- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 With the continued rise of text-neck and poor posture, mobility exercises for patients is becoming even more crucial. Teaching our patients self mobility can be vital to their compliance in a treatment program. When patients have shoulder mobility issues the most common areas tend to be pecs, lats, and upper traps. However, when dealing with shoulder issues be sure not to forget about the influence of the kinetic chain. Specific to shoulder mobility issues is the hips. Many times hip stiffness can cause a "tone" problem in the lats and vice versa. Check out an article I wrote for some of the self mobility exercises I typically give my patients: http://blog.paleohacks.com/shoulder-mobility-exercises/ - Brian
0 Comments
Optim COMT and TSPT Insider Access Sample: Movement Impairment Syndromes of the Lumbar Spine Lecture2/28/2016 In the last course for Optim's COMT program, we covered examination and treatment of the lumbar spine, including many different manual techniques and repeated motions. However, we ran out of time so we were unable to present the Movement Impairment Syndromes (MIS) Foundation and Lumbar Spine lecture. Below is a recording of the lecture for our program participants, which we have made available to TSPT Insider Access Page members as well. This is a sample of what we are presenting both for Optim and TSPT. Now I am by no means a "Sahrmann PT," but I tried to provide a general summary of the foundations of MIS. If you have any further questions about what we offer at Optim or TSPT, please don't hesitate to contact me. In the next few months, we'll have some other videos come out for Optim as well, demonstrating our mentoring sessions and actual weekend courses. Enjoy! -Chris
The other day my student inquired about cash-based physical therapy services and reimbursement models. He mentioned that he would like to practice in a cash-based environment in the future. This statement surprised me for several reasons: 1) It is great to hear that students are considering other options than insurance based payments. Cash based PT was a distant thought for me while in school. 2) I wondered if schools teach about cash based payment options in school. If not, where are students receiving their information? As someone who will now be starting a cash based therapy practice in a few weeks, I wanted to share my top resources I have benefitted from on this subject. If you are interested in cash-based physical therapy, I would recommend checking out the following sources: 1) Aaron LeBauer: Anatomy of a Physical Therapy Cash Practice. Aaron's site has tons of free and premium information depending on your level of commitment. He offers a free CashPT Checklist that is a great starting point! 2) Top 10 Things You Must Do To Get New Patients. If you are getting into a cash-based service, you need to start thinking outside the box with our marketing strategies. 3) Jarod Carter's Interview with PT students on Cash-Based PT Services. Dr. Carter has written extensively on his success in the cash PT market. 4) WebPT blogposts "How to Equip Your Clinic for Cash-Pay Services." There are plenty of great articles and resources regarding cash-based payment models. Starting a practice is possible as long as you take the proper steps before opening your doors.
-Jim This coming week, Honor Health (formerly Scottsdale Healthcare) is hosting an open house for both the orthopaedic and neurological residencies. They can be attended either online or onsite. The orthopaedic residency has had 100% OCS success from past residents. The residency and the incredible faculty there played a significant role in my development as a PT. Be sure to check it out and let me know if you have any questions. Neuro Residency Open House 2/24/16 6:00-7:00 PM (Mountain Time) Ortho Residency Open House 2/25/16 6:00-7:00 PM (Mountain Time) To attend online, go the this link and RSVP to the open house you are interested in. If you would like to attend onsite, the open house will be held at the location below: 7301 E. 4th St. Scottsdale, AZ 85251 -Chris It is amazing to believe that I took the OCS examination nearly 1 year ago. As I look back on myself 1 year ago, I remember the extensive amounts of studying I did in the weeks leading up to the examination. One of the most difficult aspects regarding studying for the OCS is the lack of prep tests, quizzes, or guidance when preparing. In this post I want to review the TOP resources I utilized when studying for the OCS plus a few bonuses I would use now. 1) APTA Current Concepts and APTA Monographs. The Current Concepts is a series sponsored by the APTA which include a joint-by-joint breakdown of the anatomy, arthrokinematics, pathology, treatment, and sample questions at the end of each section. They are written by an expert on the subject matter and highlight many key components of the exam. 2) Clinical Practice Guidelines. The guidelines outline the highest level of evidence per diagnosis. Several questions are written on the information contained within the CPGs! 3) Ortho Secrets Textbook. This book consists of questions and answers regarding commonly misconceived PT questions. 4) OPTIM Weekly OCS Prep Quizzes. Find all the quizzes HERE. Chris and I have discussed the OCS examination in previous posts. Additionally, Brian has written about his experience with the SCS examination (see below for specific links). OCS Preparation Links: 1) TSPT OCS Link 1 2) TSPT OCS Link 2 SCS Preparation Link: 1) TSPT SCS Link 1 The last few weeks are tough, but keep pressing until the end. It will be worth it! -Jim
