- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
Many studies have shown the benefits of manipulation in improving muscle performance, mobility, and, of course, pain. What can be more difficult is determining the appropriate time or place for manipulation. Most manual therapy schools of thought teach their students they can manipulate specific segments and that it makes a difference. When looking at the research, support is lacking on both accounts. Studies have shown that during manipulation, cavitation can occur up to 9.5 cm above or below the "targeted" segment and that non-specific manipulation is just as effective as specific manipulation (Ross et al, 2004) (de Oliveira et al, 2013). How can it be that a non-specific manipulation is just as effective as a specific? Well the biomechanical theory of manipulation appears unlikely due to the amount of force required for collagen deformation. It seems more likely that the effects of manipulation are neurophysiological in nature. The stimulus to the nervous system may impact the tone of muscles around the various joints allowing improvements in mobility. Could that be possible? It's a theory as to why the non-specific effects can be seen, but I'm uncertain if it's possible to test. Some specific examples could be the improvements in cervical pain from thoracic manipulation (Huisman et al, 2013). While altered mechanics have been suggested, little support has been shown in research. Now, I could comment on the weaknesses of the studies shown as there are always confounding variables that cannot be controlled, but there is little benefit in focusing on that discussion, due to the difficult nature in demonstrating the mechanism of neurological changes. With all that being said, I do still believe there is benefit in trying to be specific with manipulation. I, personally and clinically, have experienced many scenarios where a general manipulation helped, but was not as helpful as targeting a specific area. There may just be a stiff area of the spine that needs the proper stimulus of increased mobility. Secondly, I believe we become much more effective with our manipulations if we try to increase our specificity. I have sat in on classes where the instructors emphasized the lack of importance in trying to be specific. The instructions were basically to wind up the patient using long levers and thrust. It is far more difficult to perform a manipulation that way, in my opinion. If you try and "target" a segment and lock them out above and below, sensing for movement at the vertebra, you typically allow the patient to relax more, which permits a more effective thrust. Again I'm not saying that we can actually manipulate that one segment, but I think we can narrow our range of force and provide more effective manipulations by allowing the patient to relax properly. -Chris References: Huisman PA1, Speksnijder CM, de Wijer A. (2013). The effect of thoracic spine manipulation on pain and disability in patients with non-specific neck pain: a systematic review. Disabil Rehabil. 2013 Sep;35(20):1677-85. de Oliveira RF1, Liebano RE, Costa Lda C, Rissato LL, Costa LO. (2013). Immediate effects of region-specific and non-region-specific spinal manipulative therapy in patients with chronic low back pain: a randomized controlled trial. Phys Ther. 2013 Jun;93(6):748-56. Ross JK1, Bereznick DE, McGill SM. (2004). Determining cavitation location during lumbar and thoracic spinal manipulation: is spinal manipulation accurate and specific? Spine (Phila Pa 1976). 2004 Jul 1;29(13):1452-7.
Like this post? Then check out the Insider Access Page for advanced content! And check out similar posts below!
0 Comments
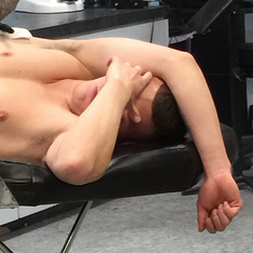
 I have been treating the individual in the picture to the left for 4 visits following a forward bending injury. After 4 visits he has reported 90% improvements in pain and function. His treatment sessions have focused on neutral core posture with hip strengthening & retraining his squat, deadlift, and reaching patterns. On the date of this photo, he is no longer having low back pain, but complains of lower thoracic spine pain. What do we see from the picture? First, he is lacking forward flexion active range of motion. He should be able to touch his hands to the floor when bending forward. Second, he does not have a uniform spinal curve. Almost all of his movement is coming from his thoracic spine. The large hump in the middle back is a good indication that the lumbar spine is not flexing! In addition the location of his pain is at the transitional zone from the thoracic spine to the lumbar spine (TL Junction). Finally, this individual does not translate his hips posteriorly at the proper time. In the photo, some posterior hip translation is noted; however, this movement only occurs after the thoracic spine has ran out of room to move. Normally, an individual should lead the movement from their hips.
