- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
The sacroiliac joint (SIJ) is one of the more hotly debated areas in orthopaedic physical therapy. There are some who preach that it cannot move. There are some classes and theories of treatment that lay treating the SIJ as the foundation of the program. And then you have others that state we cannot possibly assess it even if it does move, so why bother. Personally, I will occasionally still assess the SIJ, however, I try to assess and treat through more general approaches, such as repeated motions, first. Occasionally, you will get a patient that is obsessed with the SIJ anatomically and pathologically. Check out this post from Dr. E at Modern Manual Therapy for some excellent advice on how to deal with these patients. -Dr. Chris Fox, PT, DPT, OCS
1 Comment
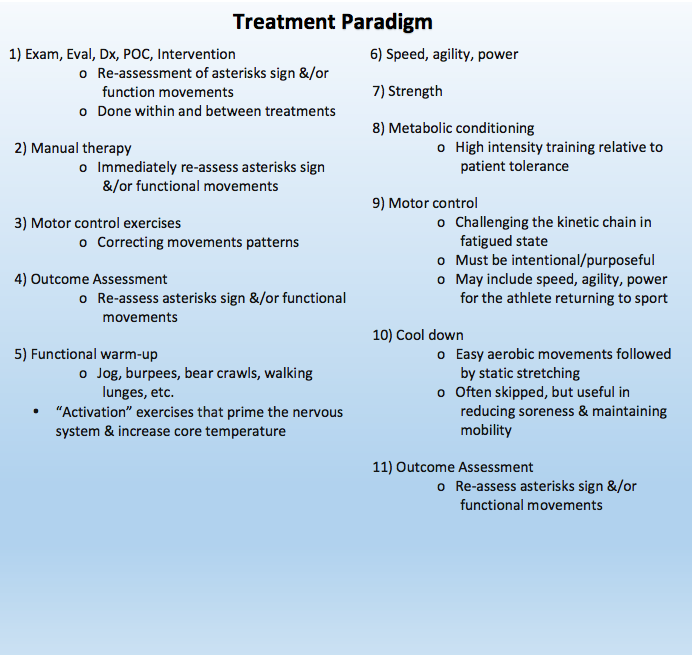
 Similar to having an efficient examination, it is important to follow a consistent treatment paradigm and flow within every session. For example, do you prioritize therapeutic exercise or manual therapy first in your treatment session? The answer is manual therapy. If you are currently squeezing your manual therapy into the end of a treatment session, STOP! The manual therapy needs to be performed early in the treatment so that changes in mobility or tissue extensibility can sustained with motor corrective exercises afterward. As seen in the treatment paradigm below, certain interventions are more appropriate during specific portions of a treatment session. First, a mini-reassessment is always warranted so that an asterisk sign (concordant sign) can be established. After identifying the asterisk sign, it is important to perform any manual therapy and corrective exercises to fix the primary impairments. Assuming the impairments have been corrected, a quick functional warm-up should prepare the patient for power and agility training next (if the patient is appropriate). It is important to perform power training before strength training and metabolic conditioning because power training is a more demanding intervention on the neurological system. Continuing with the paradigm, it is important to perform a light cool down and reassessment of the asterisk sign at the end of treatment. While certain patients may not be appropriate for all interventions during the first few sessions, the paradigm should be regarded as the ideal structure of a successful treatment session. Using this intervention structure may appear difficult at first. Be consistent and follow this process on a regular basis to instill the practice! -Jim Heafner PT, DPT, OCS The treatment paradigm was created by Dr. Dana Tew PT, DPT, OCS, FAAOMPT from the OPTIM Fellowship Efficiency is Key!OPTIM COMT and Manual Therapy Fellowship is now enrolling classes in Dallas, Houston, and Scottsdale!  Posture is a common buzzword in the health field today. It is without a doubt an important problem to discuss with our patients, especially with how much we sit. Everyone doesn't fall into the same category for posture however. It is important to categorize our patients so that we can give the correct treatment. Patients typically fall in swayback, forward head, and lumbar lordosis, among others. Furthermore, despite the postures our patients fall into, sitting tends to be the posture most need to fix. Check out this article for an easy refresher for your patients. http://blog.paleohacks.com/how-to-fix-posture/ - Brian Schwabe, PT, DPT, SCS, CSCS Board Certified Sports Clinical Specialist in Physical Therapy/Strength & Conditioning Coach/Fitness & Medical Writer Sports Physical Therapist in Los Angeles, CA  Back in July, I developed some odd neck symptoms. My throat felt swollen, like my uvula was resting on my tongue. I was unable to breathe through my nose while laying supine. Initially, I attributed the sensation to a reaction to an intense dry heat in the summer of Arizona (frequently 110-115 deg) or an allergy. I took some allergy medication for a couple weeks but noticed little change. Of course, at this point I was becoming concerned. The feeling of a lump in the throat can be associated with significant medical conditions, like thyroid disorders or cervical instability. I was disappointed that I had no change with repeated motions for my neck or back. What kept me calm is that I had no other symptoms. My lymph nodes felt normal, it didn't hurt when I swallowed and my symptoms were intermittent. I actually felt completely normal after working out or taking a hot shower, and doing some DNF strengthening exercises gave temporary relief. Given the unusual symptom and lack of other significant medical signs, I considered being treated by a visceral therapist. Fortunately, my wife does visceral manipulation, so I had her treat me sometime in August. She did a parietal-cecal ligament release, thermal scar release, cecum motility, and addressed some intestinal sphincter dysfunction. The next day I was 80% better. At this point, I could lie supine and breathe through my nose without any issue, however I still felt some pressure in my throat (still no other signs). Towards the end of September I had a treatment focused on my neural mobility both in my neck and around my sacrum that I would say got me to 90% improved. I also noticed, my neural tension in my L leg was significantly improved. I could also perform an overhead squat better than I had in years. This past weekend, I had my wife perform a visceral treatment on me for the 2nd time. This time her treatment focused on a liver lift and liver motility. Within a couple days I can now say I feel 99% improved with the remaining sensation being attributed to some neural restrictions in my neck per my wife. In a week or two, I'll have my wife address the final restriction in