- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
When setting up a patient's schedule after doing an evaluation, there is typically a preference from both the therapist and patients for continuity. But in a modern physical therapy clinic, it is difficult and rare to meet this demand. Many patients either want to come in before or after work, leading to a backlog of patient requests for those time slots. With working in a clinic with multiple therapists, patients often end up having several treatment sessions with other therapists. This can be frustrating for several reasons. When evaluating a patient, we set up a plan of care on paper and in our minds for how to manage that patient's condition. Maybe we have particular manual therapy techniques or exercises we want performed in particular sessions. It's possible, and likely, that other therapists may not know what you are looking for with specific exercises or even how to perform certain manual techniques. When treating someone else's patient, we become hesitant to adjust any treatments the patient might receive out of fear of altering the main therapist's plan of care, having the patient lose faith in the main therapist, or at worst possibly regress a patient! That being said, there are definitely benefits to having multiple therapists treat a patient occasionally. As thorough as we like to think we are with our evaluations, it is not impossible for there to be something that we missed. Whether we just weren't thorough enough with our assessment or we lack the experience and skill to pick up an essential impairment, a second set of eyes can be extremely beneficial. That ties right in to the benefit of various backgrounds for treatment. Perhaps you are aware of a treatment method that would be extremely useful for a patient, but you don't actually know how to do it. With all the continuing education courses available and various schools for physical therapy, it is possible that other clinicians in your setting may have those skills. I am fortunate to work in a clinic with 3 other therapists, all with different backgrounds. I have already been utilizing their unique skill-set in my 2 months of working there. So which is better? As in most cases, a little bit of both can be preferable. Personally, I think a consistent relationship between one physical therapist and one patient is the better option and cannot be underestimated. The trust developed between the PT and the patient may alone enhance the patient's experience. It is also far easier to maintain the original plan of care that was set in place. However, when we do notice lack of progress in our patients and run out of answers, it is definitely beneficial having another physical therapist work on and assess the patient. In the end, patient outcomes are what is most important, and we likely will not always have the answer. That second set of eyes may be just what is necessary to reach the remaining goals.
-Chris
1 Comment
Overview: The SLUMP test is a highly sensitive test that can elicit positive neural tension in even asymptomatic individuals. The test can be used in conjunction with other neural tension testing (straight leg raise) and is often a great concordant (asterisk) sign to demonstrate within treatment progress. Due to the complexity of this test, consistency is key. To ensure you are performing the SLUMP correctly, you must be systematic. Perform the same order of events with every patient, every time. Proper Start Position: 1) The patient sits upright with their popliteal creases against the back of the plinth. 2) The therapist presses the knees together and releases them to maintain a neutral position of the lower extremities 3) The patient folds their arms behind their low back *These 3 steps are to maximize consistency Performing the Test: 1) Have the patient slowly slouch from their thorax spine (this will also create lumbar flexion) 2) SLOWLY flex the head toward the sternum 3) SLOWLY begin extending the knee* 4) SLOWLY dorsiflex the ankle* 5) Extend the cervical spine (move a distant component) *In steps 2, 3, and 4, I emphasize SLOWLY because the test is intended to pick up adverse neural tension. Many individuals will push past the onset of neural tension and confound the results of the examination. Remember, neural tension is only positive if their is a side to side difference, reproduces their primary complaint of pain, and if symptoms change by moving a distant component. Turn the SLUMP Test into a Treatment: Fortunately, setup and treatment for positive neural tension findings can be very similar. Check out our HEP program page on Slump Sciatic Nerve Glides to improve your intervention selection. Additionally, for more information on neurodynamic testing and treatment check out our guest post from Darrin Staloch. -Jim Heafner PT, DPT, OCS Learn more about the Lumbar Exam!TSPT Lumbar Spine course has over 5 hours of lecture dedicated to lumbar examination, treatment, biomechanics, and more! The course outlines multiple treatment options include Sahrmann, repeated motions, and manipulative therapy. Click below to learn more!