Conclusion How our patient's move gives us so much information about their pain. At the end of the treatment, he could bend forward about 50% further with an improved uniform spinal curve. A key point to note: I did not directly work on his lumbar AROM, but by providing stability and motor control to the thoracic spine, his lumbar range of motion improved. This treatment session is a great example of the necessity to treat the area of dysfunction not pain! Jim  Final Days to Apply for OPTIM COMT Program! Join the program to improve your movement analysis and manual therapy skills.  The standard doctorate of physical therapy program is 3 years with a majority of classes oriented toward Orthopedic and Neuromuscular (NM) pathologies. These courses focus in depth on pathophysiology of NM conditions, diagnosis, and treatment. Even the courses focusing on cardiovascular rehabilitation or pediatric care have strong connections back to the neuromuscular system. All of these classes have the common goal of making us experts in the human movement system. 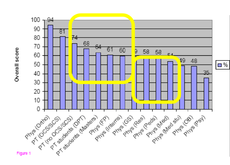 How does Our Education compare to Our Medical Counterparts? Largely, education in neuro-musculoskeletal medicine has shown to be inadequate in medical school curricula. Almost half of the American medical schools do not require any formal clinical or basic NM-skeletal courses prior to graduation. Additionally, <3% of all curricular hours in the typical Candadian medical school are devoted to NM-skeletal education. Think about these statistics for a minute! Our referral sources have very little, if not zero, education in our field of specialization. To make the PT case stronger, Childs et al published a study in 2005 that suggests Physical Therapists do not suffer from a lack of knowledge or diagnostic skill. The study found that Orthopedic Physicians (surgeons) had the highest level of competency regarding neuromuscular conditions. Physical Therapists with an OCS or SCS were the second most knowledgeable, following by Physical Therapists without a specialization. In fact, DPT students ranked above family practice physicians and physicians from many other specialties in regards to NM competency. What Does this Mean for Physical Therapists? Physical therapists are some of the most competent healthcare practitioners in regards to diagnosing and treatment neuro-muscular conditions. The American medical system does not properly train physicians to treat these conditions. PT's need to be present to assist in diagnosis, plan of care, and prognosis for these individuals. Secondly, we need to do a better job educating our referral sources on what we do and why we do it. Most physicians do their residency training in a hospital setting. Their picture of physical therapy is confined to their experiences. Many physicians do not know the vast capabilities of our treatments. This is our opportunity to educate. -Jim  Like this post? Check our more on our Insider Access Page! Come learn from Jim Heafner and Chris Fox in person. We recently partnered with OPTIM Physical Therapy for their COMT program is Scottsdale, AZ.  You may have seen some posts earlier on our site about OPTIM Physical Therapy. Several months ago, Chris and Jim partnered with OPTIM Physical Therapy to create a COMT program based out of Scottsdale, AZ. The mission of the program is to create a residency-like experience for those who are unable to make the financial and location commitment. The program consists of 6 weekend-long courses on-site, in addition to Medbridge courses and online mentoring between classes. Throughout the year, the class as a whole will improve their clinical skills and reasoning while working as a team. Check out the official OPTIM website for more information  One of the hardest things to do in the clinic is to regularly practice things at which you are uncomfortable or less skilled. Most physical therapists work a busy day with patients and have notes to complete afterwards. The desire to do anything PT-related outside of those obligations can be exhausting. What we must do as clinicians, if we are to regularly improve, is reflect upon our weaknesses. They often can be difficult to identify, because we think we are examining our patients as efficiently and effectively as possible. But what lies unknown remains unknown. An easy way to start reviewing weakness is selecting techniques or other aspects of care with which you are less successful. Maybe it includes a lumbar manipulation or educating a patient on pain science. A more difficult weakness to identify is that which you are unaware is occurring. There are a couple methods of reflection I like to use for these. One is to review groupings of patients that have had less than optimal outcomes with your care. Maybe there is something else that should be included in managing the patient? Another method is to regularly review other PT blogs or courses that may point out examination or treatment techniques with which you have less experience. So how do we manage these things? For the technique or education aspects, it is simple - practice. To develop an expertise level at something, it requires lots and lots of practice. This is easier said than done for some things. For example, if you want to practice lumbar segmental mobility assessment, you can perform this on every one of your lower quarter patients. You will know more than almost every one of your patients, so go ahead and practice assessment techniques. You will notice differences between tissues and segments far more easily over time. Now, certain treatment techniques should not be practiced on patients as liberally. For example, cervical manipulations carry some level of inherent risk, so it is essential the clinician already have sufficient skill when performing. These sorts of techniques should be practiced for prolonged periods outside of patient care before performing on patients. For more non-technical aspects, it may benefit from some form of peer discussion or mentoring. As we've said many times before, it helps to have multiple perspectives in clinical development. Someone may have had some other success or experience that could benefit you in the future. Regardless of how you work on your weakness, it is important that we take the time to identify them and then address them. -Chris
Like this post? Then check out the Insider Access Page for advanced content! And check out similar posts below!
