- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 Last week, I was reading the most recent JOSPT's editorial on chronic pain: "When Chronic Pain is Not 'Chronic Pain': Lessons from 3 Decades of Pain." While an editorial (and the case study presented within it) is not a standard for evidence-based practice, the article does an excellent job of stating that just because we think something is correct today, doesn't mean it will be in 10 years. If you aren't familiar with the article, a case is presented on an individual that had leg pain over 3 decades of his life and was treated with the different "fads" of each decade: McKenzie, core stabilization, and more recently pain science. The individual in the case study showed little change in his symptoms until an exercise-based ABI was performed and revealed circulatory issues in his LE. Once the vascular issue was addressed surgically, the individual was back to his PLOF from 30+ years ago. Obviously, a case study doesn't hold much weight by itself, but this article does an excellent job of getting us thinking about the state of physical therapy and our overall perception of evidence-based practice. At each point that care was being delivered to the individual, the treatment was perceived as best practice. Today addressing pain science and biopsychosocial aspects is the more evidence-based treatment. If anything, research today should tell us that there is a lot out there that we don't understand, and we are prone to blindly attribute the effects to the nervous system or the mind in general. As the author of the article stated, it will be interesting to see in 10-20 years how the practice of PT changes. While we should absolutely base our treatments in what the evidence suggests while practicing, we shouldn't be so quick to stop researching other techniques that may prove beneficial down the road as we continue to learn more. -Dr. Chris Fox, PT, DPT, OCS
1 Comment
One of the foundations of physical therapy is exercise prescription. While every PT school is required to teach their students the fundamentals of exercise physiology and prescription, many would agree that what should be an expertise of the profession is often a weakness. More and more research is showing that exercise is likely one of the best interventions we can provide as health care professionals, for both tissue healing and addressing biopsychosocial factors. A common mistake many are prone to (myself included) is insufficiently challenging the patient. Whether truly focusing on strength, proper tissue loading, or for psychological benefit, it is our duty to properly load our patients. One aspect we should consider is if we are having our patients exercise on a table too much. While there is a time and place for some exercises there, it is not the only place our patients should be challenged. Getting exercises into closed-kinetic chain movements simulates more daily motions that table-based ones. Additionally, we can progress the load our patients are having to move off the table. While those aspects are likely pretty obvious, I believe it can also be motivating to the patient psychologically. I often try and have my patients perform exercises like goblet squats, deadlifts, and others that they may have never thought possible for themselves. It can be extremely exciting! The additional load can also help to desensitize the affected tissue both locally and centrally, meaning the individual isn't overly focused on the area. While challenging our patients with more advanced exercises has its benefits on improving function and mental health, it is still essential that we recognize the foundations of exercise physiology. If we are truly looking to strengthen a muscle, we must focus our efforts on the proper fuel system and rep scheme. If a patient is performing 20 repetitions of an exercise without any struggle, they aren't strengthening. I'm not saying there isn't a place for an exercise like that or even that there isn't a benefit, but if we are truly wanting to strengthen them, the load must be increased. -Dr. Chris Fox, PT, DPT, OCS
Below are my TOP 10 Physical Therapy beliefs. These are not meant to be offensive, but merely thought provoking. I hope you can resonate with one or two of them. Please share with a friend! 10. Physical therapists have unique opportunities to change people's lives everyday. Change is not easy, but passion and persistence usually prevail! 9. We do not have all the answers. Twenty years ago we thought ultrasound was good. Ten years ago we believed manipulations worked for biomechanical reasons. Our current research will only be developed and improved upon tomorrow. Look ahead, not behind! 8. In our current society, we have too many under qualified people teaching others how to move (look at our current fitness industry). Physical therapists are the movement and pain experts. We must be active in the community, teaching trainers, coaches, etc... how to move. 7. Orthopedic pains are commonly problems of system overload, not isolated issues. Do not underestimate the value of nutrition, sleep, stress, and lifestyle. 6. Connecting with someone on a human level is enough to get them better. There is plenty of pain and suffering in the world. More low trap or gluteal strength is not always the answer! 5. Shutting down other health professionals is a poor example of our character as a profession. It is an unacceptable way to state an opinion and should never happen. 4. There is a reason massage therapy is a >12 billion dollar industry. While it might not work on paper, people enjoy it and are willing to spend their own cash on it. More importantly, people tell their friends about how great it is. Physical Therapy needs to become a profession that people value and are willing to spend their own money on. 3. We are the only doctoral profession embarrassed to tell people we are doctors! This has got to change. We worked extremely hard for those letters. Embrace them. 2. We search too hard for answers to our client's problems. If we simply slow down to listen, the solution usually presents itself. 1. Physical Therapists should be the provider of choice for all musculoskeletal and movement based problems. We have more than enough intelligence and offer an amazing product. Now, it comes down to our ability to sell- not shamelessly, but with passion and pride! Get out and sell our amazing profession.  