- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 The Student Physical Therapist was again nominated for the "best student blog" on Therapydia.com. Please show us your continued support by voting for us in this year's blog awards.
0 Comments
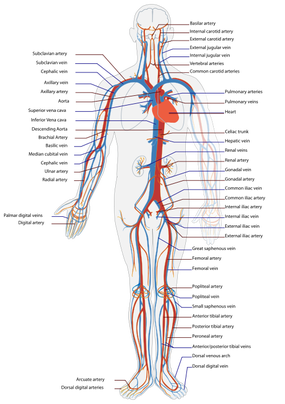
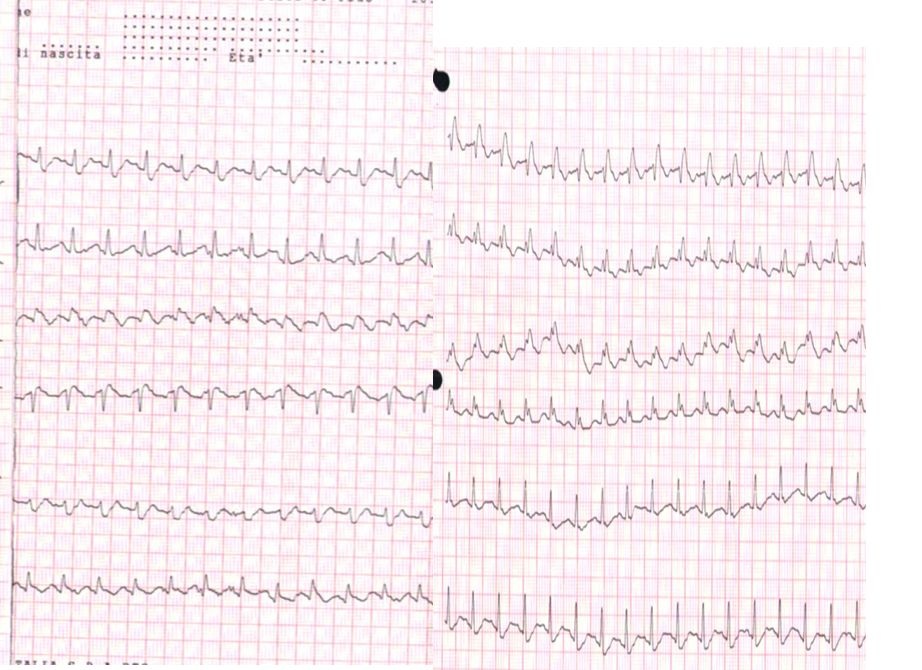
Expected ECG Findings
The easiest way to explain the heart rhythm is to refer back to an electrocardiogram (ECG - as depicted below). For review, we will go over the basics of an ECG first: -P Wave: depolarization of atria (starting at the SA node, then spreading out to the atria) -PR Interval: time it takes for the electrical pulse to get from the SA node to the AV node) -QRS Complex: depolarization of ventricles (starting at the AV node; re-polarization of atria hidden here) -T Wave: re-polarization of ventricles This patient in particular, as you recall, had 3 pulses followed by a pause. This likely signifies a Second Degree AV Block: Mobitz Type I (Wenckebach). This would be depicted at a slowly increasing PR interval, before a lack of QRS complex occurs. The cycle then restarts. Basically this means the signal from the SA node to the AV node slows until it doesn't make it through to initiate ventricular contraction, before the next SA node initiates again to restart the cycle. If you've ever struggled with interpretting ECG's, I recommend reading this book by Dale Dubin. It provides a step-by-step understanding and asssessment of ECG's along with the associated pathologies, at an MD level. It is an excellent source for reviewing for a CardioPulm course or preparing for the Cardiovascular section of the boards! -Chris  As former students and current alumni of Saint Louis University's Physical Therapy program, we would like to congratulate SLU on the launch of their orthopedic residency program! SLU has partnered with SSM Physical Therapy to give the the residents a unique experience of spending time at both SSM and Saint Louis University. They have put together a phenomenal faculty and diverse curriculum for a structured learning year. We would encourage anyone who is interested in an orthopedic residency to look into SLU's program and contact their residency director: Chris Sebelski, PT, DPT, OCS.  Pain science is becoming a more important aspect of physical therapy training. Many schools are not dedicating enough time to understanding how and why pain operates and persists. Fortunately, there is a wealth of resources on the internet to help supplement what is being taught in physical therapy education. On the TSPT blog, we have discussed this topic several times. (Here and Here). Recently, I stumbled upon this video produced by Brett Peterson, MPT, OCS, FiT on the PT Coop website. His video outlines: a) A brief history of the past and current pain theories b) Psychological components of pain c) Perception and the relationship to pain d) Treatment options for physical therapists 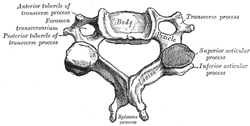 Individuals with mechanical neck pain often have pain and a loss of mobility in the upper cervical spine, specifically at the atlanto-axial (C1-C2) joint. This joint is primarily responsible for cervical rotation, but also contributes to small amounts of flexion and extension. Arthrokinematically, during left rotation, the left facet of the atlas(C1) glides posterior on the axis (C2) & the right facet of the atlas glides anterior. During flexion, the facet of the atlas glides anterior and rolls posterior in relation to the axis. The opposite happens with extension. There are 2 different theories as to how to assess the mobility of C1-C2. At Harris Health, I learned to maximally side bend the head, followed by opposite rotation. For example to assess C1-C2 rotation to the left, maximally side bend the head to the right, followed by maximal rotation to the left. The maximal side bend "locks out" the lower cervical vertebrae allowing for motion only at the C1-C2 junction. The other method to assess C1-C2, which I learned in PT school at St. Louis University, is the flexion- rotation test. To perform this test, maximally flex the cervical spine followed by maximal rotation either left or right. Flexion is thought to lock out all vertebrae below allowing for rotation at C1-C2 only. The difficulty with the flexion-rotation test is maintaining flexion while maximally rotating the upper cervical spine. From my experience, there is a tendency to lose upper cervical flexion. In the residency, I learned that the flexion-rotation test assesses C1-C3. One can then differenciate C1-C2 restrictions from C2-C3 restrictions by first performing the side bend rotation test first, then performing the flexion rotation test. If greater rotation is achieved during the flexion-rotation test vs. the sidebend then rotation, it can be assumed the dysfunction is greater at C1-C2 joint.
