- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
Proper shoulder function is all about proper starting posture. Many of our patients start from a poor position, and therefore have pain with overhead movements. For example, many patients rest is scapular downward rotation. This position places the rhomboids in a short, dominant position. In the same example, the serratus anterior and lower trapezius (both upward rotators) are lengthening and relatively inhibited. If we can neutralize scapulothoracic mechanics, chances of pain free overhead movement will increase. In this post, I break down Eric Cressey's video on Cues to Improve Shoulder Flexion. Eric Cressey's 3 Cues: 1) Assess for an adducted/downward rotated posture. This patient is not appropriately activating their upward rotators. With these individuals cue them to make a bigger arc of motion as they are raising overhead. The bigger arc will allow for more scapular upward rotation. 2) Assess for anterior tilt and a prominent inferior angle of the scapula. With this cue, manually assist the patient into posterior tilt as they are raising their arm overhead. The practitioner will be mimicking the function of the lower trap and serratus by posteriorly tilting the scapula. 3) Assess for scapular depression and Lat Dorsi dominance. Due to their resting posture (clinically interpreted as downsloping shoulders), these patients often have lengthened upper trapezius muscles. Start in a neutral scapular posture. Have the patient raise overhead. When the subject gets to about 90 degrees of shoulder flexion have them perform a small shoulder shrug. This will help engage the upper trapezius and allow for better clearance of the humerus under the acromion. -Jim Like this post? Check out more videos similar to this on our Insider Access page!  Want to learn from Chris Fox and Jim Heafner in person? Join our COMT program starting this October 2015. Click here to learn more!
0 Comments
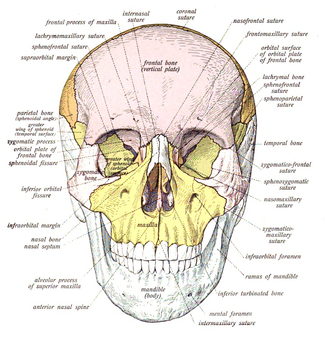
The Manual Therapist recently posted about different methods to address patients' perceptions on imaging. He calls them "thought viruses." As I've said before, one of the most frustrating things during an evaluation for me is when a patient can recite their imaging findings. It's not their fault. Often, multiple doctors and other health care practitioners have used a combination of the imaging findings, pain location, and biomechanical model to explain why the patient is having pain. With doctors' level of respect and how the biomechanical model "makes sense," it's no surprise that patients grab onto these explanations. Some of the things discussed in the article include the fact that degenerative changes almost always present in an asymptomatic population and that with intermittent pain, how the spine looks in an MRI doesn't change. Patients are often focused on the structural aspects and words such as "pressing," "pinching," or " crunching" have been shown to increase level of fear and pain in the brain by themselves. As a profession, we should stop reinforcing these outdated theories that may potentially even be harmful for our patients. Check out Dr. E's post for more in-depth discussion! -Chris Like this post? For more advanced information, join the Insider Access Page now! Also, check out similar previous posts below:
Performing a thorough, but concise subjective history is essential prior to performing your physical examination. Each question that is asked should guide you to a follow-up question. These answers should then correlate with the physical exam measures you choose to perform. For example, if a patient states she fell on her left buttock and her symptoms are aggravated by forward bending, you absolutely need to check her cardinal plane flexion and sacral mobility. Always correlate a specific aggravating factor to a measureable functional movement. A good format to follow: 1) Have the patient describe what their problem is in their own words. Is the patient having pain, numbness and tingling, weakness? Don't assume every patient has pain. Listen to how their describe their symptoms. 2) When did their symptoms start? Asking when the symptoms began allows you to determine if the symptoms are traumatic or insidious in nature. Additionally, this question can help you determine what structure may be involved. For example, a traumatic knee injury may guide you toward ligament insufficiency versus knee pain of insidious onset may lead you to think patellofemoral pain. 3) How has the pain changed since onset? Has the pain changed in quality, progressed, or gotten better? Do the symptoms have a specific pattern throughout a 24 hour period? 4) Can the patient describe aggravating and alleviating factors? Make sure there are alleviating positions or activities. 5) What is the nature of the pain? Is is constant or intermittent, sharp or dull, stabbing, throbbing, and/or aching? 6) Any significant past medical history? If a patient comes into clinic with L shoulder pain, but also has a history of cardiovascular disease, you need to ask some follow up questions. Always inquire about PMH! 7) Has the patient every injured this region before? This includes past surgical history to the area. 8) Is the patient having pain anywhere else in the body? In PT school, one learns to check the joint above and below. I challenge you to check all joints that may be associated with the area of dysfunction! Often times a patient will forget to tell you about a calf pain when they are having low back pain OR a wrist pain when they are having shoulder symptoms. Sometimes you need to assess more than 1 joint away from the primary pain. Remember: A good clinician should obtain 85-90% of their information from the subjective history and initial interview. What other questions do you ask during the initial interview? Jim Like this post? Check out more exclusive information on our Insider Access Page.   