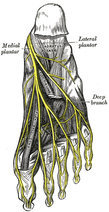 Plantar Fasciosis can be a very difficult condition to treat because of the intricate anatomy of the foot and ankle complex. To complicate issues, we now know that many lower quarter problems root from lumbopelvic and hip dysfunction as well. In previous posts, TSPT has done a literature review of the condition as well as talked about new treatment methods regarding plantar fasciosis. In these posts, one aspect of management we did not discuss in depth is assessing for neuropathic pain. From my clinical experiences and the experiences of my colleagues at the Harris Health System, many patients with plantar fasciosis have positive neural provocation tests for the distal branches of the tibial nerve. Anatomy Review After the tibial nerve passes around the medial malleolus, it splits into three distal branches: the medial plantar nerve, lateral plantar nerve, and medial calcaneal branch. Specifically, the lateral plantar nerve innervates the fifth and lateral 1/2 of the fourth toes and provides motor input to many of the intrinsic foot muscles. The nerve passes laterally across the foot and splits between the flexor digitorum brevis and quadratus plantae. Assessment To assess for tibial nerve adverse neural tension, have the patient lie supine. Passively extend the toes, dorsiflex and evert the ankle. This combined movement place a stress across the tibial nerve and its distal branches. Ask the patient if this position changes their primary symptoms (better, worse, or the same). Next, passively perform a straight leg raise maintaining the foot and ankle components. If this position recreates their primary symptoms, they have positive neural tension in the tibial nerve* (remember to test bilaterally as well). To further assess the tibial nerve, adduct and internally rotate the lower extremity. If the test is positive, appropriate treatment options include nerve sliders, tensioners, and manual therapy. *When performing a straight leg raise, you are changing the hip component. No musculoskeletal structure courses from the hip to the ankle, so if symptoms change it must be the nervous system that is being assessed. Conclusion -Lateral plantar nerve pain can be a contributing factor to plantar fasciosis pain. -By performing the proper assessment (discussed above), you can identify if neural tension is part of your patient's symptoms. -Do not underestimate the impact of the peripheral nervous system in musculoskeletal dysfunction. Lower Extremity Peripheral Nerve Testing [Video taken from TSPT Insider Access Library- subscribe to learn other advanced assessments!] Author: Jim Heafner PT, DPT, OCS is one of the founders of The Student Physical Therapist. He is owner of Heafner Health Physical Therapy in Boulder, Colorado. Are You on the Inside?Looking for advanced sports and orthopedic content? Take a look at our BRAND NEW Insider Access pages! New video and lecture content added monthly.
As many of you know, we recently launched a Home Exercise Portion to our website. They consist of many exercises that we prescribe and programs like VHI don't contain. I wanted to highlight one exercise today, the Quad Rock Back, because of all of uses for it. The exercise is a staple of the Shirley Sahrmann philosophy. While it is listed under the "Low Back" section, it is often prescribed for cervical, shoulder, and hip patients as well. We will break down how the exercise can be used for each region. As described in the video, when this exercise is performed for cervical patients, often the head begins to extend or flex while rocking back. This is a result of abnormal movement and compensatory patterns in the cervical spine. For cervical spine patients, we encourage a chin tuck so that no neck movement occurs during the rocking.
There are many reasons why I like to give this exercise to shoulder and hip patients, one being joint compression. We are taught in our manual therapy classes that joint compression can be beneficial for healing; it also can help mobilize the posterior capsule. It also helps mimic the developmental patterns of weight bearing on the upper extremities, and thus is a critical part of rehabilitation. Additionally, the quad rock back exercise can be use to help normalize scapulohumeral movement patterns and avoid any compensatory activity. While performing the exercise, the movement can be completed by actively flexing the hips, instead of pushing away with the UE's. This allows the shoulder to move in a more normal pattern. Similarly, the exercise can help with unwanted hip musculature activity. By reversing the directions (instructing the patient to push with the hands and not actively flex the hips), the patient can decrease abnormal femoral head sliding and thus compete hip flexion less painfully. The exercise can be used both for treating and assessing and low back dysfunctions, and not just because it is one of the more comfortable positions for low back pain. If you take your patient into quadruped and have them rock back, pay attention to the pelvis, hips, and low back. You may note a deviation to one side, suggesting increased muscle activity, stiffness, or movement patterns. Often you will note premature lumbar flexion compared to end-range hip flexion. This is secondary to all the sitting we do throughout the day - our lumbar spine becomes more flexible compared to the hip! By encouraging the patient to maintain a stable lumbar spine while rocking back (this can be done by placing a stick across the low back - if it falls off, we know there has been abnormal movement). This teaches our patients to isolate hip movement from back movement. While I may not subscribe to all of Sahrmann's theories on movement impairment syndromes, especially in the acute phase, I do appreciate the focus she places on changing compensatory patterns with her exercises. Many of these patterns stem from abnormal postures or repetitive tasks that we perform throughout our daily lives. The rehab focuses on resisting any changes in movement that occur as a result. I have found that I get better results with incorporating repeated motions into my treatment, but I continued to use Sahrmann exercises to try and retrain movement afterwords. -Chris  A few weeks back, I wrote a post about assessing for Lumbar Extension Rotation Syndrome (ERS) in low back pain patients. Since then I have received several comments from people wanting information regarding treatment options for this condition. Overview A typical patient presentation includes age >55 years old, chronic low back pain, and may be involved in a rotational sport (golf, tennis, etc). On physical examination, you will observe an exaggerated lumbar