- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
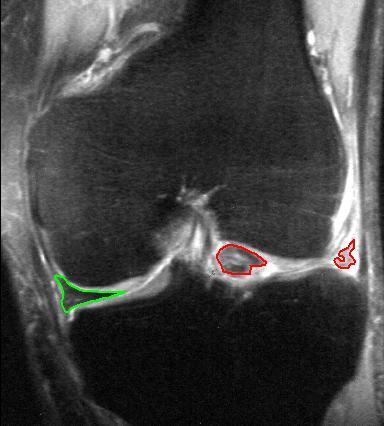
With this past month's JOSPT, an updated Clinical Practice Guideline (CPG) for Knee Meniscus and Articular Cartilage Lesions was released. Meniscus tears and cartilage lesions are commonly seen in the physical therapy setting. Once thought to require surgery, significant research has since revealed that outcomes are similar whether you have had surgery or physical therapy about a year later. While being able to identify the potentially injured tissue can be beneficial, treating the impairments remains the basis for intervention. However, because of the research that has been accumulated in managing meniscus and articular cartilage injuries, it is still recommended that we identify when these structures may be involved.
Now, some of the research for treating these injuries conservatively is based off of post-surgical management. A lot of the rehab is what you would expect: start with progressive active and passive ROM training and weight-bearing, followed by strength training in open- and closed-kinetic chain and neuromuscular training of lower quarter. Those are generally vague component to rehab but can be highly effective. Of course, not all cases are "text book." Sometimes (or often), the patient's perspective of what the injury is, or what they think it is, is more important than anything. It is extremely beneficial to educate the patient on the current pain science research, the lack of correlation between pathoanatomical injuries, and the success of conservative rehab for meniscus/cartilage injuries. The importance of progressive loading cannot be overstated. While part of the CPG, using regular and progressive loading can have both mechanical and psychological benefits. There is some research out there that high repetition, low load exercise can be beneficial for cartilage repair. On the biopsychosocial side, progressive loading of the injured area can address some of the fear and apprehension associated with injury. Either way, the main message to take away is that physical therapy can be a possible treatment for meniscus or articular cartilage lesions, based on the recent CPG's, mechanotransduction, and/or psychological benefit. -Dr. Chris Fox, PT, DPT, OCS
1 Comment
Today's post is from Meredith Castin of The Non-Clinical PT. Thanks Meredith!
You’ve probably heard plenty of grumbling about how the times are a-changin’ in the PT world. Reimbursements are falling and salaries are stagnant at best. Perhaps your loans are looming at epic proportions and you wonder how you’ll ever land a job where you’ll pay them off, much less make a solid living in the process. Here’s the thing. Lots of PTs are extremely successful in today’s healthcare climate--they’re just changing their approach by seeing themselves as a hot commodity and putting themselves out there as soon as possible. If you spend any time online (which you must, if you’re following this awesome website and reading this article), you’ll notice that some PTs are just savvy with technology. They’re putting themselves out there and they’re getting noticed. They’re interacting with influencers online and they’re making names for themselves before they’ve even finished PT school. They’re creating their own online brands for themselves, and you bet your bottom they’ll be the ones getting snatched up for the best jobs when they graduate! Frankly, I was not that person during school, and I regret it. I waited until I’d been out of school for four years before I even started to make a name for myself online, and I’m writing this article so that you don’t make the same mistake. Start That Website: If you’re a PT student or a new grad, you need to start a blog or a website--whatever you want to call it. It’s easy. Just hit up Wix or Squarespace, or Wordpress (that’s my fave and what I use for TheNonClinicalPT.com), and it’s blindingly simple to get things started. But here’s an inexpensive class to de-mystify Wordpress, just in case you like to understand all the bells and whistles, and get an idea of how to maximize your efforts. I do recommend taking a basic course. In any case, writing about a topic for long enough eventually makes you the expert on that topic. Whether you opt to stay in patient care or leave patient care to leverage your physical degree in a non-clinical career, you need to write about something at least loosely related to physical therapy. Write about what interests you, and what comes naturally. You’ll never find me writing about tibiofibular mobilizations because I don’t find that topic inspiring. I write about non-clinical careers about PTs because that’s what I know. As for you, you can talk about studying success, the trials and tribulations of being a student, careers, finding good clinicals, technology, networking, ballet, badminton, or whatever else you feel compelled to cover. Notice how I included ballet and badminton? When I first started writing, it was at the behest of my co-worker (at the time), Brett Kestenbaum, DPT. He wanted to start a website for new physical therapists and I was like, “I don’t really like being a PT. I don’t even know if I want to keep treating patients much longer. Why would I create a website to help new grads? What if I have nothing to offer? WHAT WILL I WRITE ABOUT?” Well, I figured, at least I knew I liked writing, so I went for it, and I wound up writing about the one thing I did know--how to get the most out of my degree without burning out. I didn’t enjoy treating full-time, so I covered topics about working per diem, preventing burnout, and alternate paths for physical therapists. Lo and