One of the frustrating things for new grads to learn after coming out of school is that we do not get 100% of our patients 100% better. Part of the reason is that with physical therapy moving towards direct access, not all patients have a true neuromuscular problem. Patients with other pathologies come into our clinics as well. Probably one of the biggest issues, however, is patient compliance. We all know the home exercise program is an essential component of any patient's rehabilitation. We also know that patients more often than not fail to comply with the prescription. A patient's adherence to their HEP allows therapists to progress or adjust patients' treatment plans more accurately. That is why it is essential we educate our patients on the importance of following the instructions. For example, with a repeated motions HEP, the exercise is not only used for treatment, but also diagnosis. Based on how a patient responds, sometimes the motion has to be altered. Even with all that being said, some patients will still not be compliant. They will come in after you gave them homework regarding exercises to do, necessary liftestyle changes and more, yet, still have significant pain. Upon questioning, you may discover the patient did follow the instructions, whether it be the required frequency or postural changes. Unfortunately, some people will not set completing their exercises as a higher priority. They are in pain, but still have trouble making time for the adjustments. It is frustrating as PT's, but we cannot lose hope. I recommend further education for the patient as a start. The key is making the "light switch on" for the patient. What I like to do is have the patient complete a painful activity, then perform their repeated motions to decrease their pain and then re-test the original activity. Sometimes it then clicks for the patient that they can manage their symptoms. Sometimes, the patient still will not make the necessary changes. We must do our best to help the patient make the commitment to the program. -Chris Like this post? For more advanced information, join the Insider Access Page now! Also, check out similar previous posts below:
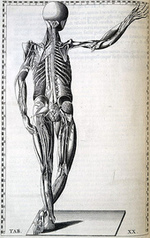
 Recently we have been receiving several questions regarding continuing education credentials. What does it mean to have a COMT, OCS, FAAOMPT, etc... In this post I am going to break down the difference among several commonly seen advanced certifications. Orthopedic Clinical Specialty (OCS): Any "CS" credential means the clinician has earned a clinical specialty. For example, Chris and I recently passed our OCS examination so we are now Orthopedic Clinical Specialists. Brian passed his SCS so he is a Sports Clinical Specialist. You are eligible to sit for your Clinical Specialty Examination in one of two ways: 1. attend a residency program OR 2. demonstrate 2,000 hours of clinical work in the specialty area plus a few other criteria. (For more information follow the link HERE) The three of us chose to do the residency program. It is a quicker route to becoming a clinical specialist and a residency program gives you at least 150+ one-on-one mentoring hours. I would highly recommend this option to anyone who is looking to improve their clinical skills. Certification in Orthopedic Manual Therapy (COMT): Many clinicians choose to pursue a COMT prior to their fellowship in manual therapy training. Many programs follow a 1-year curriculum consisting of five or more weekend learning courses. For example, Chris and I recently partnered with OPTIM Physical Therapy to start a COMT program. Our program consists of 6 weekend courses with online didactic course work in between sessions. Each program has a different focus, but the ultimate goal is to become in expert in neuromuscular examination and manual therapy techniques. (To learn more about our program click HERE. Fellowship of the American Academy of Orthopedic Manual Therapy (FAAOMPT): If you are officially seeking alphabet soup behind your name, pursue the FAAOMPT credentials. It is one year of training, plus 440 one-on-one mentoring hours. To enter into a manual therapy fellowship, one must first either go through a pre-fellowship year or residency program. In this post, I am writing about manual therapy fellowships, but remember that there are fellowship programs across multiple specialty areas. Click the link HERE to learn more about fellowship programs. So which speciality certification should you pursue? There is no perfect answer, but at least having awareness of the different options is a step in the right direction. My recommendation: look at the residency corner posts that we have made on this website and check different programs websites to gain a better understanding of which fits best with your current practice and lifestyle. Jim Like this post? Check out or insider access page to unlock even more information.  