my neck. While the exact reason for the development of these symptoms isn't clear, my wife and her mentor believe it can be attributed to multiple things throughout my life: being born with my umbilical cord around my neck, hx of MVA, potential bad cervical treatment years ago, etc. I'm not sure I know which factors were most important, but what I do know is that the treatment was successful. While I was undergoing this management, I couldn't help but think about how important this kind of treatment is. The standard individual likely would have ended up going to an ENT physician, had multiple diagnostic tests done, and even potentially had exploratory surgery. Not only was a lot of money saved, but so was the potential stress and time. I know that craniosacral and visceral therapists frequently get mocked (especially from orthopaedic therapists) for having unusual care, but I believe there is a severe lack of understanding by general physical therapists. This type of treatment should not be looked down upon, but instead embraced by the profession as the implications could be incredible. It is hard to tell when visceral therapy may be playing a role in our patients, but I've been told that there may be a visceral involvement in as many as 80% of the standard orthopaedic cases. To help identify patients that may benefit from this treatment style, look for a post next week on how to screen for visceral involvement. -Dr. Chris Fox, PT, DPT, OCS
Many patients present to Orthopedic Physical Therapy clinics with pain in the region of their sacroiliac joint. However, simply because someone has pain in the region of their SI joint does not mean the SI is the cause of their problem. In many instances these patients also have low back pain, hip pain, and/or other neurological symptoms. In this post, I discuss when to focus treatment on the sacroiliac joint versus treating the lumbar spine. When evaluating patients with lumbopelvic issues, I try to determine if the patient has lumbar dysfunction, SIJ dysfunction, or both. While some sacroiliac joint testing is naturally built into my efficient lumbar exam, the priority of my treatments is based off the lumbar examination findings. A study by Dreyfuss et al states that "patients with confirmed SIJ pain rarely identify concurrent pain at or above L5. (1)" In other words, individuals with SIJ pain (via anesthetic block) rarely had lumbar spine pain as well. Therefore, if symptoms are reproduced in the lumbar spine during my joint assessment, I will usually start my treatment in this region. While the lumbar spine is always a great starting location, I do have other patients with a clear clinical description of SIJ dysfunction. For example, they have unilateral SIJ pain, clear MOI, reported history of hypermobility, etc... After evaluating the lumbar spine, I perform Laslett's cluster for SIJ dysfunction (see tests below). If the patient has 3/5 positive tests, the likelihood of SIJ dysfunction significantly increases (2). Clinically, I do not guide my treatment based off palpation of anatomical landmarks due to significant amounts of anatomical variability. For example, the female pelvis is shaped different than the male pelvis. Additionally, the shape and structure of a child's pelvis is vastly different than an older individual. In support of this rationale, the OCS current concepts on the pelvis and sacroiliac joint state that positional palpation of the SIJ region is 'creative at best.' In conclusion, patients with lumbopelvic dysfunction may have a lumbar problem, SIJ problem or both. Clinically, if symptoms exist above L5, I treat the lumbar spine first. If symptoms exist above L5 and the patient has >3/5 positive SIJ provocation tests, I treat the lumbar spine and the SI joint. Finally, if there is no lumbar pain and a positive Laslett cluster, I treat the SIJ joint. While the research guides me to the region of dysfunction, my examination and treatment is heavily based on movement analysis and identifying poor movement patterns. Additionally, it must be emphasized that the clinician needs to assess the thoracic spine, hips, and function of the core muscles when evaluating any patient with lumbopelvic dysfunction. -Jim Heafner PT, DPT, OCS Order of Treatment: |
| If you are looking to improve upon your clinical skills, orthopaedic knowledge and clinical decision making, consider joining OPTIM's COMT program. With OPTIM, you can expect a residency-like learning experience without breaking the bank, all while learning from highly skilled physical therapists. Check out optimfellowship.com for more information! |

As I've mentioned recently, I've been reading the McKenzie texts to build a better understanding of the foundation of repeated motions. One of the diagnoses that many believe indicates we should not perform repeated extensions is spondylolisthesis. For those of you unfamiliar with the pathology, it typically represents a fracture of the pars interarticularis and slippage of the vertebra relative to the adjacent ones. The theory is that repeated forceful lumbar extension is the cause of spondylolisthesis via repetitive microtrauama, as this is frequently seen in gymnasts, volleyball players, dancers, and more. In the book, spondylolisthesis was actually not presented as a contraindicated. According to Spratt et al 1993, those with spondylolistheses have actually been shown to have an excellent response to repeated lumbar extensions. Now this can be interpreted in a couple different ways. It's possible people had an asymptomatic spondylolisthesis while also presenting with a symptomatic "disc injury" (excuse the pathological explanation). More appropriately, the patient may still have an extension directional preference, meaning they improve with repeated extensions.