behold, after I started writing about my favorite topics--leaving patient care and leveraging my degree to become a writer, I found that people started seeking me out to do exactly that: write. It was a wonderful feeling to finally build a career around something I love. And it wound up being my “golden parachute” for when I really did decide I needed to leave patient care behind. That’s why you need to write. You can’t predict what will happen to you. You might want to leave patient care, or you might want to land a dream job working with professional badminton players. Or dancers. If you write about dancing, even while you’re still in school, you know a hell of a lot more about dancing and PT than 95% of the public. And as you gain experience, that number will climb to 99%. And with your name out there as being the expert about dancing and PT, you’ll land those dream jobs working with ballet companies much more easily than if you were too lazy to start a blog. What If I Really Suck at Writing? It’s OK...if you really hate writing, or really suck at it, you have a few options:
The main point is that you’re putting yourself out there. When you’re a student PT or a Fresh PT and you’re competing with all the others to make a name for yourself, you simply have to do something special to stand out. Otherwise, you might find yourself ten years into your profession, wanting something new, and having to start from scratch when you’re already feeling burned out. I guess I probably should really have called this article “Why Every PT Student Needs to Put Himself or Herself Out There.” But that doesn’t really have the same ring now, does it? Author: Meredith Castin, PT, DPT (The Non-Clinical PT) Follow her on: Facebook | LinkedIn | Twitter | Instagram TheNonClinicalPT.com  If you work in a sports medicine environment like I do, then chances are you are getting quite a bit of ACL reconstructions this time of year. With ski season in full swing, unfortunately, many end up with ACL tears. However, a good majority of these patients are recreational skiers that like to dabble in many other sports. I recently had a few patients who asked about return to running following this surgery. This is always a time when I like to educate the patients on what I want to see from them to get them back to running. By establishing some criteria early on, it allows the patient to get in the mind-frame of what they need to accomplish as well as setting some goals. However, there are many different opinions to what should be established for return to running post ACL. From my perspective, besides time frame and MD clearance, I like to see a few biomechanical considerations. For example, I like to have a patient single leg squat a minimum of 10-15x under control with good form. What do I consider good form? Well, I often use the single leg stepdown criteria that has been established in some of the literature. Another thing I will look at is core stability. Specifically, I typically like to use a front plank with reciprocal arm drivers. The idea being that this test will look at rotational control when a patient is mimicking the arm swing during running. Again, a general time frame I use is at least one minute. Lastly, I like the reverse lunge for looking at great toe extension and hip extension. Remember that running is a full body exercise and it requires lots of moving parts. While the above is not completely comprehensive, it gives a good starting point to look at with running. Lastly, if you like this article, check out the post I made for New Grad Physical Therapy on some of the above criteria and more with pictures. Or check out our Insider Access page where I go into very detailed return to sport criteria and exercises for multiple different sports and movements, such as return to lateral agility. - Dr. Brian Schwabe, PT, DPT, SCS, COMT, CSCS Join Insider Access Today!Thoracic Outlet Syndrome: How is it Defined?Thoracic outlet syndrome (TOS) can be defined as a compression of the neurovascular bundle as it passes between the neck and axilla. Common compression points are between the anterior and middle scalene, between the first rib and clavicle, underneath the pectoralis minor, or potentially the presence of an extra cervical rib. Patients with thoracic outlet syndrome typically present with forward, rounded shoulders and a history of repetitive overhead motion. Both the neural and vascular structures can become compromised, but >95% of all cases are neurogenic. If you are suspecting a patient with neurogenic TOS cluster your TOS tests results with other neuro-dynamic tests. TOS Explained by Dr. Robert Thompson at Washington University in St. Louis How I Treat Neurogenic TOS: A Case Study ExampleEach individual case will have slight variations, but the examination section will be similar for each person My Personal Experience with Venous TOSIn 2010, my entire right arm started to swell. I went to the doctor and initially was prescribed antibiotics for MRSA. I had been paint-balling 2 days prior to the incident and had a few open wounds that were potentially infected. The doctor said to follow up in a few days if I did not improve. My arm continued to swell and became even worse with activity. At the second visit, I was told to go to the hospital to get a venous doppler for a suspect DVT. The doppler revealed a ~4 inch blood clot in my subclavian vein. I was immediately admitted to the ER, placed on blood thinners, and underwent a surgical procedure to remove the clot. CLICK BELOW TO CONTINUE READING -Jim Heafner PT, DPT, OCS Want to learn more from TSPT?
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|








 RSS Feed
RSS Feed