OCS Preparation As with any exam, it's important to be aware of the type of material that you will be tested on along with the method of questioning. From my discussion with physical therapists that have passed the OCS and after reviewing the goal of OCS certification, it appears that a major component involves "evidence-based practice" applied to many case scenarios. Continue Reading... I attended a lecture once where the idea of a muscle being "short" for benefit was discussed. The instructor commented that we should be hesitant to try and "stretch" the hip flexors of speed skaters as this adaptive shortening allows the muscle to be more effective in the required range for the activity. Due to the standards set for the Thomas Test and systems like the Selective Functional Movement Assessment (SFMA), I thought this would make an interesting topic for discussion. Now I should make a distinction between two commonly confused items: relative stiffness and adaptive shortening. Relative stiffness stems from the idea of a direction of susceptible movement between two joints. For example when you are bending forward, even though both the hip and spine can provide motion to achieve the act, a greater amount of stiffness in one will allow the majority of motion to come from the other. Sahrmann refers to a spring example where two springs are attached to one another with different tension points (as depicted below). When you spread the springs apart, the majority of motion will come through the spring with less tension. On the other hand, true adaptive shortening occurs when the actual muscle length has been shortened, i.e. contracture. For the purpose of this discussion, both adaptive shortening and relative stiffness will be included in the argument and referred to interchangeably. How do these muscles develop increased stiffness/shortening? The answer lies in both repetitive activity and prolonged positioning. Going back to our skating example, the athlete is in a flexed position with the requirement of highly forceful and repetitive action of both the hip flexors and extensors, the former acting in a shortened position and the latter in a lengthened position. The hip flexors become especially effective in that shortened position. This activity in the shortened position increases the overall stiffness of the muscle which can lead to increased mobility requirements (as a result of less stiffness relatively) in the spine. Similarly, we, as a general population, spend an excessive amount of time sitting, which is a flexed position of the hip. Now I likely test for flexibility differently than most, as I have rarely ever seen a "negative" Thomas Test. When I complete the test, I feel for any movement at all of the ASIS before the femur reaches the final position. If movement occurs, I consider the test positive as the direction of susceptible motion is lumbar extension during the test. Getting back to the primary issue, likely at least part of the reason I so regularly see positive Thomas Tests is due to how much our population sits. That's a lot of time in the shortened position! The question about whether or not we should ignore the impairment has not been addressed and that is partially due toe the lack of a definitive answer. Personally, I think the impairment needs to be addressed. Having been trained in the aspects of the SFMA, there is a normal amount of motion that should occur from each joint during certain movements. Imbalances are what can lead to injury. Our goal should be to help bring balance back to the body. With our hip flexor stiffness from prolonged sitting, we can relate to the amount of low back pain associated with prolonged sitting. This can be easily treated with something such as repeated extensions in order to help restore the "balance" between flexion and extension in the nervous system. However, the argument can be made that were we to do this with the skater, the hip flexors wouldn't be as effective in that shortened position. Again, in my opinion, overall the athlete/client will be much more successful having the normal mobility throughout, leading to less risk of injury. What are your thoughts? Are there clients we should permit potentially beneficial adaptations to persist? -Chris Like this post? For more advanced information, join the Insider Access Page now! Also, check out similar previous posts below:
I have been listening to Kelly Starrett's principles on mobility for several years now. Recently he recorded a question and answer podcast with Tim Ferriss on important tips regarding training, mobility, and movement throughout our daily lives. Some of the key principles from the podcast: 1) Humans should be able to complete basic movements from the moment we get out of bed. We should have normal range of motion in our joints prior to the warm-up. If someone has to warm-up to achieve the necessary range of motion to do a pull-up, they are at risk for injury. We need to be able to perform the range of motion innately, the warm-up should be used perfecting the movement and priming the muscles for harder movements. 2) Creating a "12 minute mobility WOD" for everyone would not be a good strategy for eliminating injury. Each person has unique mobility deficits and compensations. We need to be creative with our daily mobility exercises to keep the body flexible is multiple ranges. There is no mobility recipe for everyone. 3) Addressing the mobility alone is not sufficient, we need to change the underlying movement dysfunction. 4) Breathing, nutrition, and following a proper sleeping schedule are vital for healthy movement. 5) Sitting and prolonged positions are causing many of our problems. We need to be in a movement rich environment. Check out the full podcast here Like this post...Check out more great information on our Insider Access Page!  