-Dr. Chris Fox, PT, DPT, OCS
Spratt KF1, Weinstein JN, Lehmann TR, Woody J, Sayre H. Efficacy of flexion and extension treatments incorporating braces for low-back pain patients with retrodisplacement, spondylolisthesis, or normal sagittal translation. Spine (Phila Pa 1976). 1993 Oct 1;18(13):1839-49.
| If you are looking to improve upon your clinical skills, orthopaedic knowledge and clinical decision making, consider joining OPTIM's COMT program. With OPTIM, you can expect a residency-like learning experience without breaking the bank, all while learning from highly skilled physical therapists. Check out optimfellowship.com for more information! |
Manipulations improve mobility. | The talocrural joint is commonly hypomobile in many individuals with knee pain or low back problems. In addition to hypomobility, the ankle often lacks adequate dorsiflexion range of motion and plantar flexion strength. A simple intervention to improve the joint mobility is a talocrural joint manipulation (see video below). We know manipulation is safe and effective in certain situations. However, many students question if manipulating an acute ankle sprain is appropriate. |
Joint manipulations are high velocity, low amplitude techniques directed at the joint
| When performing joint manipulation, there are only a few absolute contraindications. As with most aspects of physical therapy (and healthcare), the indication depends on a variety of factors. Regarding acute ankle sprains, the clinician must decide if the benefits of the technique outweigh the risks. If the individual has low to moderate irritability, minimal swelling, and decreased joint mobility, I choose to manipulate the talocrural joint following an ankle sprain. If the patient has excessive pain and guarding, I will use lower grade mobilizations to improve the joint motion. Personally, I am not too concerned with the grade (1-3) of ankle sprain (A grade 3 sprain will likely present with more pain and swelling. Therefore, the appropriate treatment is a lower grade mobilization.) The manipulation is a high velocity, low amplitude technique focused on the joint. Additionally, the distraction technique demonstrated above is performed in a mid-range of motion, not an end-range stress similar to the mechanism of injury. Overall, joint manipulation is a safe and appropriate technique following an acute ankle sprain. *Disclaimer: Always use clinical judgement and evaluate each patient on a case-by-case basis. When performing any manual technique, the practitioner needs to assess the patient's irritability level and use the appropriate differential diagnosis to rule out other possible diagnosis. -Jim Heafner PT, DPT, OCS | Absolute Contraindications to Manipulation -Neoplasm -Fracture -Acute RA episode -Empty end-feel -No working hypothesis (...plus a few others) |

Insider Access pages
We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!
Archives
July 2019
June 2019
May 2019
March 2019
February 2019
January 2019
December 2018
November 2018
October 2018
September 2018
August 2018
July 2018
June 2018
May 2018
April 2018
March 2018
February 2018
January 2018
December 2017
November 2017
October 2017
September 2017
August 2017
July 2017
June 2017
May 2017
April 2017
March 2017
February 2017
January 2017
December 2016
November 2016
October 2016
September 2016
August 2016
July 2016
June 2016
May 2016
April 2016
March 2016
February 2016
January 2016
December 2015
November 2015
October 2015
September 2015
August 2015
July 2015
June 2015
May 2015
April 2015
March 2015
February 2015
January 2015
December 2014
November 2014
October 2014
September 2014
August 2014
July 2014
June 2014
May 2014
April 2014
March 2014
February 2014
January 2014
December 2013
November 2013
October 2013
September 2013
August 2013
July 2013
June 2013
May 2013
April 2013
March 2013
February 2013
January 2013
December 2012
November 2012
October 2012
September 2012
August 2012
Categories
All
Chest
Core Muscle
Elbow
Foot
Foot And Ankle
Hip
Knee
Manual Therapy
Modalities
Motivation
Neck
Neural Tension
Other
Research
Research Article
Shoulder
Sij
Spine
Sports
Therapeutic Exercise
















 RSS Feed
RSS Feed