Author: Jim Heafner PT, DPT, OCS Instagram: @HeafnerHealth Jim is one of the founders of The Student Physical Therapy. He is owner of Heafner Health Physical Therapy in Boulder, Colorado. Want to learn more from the author: Check out his Ebook and other online resources: 1) The Guide to Efficient Physical Therapy Examination 2) The Anatomy of Human Movement (Save $10 on either offering by using the promo code: Top10)  One year ago I entered into the OPTIM Certified Orthopedic Manual Therapy Program. I had been wanting to sink my teeth into something of substance to improve my skills and thought process for some time now and felt a program that was longer than one weekend would be best. I looked into other COMT programs but found them to be unorganized and very lengthy to complete the entire program. Fortunately my colleagues from TSPT and friends Dr. Chris Fox and Dr. Jim Heafner were already instructors for the OPTIM program. When looking into OPTIM’s program what attracted me the most was the ecletic approach they took. What I mean by that is that one school of thought was not the focus of the year long program. Instead, many different approaches were taught and offered. To me, this was very important. Another thing that stuck out to me was the emphasis on learning more on pain science. This was an area that I felt PT school and residency was lacking. Thus, learning this was important to me. Lastly, I knew from my colleagues Chris and Jim that ample time would be spent teaching and practicing techniques. So, one year later I am approaching the completion of the program. I can honestly say it was money and time well spent (and significantly cheaper than other COMT programs I might add). The program is really more like a residency as it requires quite a bit of time every month outside of the 7 weekends spent in Phoenix, AZ. There is weekly mentoring sessions online via Zoom call, Medbridge courses, and workbooks to be studied and reviewed. Additionally each weekend class goes over techniques and concepts from previous weekends to ensure constant repetition. After all, manual therapy is really a motor skill that must be practiced over and over again to improve upon. For those of you interested in seeking quality learning and are dedicated to putting the time in to really make a difference in your skills I would highly recommend this program. And don’t worry, students are also welcome and I think it’s a great adjunct to PT school. Feel free to email me for more information or check out the OPTIM website here: http://www.optimfellowship.com/ Dr. Brian Schwabe, PT, DPT, SCS, CSCS IG:@brianschwabedpt Recently, a fellow physical therapist and friend came to me for some guidance regarding a case he was having difficulty managing. Below is a synopsis of his initial evaluation. After reading his initial evaluation, please write down a few notes or comments (positives, negatives, things you may have done differently, or further questions). Following his evaluation, I provided my response to certain questions and treatment ideas to provide further insight into his case. Therapist Initial Evaluation (my friend):Main Complaint: Electric shock from the right low back to distal hamstring with a variety of different movements. Prior injection resolved S1 distribution numbness. Static Posture: -Spine: normal spine curves - Hips: narrow, symmetrical hips - Knee/ankle: genu varum Palpation: -Tenderness and tightness into piriformis Functional movement testing: -Inline lunge: increased hip flexion, but movement was painfree -Hurdle step: R lower extremity in WB- poor hip motor control -Gait: no pelvic innom. rotation - Squat: inc hip flexion, HS avoidance, R sided lumbar pain "catching" - SL squat: medial collapse, 'shakiness bilat' - SL stance: R sided LOB - SL step down: avoided WB through R via trendelenburg - Elbow flexion iso #8: paraspinal recruitment thoracic/lumbar, no TA activation Lumbar stability: -Bent knee fall out: min TA activation -Hooklying marches: mod TA activation; limited hip flexion to 105 deg because it will trigger pain -ASLR: tight HS, no neural symptoms -PSLR: 50% of WNL with back pain Muscle length testing: HS 90/90: R 145, L 155 + Thomas B, inc sx L Ely's + at 110 knee flexion, R WNL + ITB R, WNL L Passive range of motion: Hip 110% WNL with catch during full flexion Overall Assessment: Pt is a 45-year old male presenting with chronic, insidious onset of low back pain with R sided, electric shock sensation down back of leg and into distal hamstring. Pt has movement impairments with hurdle step (R WB poor hip motor control), gait with minimal pelvic innominate rotation, SL squat with medial knee collapse. Additionally he had frequent R lumbar spasming reported during exam. Pt has functional limitations in running, rowing, and ADLs, sleeping. Initial HEP prescribed: L thomas test stretch, L hip flexor Stretch, hooklying isometric marching My Response to Evaluation: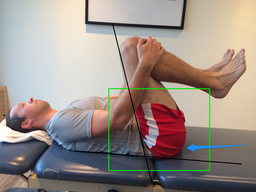 1) From his symptom description and testing, we know he has some level of nerve irritation. I would perform a SLUMP test. If positive, neural glides could be a great treatment for symptom relief. 2) How is his hip mobility, hip IR/ER range of motion and end-feel? Commonly limited hip mobility places stress on the lumbar spine due to improper loading through the hip joints (from his SL squat and other functional movements, he appears to be offloading his right hip). 3) How is his thoracic spine mobility? 4) The patient appears to have increased hip flexion with various movements. Be sure this is not actually early/excessive lumbar flexion. (See link to a post I wrote on hip flexion vs. lumbar flexion 5) The patient appears to have poor coordination between the lumbar spine and hip joints. I would look at more basic movements, such as hand heel rocks (butt to heels in quadruped) to assess lumbopelvic disassociation and general spinal mobility. 6) How is lumbar extension? Many people lack lumbar extension due to prolonged flexion (see point 4 above) and become sensitive to that movement. Retraining lumbar extension throughout repeated loading is often beneficial for range of motion, mobility, and nerve irritation. My Response Assessment: Incorporate further mobility exercises for the hip and thoracic spine (likely). Stretching (as he initially prescribed) can further excite nerve symptoms and cause irritation. Additionally, I would incorporate more neural tensioning exercises for symptom management. Since the nerve is irritated, add the recumbent bike or low level total gym for nerve nutrition and proper loading through the hip. From a manual therapy perspective, I have seen good results with lateral hip mobilizations using a mobilization belt. This can improve hip mobility and reduce neural tension. Finally, basic exercises like Cat/Cow are good for emphasizing thoracic extension and are a precursor for lumbopelvic mechanics. -Jim Heafner PT, DPT, OCS |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|













 RSS Feed
RSS Feed