Sitting Wrecks Your Hips The problem with sitting exists beyond the chair as well. Normal standing posture requires little muscular action to maintain an upright position. In the presence of a hip flexor contracture due to prolonged sitting, forces are placed anteriorly across the hip requiring the hip extensors to counteract the force. Increased muscular action and metabolic cost creates the desire to sit, perpetuating the circumstance which initiated the hip flexion contracture (Neumann 2010). Continue Reading With the push for evidence-based practice, there is an increasing disregard for less common evaluation and treatment methods, such as craniosacral and visceral manipulation. Part of that may be due to the difficulty to formulate a quality and standardizd study using these theories. Personally, after PT school I thought the techniques were similar to the practice of witch doctors. My mind was set in a purely biomechanical perspective. Recently, I spoke with someone who had intense pelvic and abdominal pain after surgery that had her pain eliminated with visceral manipulation. I've heard of similar presentations after gall bladder removal, appendectomy and more. While I am still uncertain of the true mechanism, I have definitely become more open to the atypical approaches. With the development of pain science, we understand how crucial a role the mind plays in our patient's pain levels and treatment. Simply put, if a patient thinks a treatment will work, it will work. There was a time when I thought the use of modalities was equated with out-dated physical therapy, but I have become open to its use in patients who report prior "success" with it (I, of course, educate the patient on the benefits of a more active treatment approach). Going back to a patient's beliefs, we as clinicians can play a significant role in the process. If we build trust with the patient, our explanations of why the patient is experiencing their symptoms can impact the patient's response to treatment. A patient who trusts a craniosacral therapist and their explanation may be more open to whatever changes occur with the treatment. Same rule applies for all treatments. While it is not so simple as to give an explanation to the patient then treat according to that theory, these factors may at least influence our patients. The most difficult aspect occurs when patients have had many various explanations for their pain in the past or were convinced in the past about the source of their issues. My most difficult patients to treat are the ones who memorize their MRI findings. Educating them on how insignificant those findings are can almost completely eliminate any trust that was there in the first place. In conclusion, as a profession, we shouldn't be so quick to eliminate anything that isn't supported by higher levels of evidence. Things like craniosacral therapy and visceral manipulation have been around as long as they have because there is some sort of success. Maybe part of the success is due to a particular subset of the population being more open to the concept and maybe not. Regardless, we should be open to any form of treatment that may benefit our patients, thus increasing the importance of developing an eclectic approach. -Chris Like this post? For more advanced information, join the Insider Access Page now! Also, check out similar previous posts below:
Working in occupational medicine, I see many middle aged patients with knee pain. Often times these individuals have a history of knee symptoms with a recent flare up of their symptoms due to a recent injury. MRI evidence of these patient will likely show meniscal or chondral pathology consistent with degeneration. In other words, these patients have early arthritis. What is the best treatment course- surgery or conservative management? A recent systematic review was published on the benefits and harms of arthroscopic surgery for degenerative knees. The review found that the small benefit associated with arthroscopic surgery does not outweigh the benefits seen from 'exercise therapy.' Some of the harmful effects of surgery include DVT, pulmonary embolism, venous thromboembolism, infection, or even death. Current findings do not "support the practice of arthroscopic surgery as treatment for middle aged or older patients with or without signs of arthritis." How does this affect our practice? We need to educate our patients on the benefits of conservative management with degenerative knee pain. Surgery may present as a quick alternative, but the benefits do not out weight the potential risks. Educate your patients on knee osteoarthritis, exercise, and weight management. It is our duty to empower the patient to treat themselves with exercise vs. having surgery. Jim Join our Insider Access for exclusive learning from Board Certified Orthopedic & Sports Specialists!7/1/2015 Have you subscribed to our Insider Access yet?! For $4.95/month see at least three new pieces of content each month by residency trained Board Certified Sports Clinical Specialists (SCS) and Board Certified Orthopedic Specialists (OCS). Want to know what to expect? See below! Sports Specific: - Runners Evaluation: What to do when you don't have a treadmill - Return to Sport Considerations: Part 1 - Baseball Pitcher Specific Advanced Rehabilitation Exercises - Lateral Movement Progressions Part 1: Biomechanical Considerations & Keys to Implementing a Training/Rehabilitation Program - Teaching Lateral Movement - Return to Running Criteria - Return to Soccer: Non-Contact Drills & Contact Drill Criteria - The Step Down: Grading Criteria and Biomechanical Implications Upper Quarter: - 3 Methods of CT Mobs/Manips - 7 Trap & Serratus Exercises - Cervical Spine Evaluation Using Treatment Based Classification (w/ podcast) - Upper Quarter Standard Evaluation - Elbow Surgical Procedures - OA & AA Segmental Evaluations & Treatments - Rib, Elbow, Cervical Manips & More! Still not convinced? Check out any of the other sections of our Insider Access Page: SFMA Breakdowns, Hip & Knee, Low Back, Podcasts, Foot/Ankle. For a price of a cup of coffee you could be CHANGING the way you practice each month! Don't get stagnant, join our Insider Access page now! http://www.thestudentphysicaltherapist.com/insider-access.h… |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|












 RSS Feed
RSS Feed