- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
One of the foundations in our residency and fellowship training and a component of our courses is Sahrmann's Movement Impairment Syndromes (MIS). While it has its faults, the system can be incredibly effective in identifying and categorizing abnormal movement patterns. When reading the text, it becomes apparent that the concept isn't all that unique; however, the system connects clinical reasoning pathways in a very easy to understand way. Recently, I had two patients come in with presentations of thigh and knee pain that I initially diagnosed with meniscus tear with sciatic nerve adverse neural tissue tension (ANTT). While this diagnosis may be correct in some circles, our current understanding on the lack of correlation between tissue injury and pain means there can be many different methods of diagnosis and treatment. Under Sahrmann's MIS, I would classify the patients' presentations as Hip Extension with Knee Extension Syndrome. While the diagnosis is targeted towards the hip, the presentation can include posterior thigh pain (similar to sciatic nerve ANTT). I thought it would be an interesting presentation to review. With Hip Extension with Knee Extension Syndrome, pain may present at either the ischial tuberosity or along the hamstring muscle belly. Pain may be present with moving from sitting to standing, walking, sitting, and negotiating stairs. The primary issue that develops with this condition is overuse of the hamstring muscle. Due to weakness in the quads and/or glutes, the hamstring muscle becomes the primary hip and knee extender. The hamstrings very obviously can extend the hip, but they can also extend the knee if the foot is fixed. Movement Impairments and Examination: When the patient gets up from a chair or goes up the stairs, it appears as if the knee moves backwards to pull the body up as opposed to the body leaning forward and using the glutes/quads to extend the hip and knee. You may also see the hip extend during a long arc quad and the glute won't displays any contour changes during prone hip extension until the end of the motion. Additionally, the knee is typically held in hyperextension (and possibly hip internal rotation) in standing, which typically is a swayback posture. In testing, the hamstring is tender, tight, and painful with contraction. Typically the glutes and lateral rotators are weak (the quads may or may not test weak with MMT). Hip flexion may be stiff due to hypertonicity in the hamstrings. Slump test may be negative, but may be positive with presence of >1 condition. Treatment: Overall, the goal is to strengthen the glutes, hip lateral rotators, and quads, while simultaneously decreasing overactivity in the hamstrings. This includes avoiding hyperextension of the hip and knee and encouraging glute contraction during gait, stairs, and transfers. Exercises that are encouraged include (for more detail on each one, check out the Sahrmann textbook on MIS or check out the Management of the Hip Course): -Quad Rock Back -Heel Slide without Rotation -Straight Leg Raise -Prone Hip Extension with Glutes -Prone Bilat Hip LR Isometric -S/L Hip Abd with LR -Seated LAQ without Rotation -Sit to Stand with Glutes/Quads -SLS/Step-Ups with Glutes For more information on evaluation and treating hip conditions like these, be sure to check out the brand new course by TSPT, Management of the Hip, an in-depth lecture series on Anatomy & Biomechanics, Differential Diagnosis, Examination, Treatment, and more! Below is a trailer of what's offered in the course. -Dr. Chris Fox, PT, DPT, OCS
3 Comments
When you hear overhead athlete what do you think about? Do you think baseball or tennis player? Do you think about the weightlifter? Crossfitter? What about basketball? You see, there is many different types of overhead athletes. Yet, preparing these athletes can be both entirely different and also very similar. Many don’t consider basketball an overhead sport but next time you watch a basketball game take a closer look at the players blocking, dunking, and rising up for a shot. It is indeed an overhead sport. Furthermore, one of the greatest players to ever play the game, Kobe Bryant, underwent rotator cuff surgery late in his career. Again, just more evidence that the game of basketball is an overhead sport. So, what is it about the overhead athlete that is unique? Well, other than the lack of return to sport tests for the upper extremity, gaining end range stability is absolutely crucial for preparing them for their sport. Later in this article I am going to show you some of my favorite end range shoulder stability drills that I’ve had success with. These are drills that can be used across all of the athletes