With the increased interest in specialization, more and more new graduates are looking towards starting off their professional careers with a residency. Residencies are an excellent method to develop your clinical reasoning and skills. Couple the many hours of class and lab-based learning with 1-on-1 mentoring and it creates a unique experience that can prove extremely beneficial. One of the issues, however, is that there is a much lower number of residency slots than people interested in residencies, which would potentially slow the progression of the profession to specialization. One method of filling that void includes various certifications and clinical development tracks. Occasional random continuing-education courses, while beneficial, do little to develop a clinical reasoning mindset, which is essential to begin working towards becoming an expert practitioner. There are many different certification series that you can choose from: manual therapy, McKenzie, pain science, SFMA, and more. Personally, starting out in the orthopaedic setting, I would recommend a COMT (or similar) program. There typically aren't restrictions on the number of applicants, due to the relatively high number of programs. The COMT programs enroll you in a set of courses that develop a clinical reasoning mindset to managing your patient's conditions over a year typically. While just glancing at programs appear expensive, they are significantly less than a typical residency. Residencies pay, at the highest, around $45,000/year. Depending on your setting and location, a COMT program may only cost a few thousand dollars and often is the same initial stepping stone as a residency when trying to enter a fellowship. One of the downsides of COMT programs is the usual lack of mentoring compared to residencies. However, at Optim, we provide online case discussion between courses to try and offer a component of it. Just because you may not get into a residency, doesn't mean you should abandon your drive to specialize. Look into all the options for different tracks to pursue and ask around if you have questions. Be sure to develop some sort of plan in order to work towards learning and practicing a system of care. -Chris
 Be more than just OPTIMistic when taking the OCS Exam. Be prepared! It's less than 1 month away. Take OPTIM OCS Quiz 7 to check your knowledge of the foot and ankle. Take Quiz 7 HERE! Additionally, OPTIM is officially now enrolling our 2016/2017 COMT and Fellowship cohorts in Scottsdale, AZ & Houston, TX! Learn more at OPTIM Website! Contact Jim or Chris with more information. Interested in Cash-based Physical Therapy? Check out Aaron LeBauer and other top names in Cash Pay Physical Therapy at Combined Sections Meeting this Thursday Feb. 18. Click HERE to learn more!
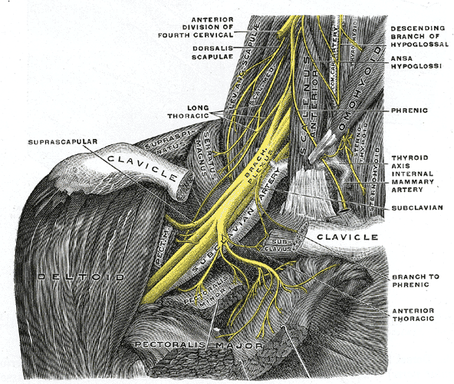
I'd been treating a patient s/p lateral epicondyle ORIF for awhile and noted both a subjective report of loss of biceps strength and visible atrophy of biceps. Initially, I didn't think it was too significant as the patient was not allowed to lift anything with his arm for a couple months. However, as the patient progressed through the later stages of rehab, the atrophy of the biceps remained, even as some strength returned. He had an MRI that revealed no biceps tendon injury, so he was referred to a neurologist. Further testing revealed the patient had the diagnosis of Parsonage-Turner Syndrome. Parsonage-Turner Syndrome is also known as acute idiopathic brachial neuritis, among other names. The cause is unknown, but is attributed to either viral origin or some form of autoimmune disorder. The neurologist told my patient it can occur after surgery as well. It afflicts 1.64 per 100,000 individuals. Typically the patient presents with pain in the upper quarter, followed up by the onset of muscle weakness and atrophy. What makes it stand out is that the atrophy and weakness remain as the pain subsides. Most of the background information I found associated Parsonage-Turner Syndrome with muscles of the RTC and proximal, however, it can vary as in the case of my patient. For proper diagnosis, be sure to have your patient referred to a neurologist for EMG and NCV. Once diagnosed, there