL, leading to increased excursion during the test (Manske, 2006). This means PCL integrity should be assessed prior to looking at ACL integrity. Often with ACL injuries, other tissues and structures can be injured as well. One of the more significant findings recently has been bone contusions with ACL injuries. Look for research on the topic coming out soon! 4. Full Thickness Rotator Cuff ClusterSimilar to the hawkins-kennedy test for impingement, it is again important to cluster this test’s results with other tests and measures when assessing for rotator cuff tears. The cluster for a full thickness rotator cuff tear includes 1. the Drop-arm sign, 2. the painful arc sign, and 3. infraspinatus manual muscle test. If all three tests are positive, the +LR is 15.6. (Note is 3/3 are positive and the patient is greater than 60 years old the +LR increases to 28) If all three tests are negative the -LR is .16 If ⅔ tests are positive the +LR is 3.6 Note: Two of the three tests for this cluster are the same as the impingement syndrome cluster. The differentiating factor between impingement and rotator cuff tear is the drop arm sign for full thickness rotator cuff tears and hawkins-kennedy for subacromial impingement. 3. SLUMP TestImportance of Test: This test's results can be interpreted in multiple ways. Like other neural tension tests, the test may indicate if a patient is experiencing symptoms related to nerves adhering to various tissues while travelling throughout the body. The patient may experience stretching, pain, or other neurological sensation in the area of adhesions. Another use for the test is detecting lumbar disc herniations. With the flexed lumbar spine and hip completed simultaneously with the extended LE, the sciatic nerve and its respective nerve roots are put on tension to detect the potential of a disc herniation. The results of the test should be interpreted based on the patient's pain/symptoms for which they are seeking treatment. Looking for a more efficient way to incorporate the special tests into your examination? Check out Dr. Heafner's Guide to Efficient PT Examination. 2. Vertebral Artery TestImportance of Test: If a patient tests positive on the Vertebral Artery test, they may have Vertebrobasilar Insufficiency (VBI), but if they test negative on it, you CANNOT rule out Vertebrobasilar Insufficiency. The theory behind this test is to maximally stress the opposite vertebral artery by stretching it to decrease the space in the lumen of the artery. The position of extension with contralateral rotation has been shown to decrease the diameter of the artery, but, again, the diagnostic accuracy of the test is still poor. 1. Transverse Ligament TestImportance of Test: Whenever a you encounter a patient that has neck pain as a result of trauma or cervical instability, you should always inspect the integrity of the transverse ligament before any other exam measures. The transverse ligament is responsible for keeping the anterior facet of the atlas against the dens of the axis. It attaches on the medial side of each large, lateral process of the atlas with the anterior side of the middle part touching the odontoid process. This creates a wide space in the vertebral canal for the spinal cord to pass through, posteriorly. When the transverse ligament is damaged, the atlas can slide forward on the dens, decreasing the size of the vertebral canal for the spinal cord to go through. This can result in neurological symptoms, such as pain, weakness, a lump in the throat, etc. In this compromised position, any movements can impinge upon the spinal cord and cause potentially irreversible damage. The supine transverse ligament stress test works to reproduce symptoms in an instability patient, because the test works to decrease the space of the vertebral canal by pushing the atlas anterior on the axis. This motion is normally blocked by the transverse ligament. The Sharp-Purser test should be performed before the Transverse Ligament Stress Test, because the Sharp-Purser test works to reduce symptoms, while the Transverse Ligament Stress Test works to reproduce symptoms. (“Clinical Testing for the Craniovertebral Hypermobility Syndrome”). Any Tests We Missed?Add them to the comment section below and tell us why!
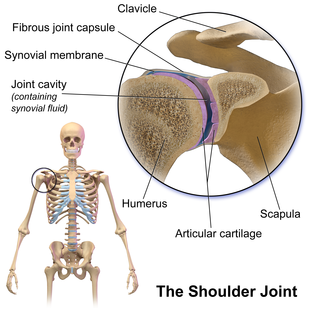
