- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
In the push for advancing evidence-based practice in the orthopaedic setting, the APTA has been working on compiling the research for etiological factors, examination, treatment, outcomes, and more for various pathologies. These collections are known as the Clinical Practice Guidelines (CPG's). There are currently CPG's for these pathologies: -Neck Pain -Adhesive Capsulitis -Low Back Pain -Hip Pain and Mobility Deficits -Non-Articular Hip Joint Pain -Knee Ligament Sprain -Meniscal and Articular Cartilage Lesions -Achilles Tendinopathy -Ankle Stability and Movements Coordination Impairments -Heel Pain A couple years ago, the APTA released the CPG's for free viewing to all at this link. A lot of work went into developing these guidelines and they are some of the leading sources of evidence-based practice and preparation for the OCS. While the articles may appear lengthy, there are summary pages at the end of each one as well. Check out the CPG's when you get a chance for a great summary of current best practice! -Dr. Chris Fox, PT, DPT, OCS
1 Comment
Every year, around this time I start hearing questions about if it is worth pursuing clinical specialization. Recently, I even saw a forum post asking if the specialization warranted a raise. It's a highly debatable topic, but absolutely worth discussing. As you know, the APTA offers clinical specialization in various fields, like pedicatric, orthopaedic, sports, and more. To become a certified specialist, one must past the specialization exam for the respective field which is offered once a year. To qualify for the test, one must either complete a residency in the field or a certain number of hours (1-2 years worth usually) treating the appropriate field and apply for sitting for the test. Now, whether or not clinical specialization actually changes practice patterns or represents a true expert knowledge is a debate by itself; however, the question that comes more frequently is does it (or should it) translate to a raise. I think what is key to help justify a raise is how does it benefit your clinic. One might initially think improved outcomes, however, I believe that studies have shown little change in outcomes compared to non-specialists. It's not that specialization isn't worth it, but I believe it is not being marketed properly. My current clinic has done very little to market it. It is not labeled on our website, in our office or on my cards. Part of it may be to keep therapists appearing on the same level (to facilitate sharing patients), but it may be due to lack of knowledge of how to market it. I honestly do not know. While I did get a raise with specialization, I believe there are more benefits to pursuing specialization than just financial incentive. There are definitely aspects of evidence-based practice that are presented in each monograph for the OCS that are beneficial to clinical practice. Also, I think there is definitely something to be said about knowing a standard of orthopaedic knowledge and recognizing that level of knowledge with specialization. It is rewarding and can help identify clinicians with that knowledge. Additionally, it may open up opportunities that may otherwise have been closed. Recently, I interviewed with two companies that were looking to hire a clinical specialist as their staffs are primarily made up of specialists. While I did accept an offer from one of the companies, I cannot for certain say I would have had the opportunity to interview for either or both companies if I weren't a specialist. The potential benefits for clinical specialization lie beyond immediate financial improvements. -Dr. Chris Fox, PT, DPT, OCS
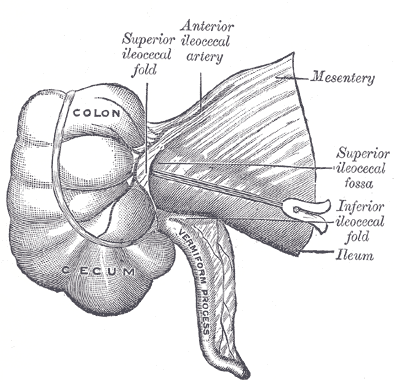
Recently, one of my co-workers was treating a patient that had been a couple times over the last couple years for the same injury: groin pain. While it had improved some with PT in the past, it never got 100% better. Typically, with recurrent "strains" we tend to think the nervous system is at fault, which leads to spinal and neural mobility training. However, in this instance, the patient was only having some improvement with dry needling (still never complete improvement in pain). While I am still far from proficient with my visceral manipulation techniques, my co-worker wanted me to take a look at this patient due to lack of improvement. The visceral manipulation course I took recommended a standard assessment of both general "listening" and local mobility testing. I have only been practicing local mobility testing. While there are more organs that can refer to the groin for pain than I am trained in, I was aware that the cecum can refer to that region, based on the material I was taught. I assessed and treated any mobility restrictions that I found in the 3 planes. As I've stated previously, the Barral Institute claims that effects for visceral manipulation may occur within 3 weeks of treatment; however, I have experienced the most significant changes occur within 3 days of treatment (not usually same day). When I followed up with this patient the next week, he claimed he was 100% pain-free for 3 days afterwards - something he had not experienced with any other treatment. Now there are too many variables to say that what I did or what I claim to have done was the reason this patient had an improvement. It may have simply been a novel stimulus to the nervous system. It may only be a temporary fix. There are many reasons to be skeptical; however, the fact that the symptoms could be affected by the treatment is intriguing. I look forward to learning more about the potential benefits of this treatment style and will be sure to keep you all updated! -Dr. Chris Fox, PT, DPT, OCS
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|













 RSS Feed
RSS Feed