It is important to understand that different programs teach different methods of assessment. One method is not better than the next as long as there is sound reasoning behind your decision making. Does anyone else assess C1-C2 differently or have preference with one method over the other? Let us know! -Jim Thank you to the Harris Health Orthopedic Residency for letting me use images from their Cervicothoracic Module Workbook. 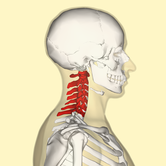 Last Tuesday I performed an evaluation on a traumatic C7 Disc Herniation. The 29 year old male presented with neck pain, medial scapular pain, and decreased function of the triceps muscle. This is the first traumatic cervical disc herniation patient I have treated and I thought I would do some research on the topic prior to his 2nd visit. It should be noted that traumatic is different from degenerative disc herniations, a component of DDD, which are present in "30-70% of all adults...as seen on Magnetic Resonance Imaging." As many people know, traumatic cervical disc herniations are seen much less frequently than lumbar disc herniations. This is primarily due to less load bearing requirements of the C-spine, but also in part due to the physiological construct of the cervical disc. The annulus fibrosis, outer ring of the disc, is discontinuous and "does not have complete concentric rings that surround the nucleus." (Neumann 2010) Cervical discs herniate either posterior or posterolateral. They do not typically herniate purely lateral due the uncinate processes blocking this motion. When the disc herniates, it may result in compression of the spinal cord or "radiculopathy, marked by compression and inflammation of the cervical nerve root." With a posterolateral herniation, symptoms include either sharp or dull pain down the medial border of the scapula with radicular symptoms present in a dermatomal pattern of the suspected nerve root. In certain cases, "numbness or tingling may also replace pain as the primary presentation." (Yeung 2012) A physical examination can guide you to a diagnosis, but the best diagnostic test to confirm a disc herniation is a MRI. Treatment of cervical disc herniations is a multimodal approach. Currently there is not a great deal of research regarding treatment options. I plan to treat this individual similar to a cervical radiculopathy patient. I will be using a cervical unloading device while performing active strengthening exercises and the appropriate manual therapy techniques. Additionally, I will be address scapular strength, nerve tension, and postural deficits that were found during the evaluation. More to come, -Jim References: Neumann, Donald A. Kinesiology of the Musculoskeletal System: Foundations for Physical Rehabilitation. St. Louis: Mosby, 2010. Print.