-Jim Heafner PT, DPT, OCS During one of my recent mentoring sessions for my fellowship, we saw a patient that had plateaued in progress. The patient was being seen for right upper extremity pain. The patient initially presented with pain that was associated primarily with cervical radiculopathy signs, such as bakody's sign, (+) cervical distraction test, (+) ULNT, etc. The patient initially responded great to PT as the radicular signs completely normalized. However, some right anterior shoulder pain remained that presented with signs of symptoms of shoulder dysfunction (anterior glide medial rotation syndrome, weak shoulder ER, restricted IR mobility, etc.). We gave him a few exercises to address these deficits. After a couple weeks, the pain in his shoulder had not changed and we had to decide the next course of action. The patient's initial reaction was to "give up and live with the pain." We initially talked about the possible benefit of an injection to address the pain, however, that was when our discussion switched to plan of care directly regarding PT. Upon examination, the patient still had restricted inferior GH capsular mobility, shoulder ER strength and scapular strength deficits. While the pain had not improved, the impairments had, but still had dysfunction remaining. When I first came out of school, I may have referred this patient back due to lack of progress, but with the deficits remaining, I would recommend continuing PT. His pain at this point still has impairments associated with it that can be addressed by PT, so we modified his HEP to focus on these strength and mobility deficits. Don't be so quick to give up on a patient's rehab. It is easy to become concerned when the patient isn't responding as we had hoped, but that is why it is essential to regularly evaluate the patient's progress in strength, mobility, flexibility, etc, instead of simply referring the patient back. It helps us track progress and helps the patient understand how they are responding as well. A change in the treatment plan or perspective may be necessary, or continue along the path the patient is currently on if progress is being shown. -Dr. Chris Fox, PT, DPT, OCS 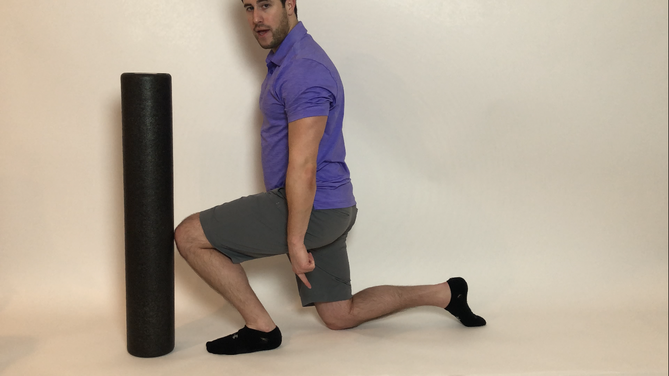 How many of you offer annual wellness screenings? How many of you would like too? As physical therapists, many times we get so stuck on offering reactive services (after injury) that we forget how valuable we really are! Think about it, we study the human body and how to move properly. Yet, as PT's we do a poor job of describing what we do and how much value we bring. This brings up the idea of offering annual wellness screens. After all, people visit the dentist, their doctor, and their accountant every year but don't get a check up on their bodies and they have to live in them everyday. We must get out of the thinking of PT only as reactive and start thinking about how much more we can help people. How many people say to you they start a fitness program only to get injured and have to stop? Or the desk jockey that says they used to be an athlete but now always feels stiff? These are perfect times to bring up how easy it would be to do an annual screen to prescribe suggested mobility or strengthening exercises to improve their condition and prevent future injuries. So what do you include in an annual wellness screen? Well, there are many things you could include but remember we are movement specialists so I would make sure you include major movements such as the overhead squat, shoulder functional ER/IR , lumbar ROM, and various breakouts based on the dysfunctions. You also want to tailor the screen to the person's individual activity. If they are a runner include some single leg squatting and hip extension screens. If they are a tennis player look closely at their overhead stability and mobility. This will ensure that the person you are screening feels the value in what you are doing for them. Remember that as PT's we offer a service and we bring value to people. Start to educate yourself on an elevator pitch and really think about some of the other services you can offer your current patients or future patients. We can do a lot more for people to help them. Dr. Brian Schwabe, PT, DPT, SCS, COMT, CSCS |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
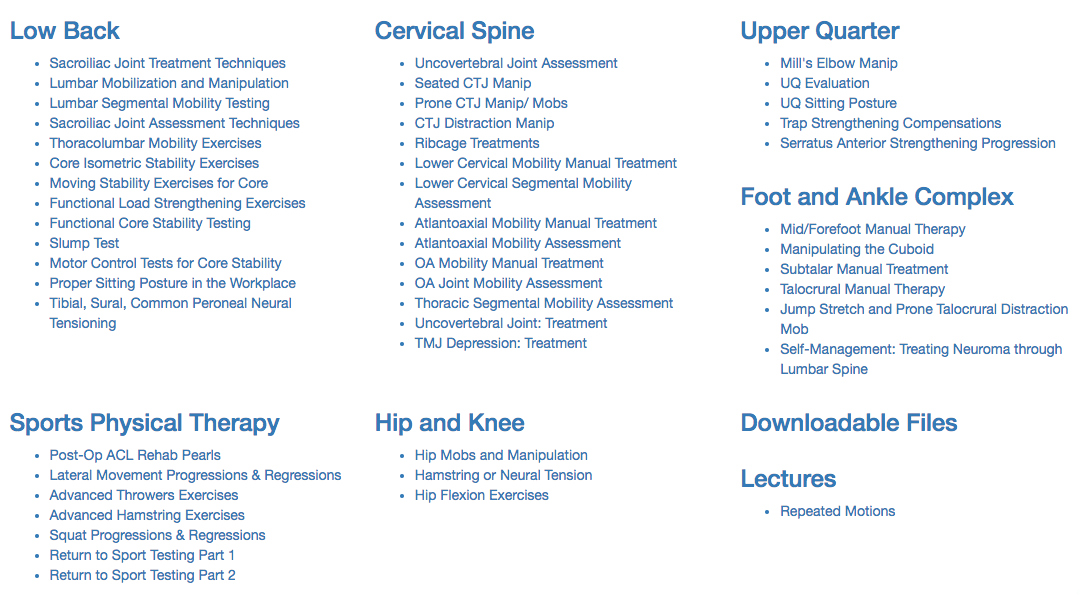
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|











 RSS Feed
RSS Feed