- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 In most physical therapy schools, including ours, McKenzie method is glossed over and, for the most part, summarized as "extension exercises." We are taught that sure it works great, but only for a small subset of populations. While some of the research may support this notion, it appears there is more to McKenzie method than the literature reveals. I recently have watched numerous video's on The Manual Therapist's channel that showed rapid changes using McKenzie method. It is more than just repeated motions. There is a necessity of reaching end-range and a clinical reasoning behind how the patient's symptoms change with the repeated or sustained motions. The Manual Therapist had a guest post recently that discussed 5 key things for understanding and implementing McKenzie. Odds are several of these topics will apply to more than McKenzie method.
0 Comments
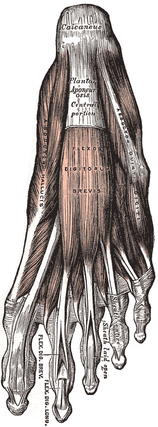 In a previous post we have written extensively about the diagnosis and management of plantar fasciopathy. Our literature review regarding conservative management showed modest improvements with the use of calcaneal taping, low level laser therapy, stretching, changing footwear, and others. In many of the controlled trial studies we read, both groups demonstrate improvement (intervention and control) and/or the study has severe limitations. It appears as if time and lifestyle modification are more important than the physical intervention performed. If the literature is consistently lacking, this tells us one of two things: our understanding of the pathology is limited OR we understand the pathology yet are still poorly managing it. In the video below, podiatrist Dr. Ray McClanahan poses some interesting arguments regarding the management of Plantar Fasciosis. For example, he discusses the negative effects of stretching the foot into dorsiflexion, which lengthens the plantar fascia. Dr. Ray states it is more important to stretch the toe extensors into flexion to take tension off the plantar fascia. Additionally he performs soft tissue work to the ADDuctor hallucis muscle in attempt to relax the lengthened and taut ABductor hallucis. His rational: when the ABductor hallucis is taut, the muscle blunts the blood supply to the plantar fascia and dorsal surface of the foot. Check out the video below and let us know what you think! -Jim My Conservative Management of a Medial Collateral Ligament Ligament Injury: Advice and More6/13/2014 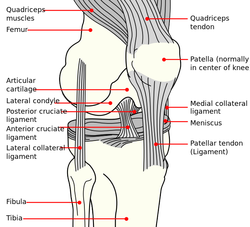 This post was inspired by a personal injury I sustained ~6 weeks ago. The nature of the injury will remain disclosed as it was a rather embarrassing traumatic event. Regardless clinical tests and measures ruled in a low/medium grade Medial Collateral Ligament (MCL) injury. With the help of some colleagues and personal knowledge, I have been self treating the injury and want to give some personal feedback regarding the process. Below are 5 key points I will touch on from a patient perspective: 1. The acute pain is real- it must treated before we can address other impairments. It is most important during the acute stage that the clinician rule-out complete ligament rupture and/or neurovascular damage prior to addressing other impairments. For 3-5 days following the injury, I would experience sharp pains with knee flexion and extension. During this time period, all provocation clinical tests were positive: McMurray, Valgus Stress Test, Apley's Compression and Distraction. Performing rotational movements such as getting out of the driver's seat of my car seemed impossible. This movement is essentially performing a self Thessaly Test. So why were all tests and measures positive? Following a knee injury, pain and swelling surround the knee make all movement painful. Swelling moves to the path of least resistance, which is located inside the joint. Additionally, it is important to look at the anatomy. The MCL has attachments into the medial meniscus, posterior-medial joint capsule, and semimembranosis tendon. The proximity of these structures can cause significant shearing to the entire area which confounds the results of the physical examination. Managing the acute pain quickly and effectively is extremely important to progressing the rehabilitation. 2. Restoring the normal joint kinematics, ROM, and muscle function is key. Following a knee injury several key impairments exist that need to be managed early in the rehabilitation process. As I stated above, addressing the acute symptoms of swelling and pain are necessary. Significant flexion and extension ROM deficits will exist and quad lag will be present. Management of these symptoms is basic, but the importance can not be understated. Since the injury, I have been much more adamant with my patients about performing heel slides, quad sets, short arc quads, and allowing me to perform tibiofemoral mobilization and manipulation. Before the injury I discredited the importance of such simple movements. One exercise I often prescribe is a heel slide + quad set combo to get a quadriceps contraction, allow for the screw home mechanism to work, and also reach full flexion in the same exercise. These exercises are relatively boring and simple, but boring does not mean unimportant and that message needs to be translated to your patients. Restoring these basic impairments- ROM, quadriceps strength, and accessory mobility- must occur before higher level strengthening and dynamic movements are brought into therapy. 3. Performing the home exercise program is not enjoyable, but it is necessary. As stated above, the early HEP is not fun and often temporarily causes increased discomfort (similar to pain) and swelling following excess movement. Anatomically speaking, discomfort is expected. Throughout knee ROM different portions of the MCL become taut. In full extension, the posterior fibers are taut and during flexion, the anterior fibers become taut. We are stressing the disrupted tissue during our HEP, but it is gentle stress which helps restore normal tensile forces to the ligament. Think about the effects of Exercise and Tissue Healing. For the first few weeks I would joke that it felt as if I had knee arthritis. The knee was very stiff in the morning with initial weight bearing and loosened within the first few steps. The pain and stiffness was related to residual swelling stuck in the knee. Personally I neglected flexion range of motion early because of the discomfort I felt during the movement. Now I am still feeling the effects of not reaching this range earlier during the rehab. The HEP needs to be performed early and often. 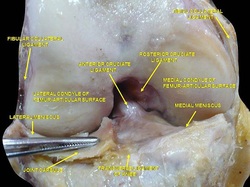 4. Do not do too much too soon. Within 3 weeks following the injury, I had "acceptable" ROM and almost full quadriceps strength and good hip strength. I had been biking for 75+ minutes at a time and was mentally exhausted from having a knee injury. I wanted to return to my prior level so I did- or at least tried to. At week 3 I returned to performing light weighted squats, running short distances, burpees, and more. This was unsuccessful. "Acceptable" ROM and almost full quad strength will not work. My body was compensating for these impairments by using the other limb greater and substituting where ever possible. I was having muscle soreness and aches in my other hip and low back. Despite these aches, I continued to load the joint abnormally, hoping the discomfort would subside. After 1-2 weeks of this exercise, my knee was just as stiff and now noticing a clicking with end-range flexion. Naturally, I was thinking an added mensical injury- pain with flexion OP, pain with extension OP, joint line tenderness, positive McMurray, and clicking and popping into flexion. Fortunately, I did not have any joint locking. I need an X-ray or MRI right? Not so fast. After resuming my prior HEP and receiving some advanced manual techniques in clinic, all of my symptoms except pain with flexion overpressure have diminished. Before jumping to any conclusions regarding imaging or surgical options, allow yourself to restore the normal joint mechanics and see what happens. I may have a partially torn meniscus, but am I a surgical candidate? What would imaging show me that would change my plan of care at this point? When working with your patients, respect the tissue healing process and use the exercise progressions and available return to sport criteria before letting them jump into full activity. 5. There will be Ups and Downs during the rehab process. I am now six weeks into my rehabilitation and things are going well. Things have not always gone well though. I became frustrated several times during the process which has slowed down my return to activity. Do not test the gods of tissue healing because they will win. The body has a natural process it must go through following injury. Final words of advice: start simple, restore normal anatomy, and use clinical judgment and any available tools for exercise progression. -Jim |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|






 RSS Feed
RSS Feed