- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
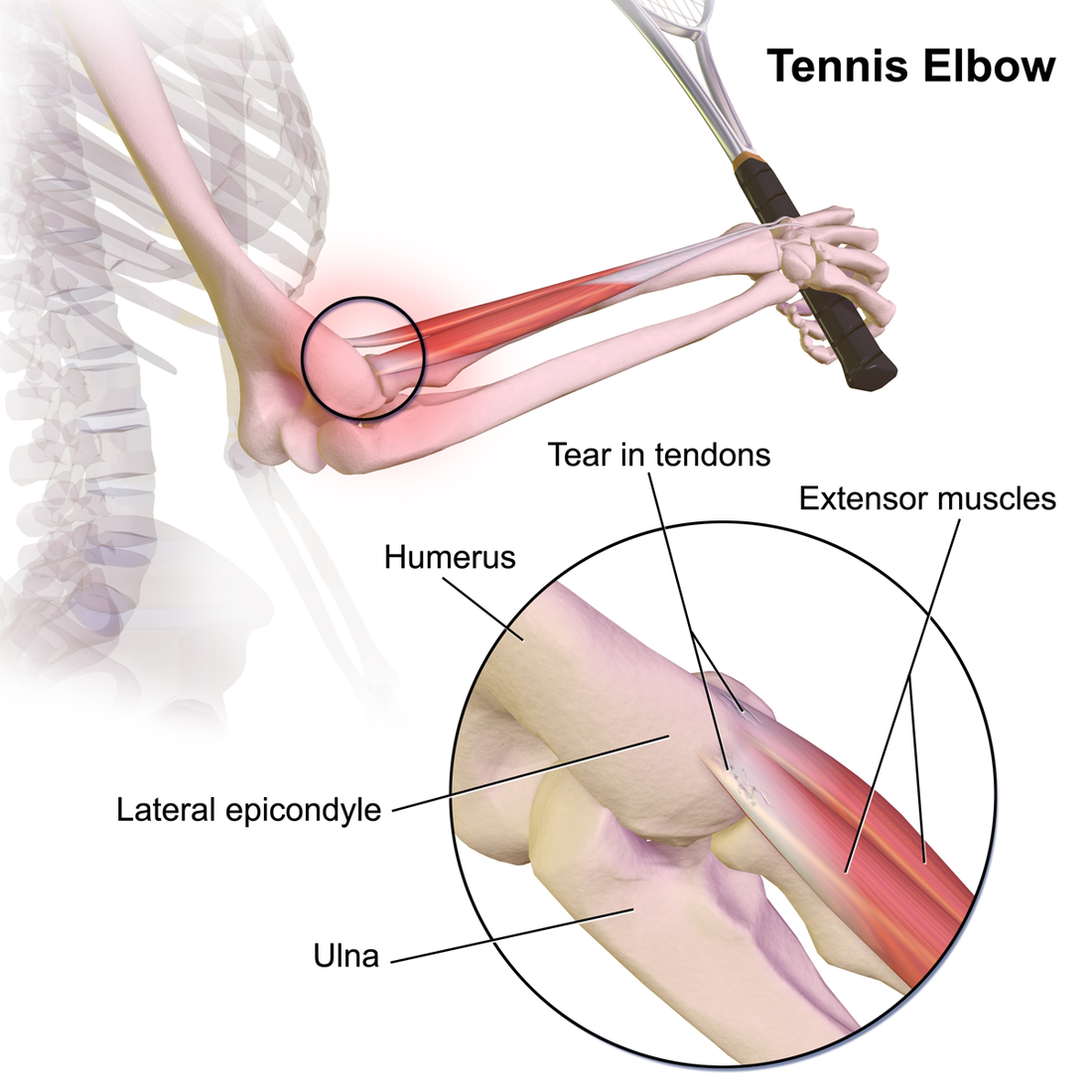
One of the topics we regularly return to is differential diagnosis. While ruling out non-musculoskeletal conditions is an aspect of this, we also want to be aware of diagnoses that present somewhat similarly but may be treated differently. Now, we recognize that pathoanatomical findings and management are not what we once thought they were; however, there are some differences on what the research shows for treating tendinopathy versus nerve entrapment. I won't focus much on treatment in this article, but instead on differentiating between the two diagnoses of lateral epicondylopathy and radial tunnel syndrome. Presentation: While both diagnoses often present with "elbow pain," the location may help indicate which diagnosis is more likely. Lateral epicondylopathy (LE) typically has some pinpoint pain over the lateral epicondyle but may radiate down into the forearm as well. Radial Tunnel Syndrome (RTS) typically has pain in the proximal forearm around the supinator (lateral to the brachioradialis) but distal to the lateral epicondyle. There may be some tenderness around the lateral epicondyle but it's not quite as significant as in lateral epicondylopathy. I recognize it sounds like these diagnoses are almost identical in pain location, but the proportion of pain location relative to the other is the leading factor. In fact, often ,in cases of lateral epicondylopathy, there is some radial nerve adverse neural tissue tension (ANTT) associated with it as well. Both LE and RTS symptoms are typically aggravated with increased use of the elbow/wrist muscles and alleviated with less use. RTS may be worsened with abnormal neck positioning/motion due to the altered neurodynamics. Additionally, the impact of compression may help with diagnosis. With appropriate positioning and force, compression of the forearm will "feel good" for LE and irritate those with RTS. Examination: As you likely may have noticed previously, I strongly encourage a standard exam, where most of the motions are tested for all upper quarter pain. This means I assess cervical, shoulder, thoracic, elbow mobility for all upper quarter patients. In diagnoses like LE and RTS, wrist/hand and forearm motion is assessed as well. With strength assessment, I will always test the shoulders, elbows, wrists, and scapula for upper quarter patients. How the patient responds to some of the tests may vary in the diagnoses. With resisted wrist extension, LE will likely be more painful than RTS although it may be painful in both. With resisted supination, RTS may be more painful than LE, but, again, it may be painful in both. Even though, the strength and mobility testing here may not appear super useful for differentiation, it is still beneficial for identifying impairments. Special Tests: Lateral Epicondylopathy: -Cozen's Test -Mill's Test -Maudsley's Test: resisted middle finger extension with palpation of lateral epicondyle Radial Tunnel Syndrome: -Radial Nerve ULNT (will reproduce patient's pain in RTS, but may still have some tension present in those with LE and associated radial nerve ANTT) A test that I learned but an unfamiliar with an official name involves trying to affect the pain via compression. The patient will make a strong fist and note the pain level (a dynamometer may be used for this as well to measure grip strength). The PT will then use his/her hands to compress the proximal forearm and the patient will make a fist again. Any changes in pain and strength will be noted. For a patient with RTS, the pain may increase and grip may be weaker. For those with LE, the counterforce will likely feel better and grip strength will improve. I'm unaware of the diagnostic accuracy of this test but has seemed useful and relates to the concept of counterforce bracing. Summary: It should be apparent that RTS and LE are not easy to differentiate as the pain presentations can be somewhat diffuse and testing may present similarly, especially in cases of LE with associated radial nerve ANTT. With that being said, I recommend starting with treating the associated impairments. Improve joint/muscle/nerve mobility where it is restricted and strengthen areas that appear weaker. Where being able to diagnose the primarily affected area become more important is management of the condition. Treatment to the cervical spine is especially important for cases of RTS as is isometrics/eccentrics for cases of LE. There is some research to show these benefits; however, patients with both diagnoses would likely benefit from these specific treatment anyways! -Dr. Chris Fox, PT, DPT, OCS
3 Comments
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|








 RSS Feed
RSS Feed