Yeung, Jacky T., John I. Johnson, and Aftab S. Karim. "Cervical Disc Herniation Presenting with Neck Pain and Contralateral Symptoms: A Case Report." Journal of Medical Case Reports 6.1 (2012): 166. Web.  I once had a teacher tell me, "A physical therapist is only as good as his/her home exercise program." At the time I did not fully understand the scope of this statement. Of course a home exercise program (HEP) is an essential component of physical therapy, but the really important aspects are completed in the clinic...or so I thought. Once I complete each initial evaluation, I start educating my patients on their HEP by giving them a frame of reference. I discuss how little time each week is spend with the physical therapist. If they come in 2 times a week for 45 minutes, they would not even be with me for 1% of the week. Getting better is a commitment that should require them to think about their HEP daily. Prescribing the correct exercises is another factor the must be considered of course. We want to combine the primary impairments found during the examination with results from any manual therapy to determine which exercises are most critical. While the patient is responsible for being committed to performing the HEP, it may be unrealistic to expect every patient to perform every exercise that we would prefer as clinicians, often leading to a selection of the most key exercises. I recently read a post from The Manual Therapist about the 5 articles that most significantly impact his practice (I highly recommend reviewing it). Several of the articles covered really had an impact on me regarding my understanding as to what my manual therapy techniques actually are and are not accomplishing. One of the articles is a basis for the differing views regarding Instrument Assisted Soft Tissue Mobilization (IASTM). IASTM techniques such as Graston and ASTYM preach the effect collagen remodeling, while other perspectives view it as a neurophysiological effect. One study showed that it requires over 100# of force to remodel fascia by 1% (Chaudhry et al, 2008). Why is it we spend so much time on soft tissue techniques and see results? Schleip did an extensive review on the fascial systems. He reminds the reader of the high number of mechanoreceptors located in the skin and other soft tissues. Different parts of the body are intricately connected via this fascial system, suggesting treatment of one location may impact another. When stimulated via our techniques such as soft tissue massage, trigger point release, foam rolling, etc., we are in fact encouraging the receptors to alter the sympathetic nervous system and alter tone in the muscle and fascia, which can be portrayed as a "release" in soft tissue restrictions. This leads us to believe that many of our manual therapy techniques achieve their results due to a neurological effect. To get mechanical changes, we would need high levels of force for prolonged periods (this may not apply to manipulations - high velocity low amplitude thrusts). If the fascia were as easy to deform as some think with manual therapy techniques, actions such as running, jumping, or even sitting provide larger forces than we are providing with our hands on our patients. Another study looked at spinal mobilizations/manipulations and their effect on various outcomes. Manual therapy techniques like these have been shown to have effects on the sympathetic nervous system via the dorsal peri-aqueductal matter of the midbrain (Hegedus et al, 2011). The study also found that these neurophysiological effects only last typically 5 minutes. They pain-modifying results lasted up to 24 hours. So what does all this mean? If we want any lasting changes, it is imperative we distribute a HEP that encourages movement in these gained patterns and establish the necessary changes in posture, habits, work space, etc. needed to reinforce proper tissue mobility and stability. It means our manual therapy techniques can be effective, but maybe not due to the reasons we previously thought. We can instill immediate or near-immediate changes with any manual therapy skills we have but they may not last more than anywhere from 5 minutes to 24 hours. To put it simply, manual therapy is not enough. Without an effective home exercise program, we would be likely to see our patients returning week after week with little retention of the gains we had achieved during prior treatment sessions. -Chris References:
Chaudhry H, Schleip R, Ji Z, Bukiet B, Maney M, & Findley T. (2008). Three-Dimensional Mathematical Model for Deformation of Human Fasciae in Manual Therapy. Journal of the American Osteopathic Association. 2008;108(8):379-390. Web. 5 April 2014. Hegedus EJ, Goode A, Butler RJ, Slaven E. (2011). The neurophysiological effects of a single session of spinal joint mobilization: does the effect last? J Man Manip Ther. 2011 Aug;19(3):143-51. Web. 5 April 2014. Schleip R. (2003). Fascial Plasticity - A New Neurobiological Explanation. Journal of Bodywork and Movement Therapies. 2003;7(1-2):1-22. Web. 6 April 2014.  Next Tuesday I will presenting a Journal Club on the different manual physical therapy "cults" that exist in our practice. I did not choose the word "cult" nor do I think that this term is appropriate. "Cult" has a negative, even evil connotation, that makes the cult-ee seem close-minded and against all other practices. A simpler, more optimistic word may be "brand,"(which manual therapy brand is one associated with) but for the sake of today's writing, I will stick with cult. When discussing different manual cults, I think it is important to look back into the beginnings of this name game in PT practice. In a 1996 Physical Therapy Journal editorial entitled, "Be not content to Sleep and Feed," author James Holmes defends the "cult" of manual therapy against therapeutic exercise and passive modalities for the treatment of low back pain. Around this time, there was much controversy regarding the proper management of low back pain patients. Many patients were not improving with therapeutic exercise and the use of passive modalities. In response, some therapists turned to manual therapy. At this time, there was limited evidence toward the efficacy of manual therapy treatments. This change in practice did not go unforeseen. The traditional therapists started classifying manual therapy as a cult. In the editorial he writes: "reconsider chastising manual therapists as cultists...our methods await research validation...and our patients are better served as a result of the emergence of manual therapy." Holmes was right in defending manual therapy, but what is more interesting is that manual therapy in itself was viewed as a cult. Now each branch of manual therapy is its own cult: Maitland, Kaltenborn, Active Release Technique, IASTM, etc. As human beings, we have tendency to classify ourselves based on our training. The question one needs to ask, "is it bad to be identified with a certain brand of manual therapy?" I do not think so as long as I am not solely utilizing that one system. Each "cult" has its unique positives and negatives, but the truth is that our research is not strong enough to place a patient in only 1 cult. Be open-minded and ready for change. Humans are too unique and individual to place all of one's training into 1 type of practice. It is best to have an eclectic approach, where we consider evaluation and assessment techniques from various schools of though. -Jim Reference:
Holmes, James A (1996). Be Not Content to Sleep and Feed. Physical Therapy Journal. 76(6), 664-666. doi: 31 Mar 2014. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|








 RSS Feed
RSS Feed