 Forward Head Posture anyone? Forward Head Posture anyone? First rib dysfunction is an often overlooked positional fault when assessing shoulder and/or cervical dysfunction. However, with how often I see postural faults on a weekly basis it has become a primary assessment for me in my shoulder and neck cases. The first rib has attachments to the scalenes, serratus, and subclavius. It is important in breathing and shoulder movements. A few months back I was warming up before one of my weight lifting sessions and did a few shrugs to finish off. I felt a pop in my neck and immediately had pain and limited ROM. Naturally I walked right out of the gym. I couldn't sleep or move my head from the increased stiffness. Fortunately, I had no neural symptoms. What remained was stiffness and pain that was excruciating. The culprit: the first rib. My first rib elevated and put my levators and upper traps on spasm, locking up around it. However with first rib mobilizations, soft tissue mobility of the upper traps, scalenes, and levators, in three days I was pain free and had full ROM. I worked on pain free ROM every hour on the hour in addition to my therapy. The point of this is to remind us of the importance of first rib dysfunction. I typically see it with my patients with poor posture and it tends to immediately improve patients cervical ROM when they are stiff. Next time you see a patient with limited cervical ROM or increased stiffness check out the first rib in addition to the t-spine and c-spine. - Brian Want to know how to treat cervical and first rib problems? Check out the Insider Access page for manual therapy techniques and assessment techniques! Also- check out Brian's recent published posts on Paleohacks. http://blog.paleohacks.com/why-stretching-isnt-helping/
 As my clinical knowledge and understanding of the nervous system continues to develop, I am finding that "muscle strength" is a relative term. In a previous post, Chris discussed how performing repeated movements can immediately improve an individuals strength. Similar to repeated movements, joint manipulation has shown similar results clinically. The exact mechanism by which a manipulation works is unknown. The most recent evidence suggests that it is multi-factorial. Some proposed effects of manipulation include: 1) Mechanical- breaking up intra-articular lesions 2) Neurological- "resets" nocioceptive pathways and mechanoreceptors 3) Hydraulic- changes in synovial fluid viscosity 4) Relaxation- alter muscle tonicity & restore blood flow 5) Psychological- both laying hands on the patient & hearing a "pop" are strong influences A clinical example you can test tomorrow is assessing lower trapezius strength, then performing different manipulations, and reassessing the strength after each manipulation. The three manipulations I recommend performing are a supine thoracic manipulation, a CT junction manipulation, and C3-C4 manipulation. I want to note that restrictions may not always be found in these regions. Remember: neurophysiological effects can have a profound impact on pain and function. Why Perform These 3 Manipulations?
Like this post? Check out our insider access page to see more clinical reasoning similar to this!
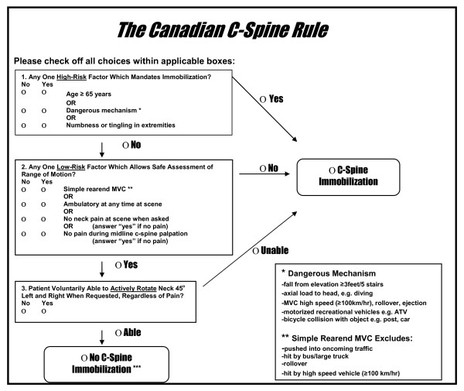
One of the more difficult types of diagnoses to manage in my opinion is neck pain after a motor vehicle accident (MVA). The patient often presents with some form of hypersensitization and a high fear avoidance behavior. This alone makes treatment difficult as the patients typically do not want to do much because "everything hurts." Prior to treating the patient (or even performing certain exam measures), it is essential that you review how the patient matches up with the Canadian Cervical Spine Rules. Check out the flowchart below. Should your patient meet the criteria, they should be referred for x-rays. If your patient doesn't meet the criteria, you can proceed with completing your examination more thoroughly. Treating patients with whiplash can be difficult as 2% of patients will still have significant pain and limitations a year after the accident. What complicates things further is that often there is a delay between the accident and when the patient actually seeks physical therapy treatment. This can be associated with central sensitization. These patients absolutely will benefit from therapeutic neuroscience education (TNE) in order to raise their pain threshold. Over the last year, I have noticed a trend in success with treatment options for patients following an MVA. Initially, I use IASTM (Instrument-Assisted Soft Tissue Mobilization) to the cervical and scapular musculature. This provides a non-threatening stimulus to again re-educate the patient's nervous system about how a normal input should be perceived. Once the patient is about 3 weeks s/p MVA, I typically implement some repeated motions (usually retractions or retractions with extension) hourly. This re-educates the patient's nervous system that end-ranges of cervical AROM can be non-threatening as well when given enough input. It's possible the patient can begin repeated motions earlier or later, but I typically find that patients are too hypersensitive earlier to get to end-range. Manipulations are often used to affect neurodynamics. The issue with patients suffering from whiplash is that their tissues are injured from an overstretch. A manipulation, in some theories, puts a stretch on the tissue as well, so early on may be contra-indicated. I will usually wait until the patient is 6 weeks s/p MVA before I consider performing a manipulation and will start with one directed towards the thoracic spine. Patient also frequently respond to some form of mild traction, so I include a manual component as well. What sort of treatments have you found to be successful with MVA's? Do you utilize manipulations and at what point do you feel it is safe? -Chris
Like this post? Then check out the Insider Access Page for advanced content! And check out similar posts below!