mentioned above (within your clinical reasoning framework of course). First, let’s talk about screening the overhead athlete. This step cannot be overlooked as this is the cornerstone to determine what our overhead athlete needs. For those of your who are also strength coaches, this is part of our “Needs Analysis” phase. There are a few must have screens for this part. The standing shoulder flexion screen gives us an overall first look at movement quality. Does the athlete have full range of motion? Is it smooth? Does the athlete substitute with the lumbar spine or forward neck? Is their rib flare? Pain? From here we can break down the motion in supine with a lat screen if the movement is limited. See the video below for an explanation on this. We can also look at subscapularis and pec minor tone and mobility here. Once we’ve established a baseline of movement quality and possible restrictions there are a few key muscles to look at testing. While I hate MMT’s, they serve a purpose at times. Looking at serratus anterior strength is one I often look at with this population. I will also look at middle trap, low trap, and RTC strength. Again, without some type of assessment it does not matter how “good” of an exercise it is or how “cool” it looks. There’s a lot of great exercises out there but they might not be appropriate for YOUR athlete. Assess, don’t guess. Now for the fun part. Once you’ve worked on ROM and basic strengthening you will want to start working on end range stability. I often see this phase botched and it’s a disservice to our overhead athletes because ultimately, we do have to load them to prepare the tissues and shoulder for more intense activity and their sport/positional demands. See below for a short list of exercises I use. For the complete list and progressions/regressions check out my full videos on our Insider Access page. My favorite OH exercises
In physical therapy school, therapists are taught a broad spectrum of knowledge. Orthopedic examination, treatment, and prognosis is covered in-depth. For example, we learn more than 50 special tests to diagnose shoulder impingement, rotator cuff dysfunction, biceps pathology, and labral tears. Despite all this knowledge, therapists lack the ability to prioritize these tests. Many therapists gather information without considering ‘why’ we perform each measure. We soon realize that the special tests are not very special! Upon finishing their clinical examination, they are drowning in information that only minimally changes their patient’s prognosis or intervention selection. The therapist has found several secondary and tertiary impairments without identifying the primary cause of the problem. In this post, I am going to discuss how I perform a shoulder evaluation and review some of my regular day 1 shoulder exercises. Shoulder Examination: Efficiency and Reliability
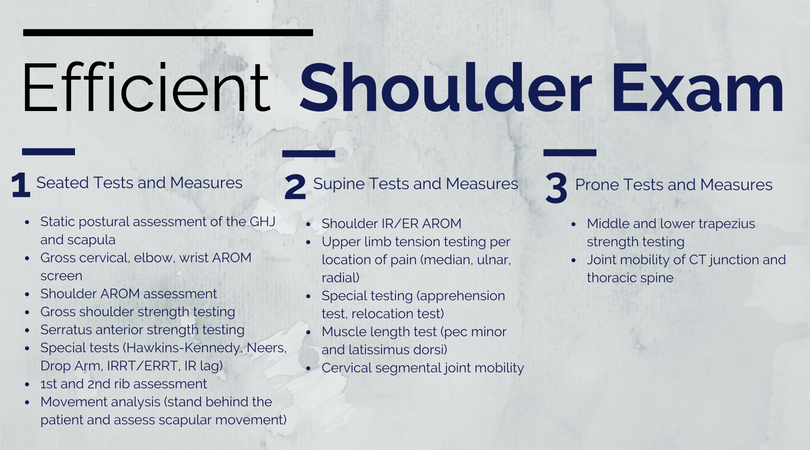
Understanding the biomechanics can be a great starting point for assessing a painful region of the body. A lack of mobility or stability in any local region can impact one's pain perception, altering their response to stimuli. For new clinicians, it is important to develop an efficient and reliable examination. This combination of efficiency and reliability will minimize any redundancy of testing while maximizing time for treatment. Below is my template for performing an efficient examination. For the purpose of efficiency, it is divided by patient position. You will notice that only a few special tests are performed and the biggest focus is on assessing regional joint mobility.
Shoulder Interventions: Day 1 Treatment and More Upon completion of the shoulder examination, the next step is selecting appropriate interventions. From my clinical experiences, the shoulder joint is typically irritable in the acute stages. Therefore your exercise selection and manual interventions should address the patient's pain. My Day 1 interventions heavily focus on desensitizing the painful tissue through graded tissue exposure. Additionally, I spend a significant amount of time discussing the different mechanisms that impact pain. These exercises often include range of motion exercises and posterior shoulder muscle activation. If the patient has low irritability, further strengthening and mobility exercises can be initiated early in the plan of care. The video below discusses 3 common exercises I give to patients on the first day. If you find this video useful, I encourage you to check out our Insider Access pages. Questions or comments?
Let us know what initial interventions you typically use when working with shoulder patients! -Jim Heafner PT, DPT, OCS |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|











 RSS Feed
RSS Feed