lordosis, paraspinal muscle asymmetry, excessive pelvic rotation during gait, and hinging during cardinal plane extension testing. They will often complain of unilateral lumbar pain that increases with extension and is relieved with non-weight bearing lumbar flexion. Generally a patient with ERS hyperextends their low back, which does not allow the gluts to fire properly. Treatment For the purposes of this post, I want to focus on core stability and lumbopelvic disassociation. I find that pure hip strengthening is not appropriate early on because the patient cannot adequately engage their gluteals without lumbar compensation. Since the patient has excessive lumbar lordosis and hinging during functional movements, addressing core stability is essential. Additionally, strengthening and motor control of the hip extensors and external rotators is important once the core has sufficient control. Manual therapy is performed on a patient-to-patient basis depending on individual impairments found during the physical examination. Since the patient is generally hypermobile at the hinging segment, they are hypomobilie cranially or caudally. Thoracic and lumbar mobilizations and manipulations are appropriate for the appropriate patient. Core Stability Assuming the patient has low irritability levels and good body awareness, I will usually begin TherEx by retraining the transversus abdominus (TrA) in supine. After the patient can maintain a neutral low back position, I will incorporate the bent knee fall out exercise using a blood pressure cuff for additional cueing. Many progressions of the blood pressure cuff are appropriate until the patient demonstrates good isolation of the TrA in supine. As the patient progresses, I take them through a progression of exercises in quadruped to ensure the patient can maintain a neutral low back posture in a gravity independent position. The progression includes isolated TrA contraction, TrA hand heel rocks (see below), and removing limbs from the table (alternating shoulder flexion, alternating hip extension, then birddog exercises). When the patient can demonstrate good control in quadruped, I address core control in spinal weight bearing. In standing, I have found using the wall as an external cue helps the patient 'find' their TrA. When appropriate, begin functional training in standing by incorporating mini-squats, lunges, and other upper and lower extremity disassociation exercises. Below is a progression of 3 common exercises I prescribe for ERS from supine to standing.
Please let me know if you have any questions or would like more information regarding treatment options of extension rotation syndrome. -Jim  Recently, The Manual Therapist wrote a blog post about what is most important when treating a patient: the what, the why, and the how. To relate it more directly, what you have refers to specific diagnoses. Why you have it refers to the theory of why the pathology occurred, i.e. movement impairment syndromes. The how refers to how we actually treat and assess. Much of medicine and physical therapy is often stuck in the "what" phase. We tend to assign diagnoses to tissue pathology and often look to treat what we believe is the source of the pain, not the original cause. Many physical therapists are moving towards the "why" mindset where we look at a more complete chain of the body to determine why our patients are in pain. This typically leads to a more well-rounded treatment approach. The "how" comes back to what we are actually doing and how we are treating our patients. I recommend reading the original post by Dr. E to get further clarification. This post comes with good timing in the wake of Tiger Woods' "sacrum" comments. In case you missed it, Tiger Woods recently played in a golf tournament and had to withdraw, because he claimed his "sacrum went out." As a result, there was a backlash from much of the young PT community claiming how it was a horrible diagnosis, Woods' physical therapist had poor communication skills, etc. The discussion lead to many physical therapists and physical therapy students ranting about how the research for SIJ Dysfunction as a diagnosis is poorly supported based on higher level evidence (which is correct) and some even saying how the SIJ doesn't move at all. Based on these comments, it would appear many do not assess or treat the Sacroiliac Joint. While I may agree that we shouldn't worry about actual tissue diagnoses, I get frustrated by people's reluctance regarding any potential SIJ treatment given my personal clinical success. In the residency at Scottsdale Healthcare, we were taught various assessment and treatment techniques for the SIJ, but the distraction manipulation could be used as a "shotgun" approach and treat typically any form of SIJ dysfunction. In my limited experience, in the patients I feel would benefit from the manipulation, they tend to be 100% within just a few visits. Now a manipulation by itself is never the answer alone, but it can be an extremely useful tool. We need to build on preventing future recurrences of pain and teach our patients to maintain improvement independently. Some patient's arrive at clinic in excruciating pain and are nearly pain-free after manual treatment. A manipulation and mobilization are not the only potential treatment for what some would diagnose "SIJ Dysfunction." Repeated motions towards the directional preference may be appropriate as well. Basically, many of treatment techniques like these have theories to support them, but the evidence is not always as established. That doesn't mean successful treatment techniques should be discounted. I again recognize our limited ability (and importance) of truly diagnosing what we think we see with the SIJ, but I must continue to stress the impact of when we assess, treat, and reassess. This is the importance of the how I discussed at the beginning. If the patient feels better immediately after a treatment technique, something I did had the desired effect! We currently are unable to be certain in knowing the exact mechanism our techniques have, but we should not ignore positive results. I have written extensively in the past about the problems with the studies regarding manual therapy, especially the SIJ, but that is not important in the end. What is important is that we find effective ways in getting our patients better as soon as possible. If that means doing a manipulation or mobilization where we think we are targeting the SIJ, then so be it. Do not let the limitations in higher level research prevent you from providing your patients with the most effective care. -Chris
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|












 RSS Feed
RSS Feed