Fryette's laws of spinal coupling can be a difficult concept to grasp. They are not taught in depth in PT school, but we frequently hear about them as if we are supposed to follow them as 'laws of movement.' In reality, these laws have questionable validity. In fact, the term law should be taken loosely. These guidelines should be carefully utilized in diagnosing spinal conditions. With that being said, the theories of spinal coupling can assist with your examination and treatment. if the lumbar spine is in a neutral position, sidebending creates contralateral rotation (Law 1). For example, left sidebending should cause a simultaneous right rotation. If the spine does not start in neutral, sidebending and rotation occur in the same direction. For example, a patient with increased lordosis does not start in neutral. When they sidebend left, they will also rotate left. The video below does a very nice job portraying these 2 patterns. In addition to spinal coupling, remember to assess for the order of movement, a loss of movement, aberrant movements, pain or stiffness, and uniformity of the spinal curve when performing lumbar spine active range of motion.. Learn more by reading my Lumbar Spine AROM post! -Jim
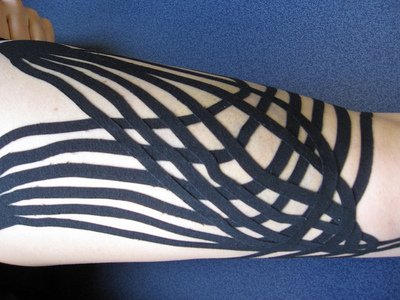
We have discussed before about the potential effect of placebo. It can play quite a significant role and should never be discounted. Probably one of the specialties of PT that is most frequently challenged by a patient's prior expectations is the orthopaedic setting. Patients come in asking about the "wonders of ultrasound" or possibly kinesiotape after seeing their favorite athlete wear it all over their body. With the push for evidence-based practice, research has shown little support for these interventions, leading to many PT's tossing them out of their treatment options. People often forget that one of the 3 pillars of evidence based practice is patient values. Patient expectation is a component of the patient values pillar. If a patient states they had success with one of the less-supported treatments in the past and they expect to receive it again, we should implement it. If we ignore it, the patient-clinician relationship could become compromised, leading to a lack of improvement. I recently have had some patients that expected Instrument-Assisted Soft Tissue Mobilization (IASTM) to be deeper and more forceful than I usually provide. Many of the brand names build their philosophy off of "realigning collage" or "initiating the inflammatory response," while current research states that amount of force is not necessary. When patients do expect that force, however, I typically increase the force I apply, but still not as intense as others. That doesn't mean it should be performed blindly. The unsupported treatments may be provided, but they should be coupled with different treatments that have more support. In application of a treatment, I'll educate the patient how the support behind the technique is limited, but we will couple it with components that have a stronger background of support. With the advancements in pain science research, the power of the mind in its relation to pain is just beginning to be realized. If the patient is expecting certain aspects of treatment, we should consider incorporating it, otherwise the patient may "refuse" to get better. No single study can control for a patient's expectations, so no study is perfect. Next time a patient reports prior success with a certain mode of treatment, don't be so quick to set it aside. -Chris Have you ever wanted to enroll in a residency but not have the time or ability to financially commit? Jim Heafner, PT, DPT, OCS, SFMA and Chris Fox, PT, DPT, OCS, SFMA from The Student Physical Therapist have partnered with Dana Tew, PT, DPT, OCS, FAAOMPT from Optim Physical Therapy to create a COMT program starting in October! The mission of the program is to develop the clinical reasoning and manual skills of the participants over the course of a year through a structure similar to a residency, but without the financial sacrifice and significant time commitment, The program will help you to prepare for the OCS, improve your outcomes, and qualify for Fellowship enrollment. Check out the program for more details at www.optimfellowship.com and let us know if you have any questions! Like this post? Then check out the Insider Access Page for advanced content! And check out similar posts below!
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|












 RSS Feed
RSS Feed