are typically two stages for management. During the acute stage, the patient is instructed to rest and take the appropriate pain medication. Once the pain disappears, the patient should begin physical therapy in order to maintain joint mobility/flexibility and strength in the muscles. Typically, it takes several years to return to prior level of function (longer for elderly patients), and full strength may never return. As with any case that involves nerve origin, I recommend treating the whole chain as in the case of double crush syndrome. Be sure to address any joint/neural mobility restrictions found. While it is not 100% certain my patient has Parsonage-Turner Syndrome, I thought this would be an interesting pathology to discuss as I was previously unfamiliar with it. For more information, check out this study. Have any of you encountered this pathology before? -Chris
 Now that I caught you with the title...we know nothing in Physical Therapy is 'all about' one thing. The beauty and difficulty of the human body is our unique differences. There is not one thing that is the same for all of us. However, when dealing with back pain, we know the importance of proper strength and mobility of the hips is essential.  Throughout my lumbar evaluation, I look at the function of the hips in several planes. From the functional movements of gait analysis and squatting to AROM and strength testing, I try to gain an understanding how people use their hips. If a patient is lacking range of motion, their mobility will likely arise from the lumbar spine. Contrarily if the hips are lacking strength, the low back will attempt to compensate for the weakness. For example, when someone performs a squat, if they are lacking hip strength, they will likely use their low back to ascend from the squatted position. This excessive lumbar hyperextension demonstrates an inability to stabilize the trunk.  The hips are inherently stable and facilitate the overall health of the lumbar spine. When rehabbing the lumbar spine, we must focus on hip mobility, strength, and retraining functional movements. In my therapy sessions, I start retraining the gluteals with basic table exercises such as bridges and clamshells. When pain decreases, I advance to quadruped exercises, standing hip extensions with TrA activation, and dynamic single leg balance activities. Regarding function, I start retraining the hip hinge technique as well as squat and lunge patterns. We must check the hips on every lumbar evaluation! -Jim
This case is coming from treating one of my co-workers yet again, although it is a different one from last week's post. A few weeks ago, one of my co-workers came to me with complaints of a "squeezing tightness" with CKC flexion of his R knee. I was pretty busy at the time treating my patients, but I have treated this co-worker a few times with repeated motions and, due to his excellent compliance, I knew he would likely respond well to repeated motions. My co-worker told me he had a history of knee problems from several years ago when he was in the military and thinks those issues may have been contributing to his current symptoms. His asterisk sign was a lateral lunge. On his L side he had no issues and displayed good depth. On his R side, he had significant loss of depth and reports of intense "squeezing" the deeper he lunged. As always, I checked the lumbar spine first which displayed relatively good lumbar flexion and extension mobility but a slight loss of sideglide motion, loading the involved side. This was the same side I had previously given him sideglides to and he told me he has kept up with them, but hadn't noticed any changes in his quadriceps symptoms. I continued my assessment and noticed a loss of hip flexion mobility on the R side. I had hip then perform repeated hip flexion and reassess the lateral lunge, with reports of improved depth and less tightness. About a week later, my co-worker told me he didn't notice any significant symptoms remaining at all. I thought this case was worth bringing up for a couple reasons. One, as always, compliance plays a significant role with treatment. My co-workers, knowing the benefits of being consistent, are more than compliant with the 10 reps/hour prescription and, thus, typically get better extremely quickly. Second, don't let "weird" symptoms confuse you. Neural symptoms can be reported in many different ways but remember to always stick with your system of looking at mobility in each joint and treat accordingly. Finally, while most cases like this will respond well to lumbar treatment, you will have instances where other joints are limited and their treatment are essential to improving your patient's primary complaint. -Chris
Like this post? Then check out the Insider Access Page for advanced content! And check out similar posts below!
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|

















 RSS Feed
RSS Feed