- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
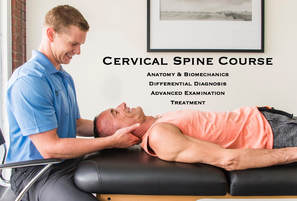
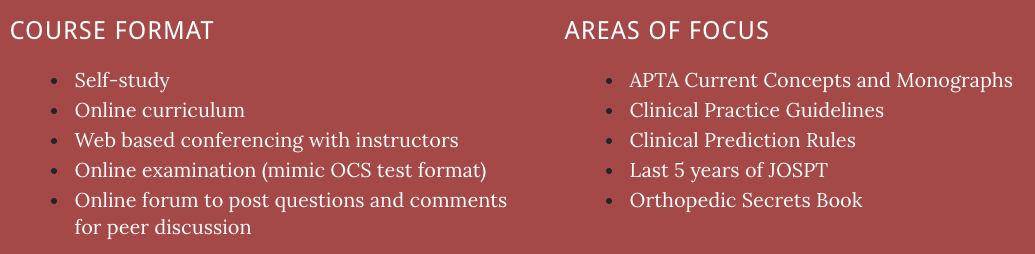
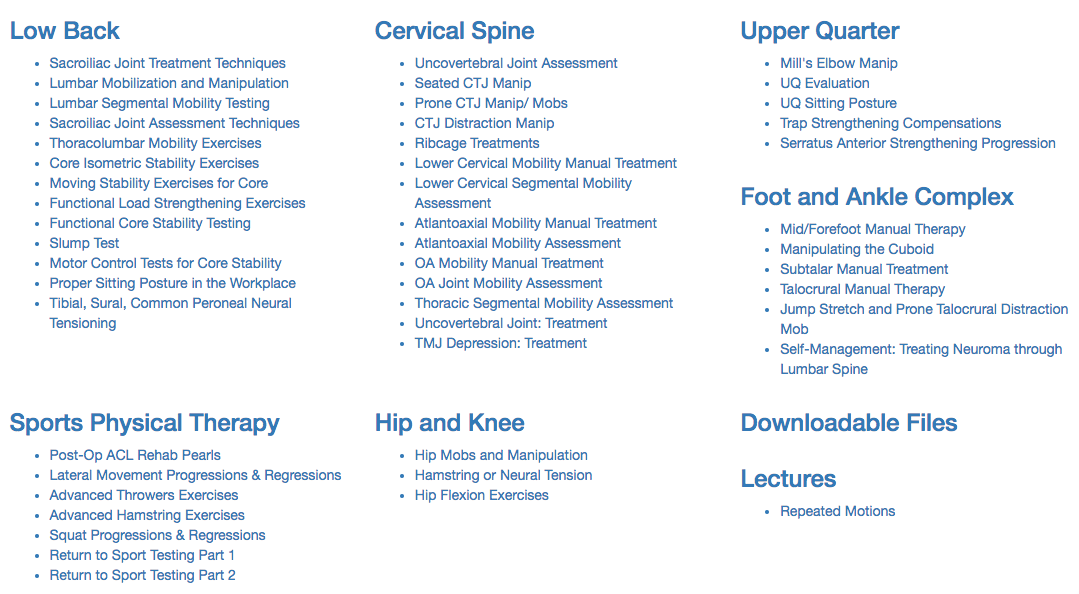
With the progression of evidence-based practice, much of the research that is being performed is looking to determine what treatment techniques are most effective for a variety of injuries. Included in that research is the development of clinical prediction rules (CPR's), which are used to take various exam findings and cluster them to determine more effective treatment measures. The below findings for individuals with neck pain were initially found to have significant benefit from thoracic manipulations (Cleland et al, 2007): There is an extensive process for developing a CPR that has true utilization and application. After a CPR has been proposed, it must go through a validation procedure. When reviewed, this CPR was unable to be validated (Cleland et al, 2010); however, those in the manipulation group were still found to have improved short- and long-term disability. Just because it didn't have the other original intended effects, doesn't mean it may not have a use. Whether thinking about the thoracic spine in an anatomical sense or a neurophysiological one, manipulating the region can be incredibly useful. The T6-7 area has been shown to be a tension point as the vertebral canal is relatively narrow compared to the spinal cord here. Additionally, there is little movement in the spinal core here relative to the adjacent structures. These restrictions can affect nerve irritability and function. With manipulation and mobilization, the biomechanical aspect of nerve mobility can theoretically improve or it may simply be stimulating the nervous system in a novel way (or it may be purely psychological). Either way, manipulating the thoracic spine can be beneficial for many injuries. It's definitely a skill worth practicing and implementing! -Dr. Chris Fox, PT, DPT, OCS References: Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL. "Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education." Phys Ther. 2007 Jan. Web. 08/18/2012. Cleland JA, Mintken PE, Carpenter K, Fritz JM, Glynn P, Whitman J, Childs JD. Examination of a clinical prediction rule to identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: multi-center randomized clinical trial. Phys Ther. 2010 Sep;90(9):1239-50. TSPT now offering a comprehensive Cervical Spine CourseInterested in learning more about the cervical spine?
Looking for advanced sports and orthopedic content? Take a look at our BRAND NEW Insider Access pages! New video and lecture content added monthly.
1 Comment
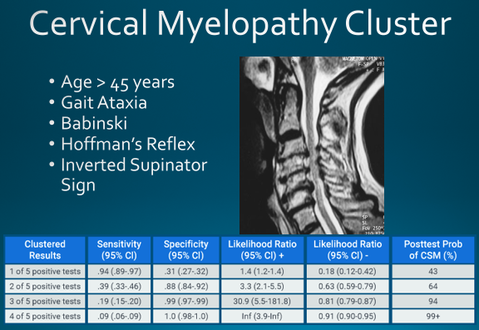
When I was going through Physical Therapy school, I remember struggling with the differential diagnosis of cervical radiculopathy versus cervical myelopathy. I knew both diagnosis' typically cause numbness and tingling, weakness, and sensory loss, but I did not fully comprehend the location of compression or WHY myelopathy had more widespread symptoms. Understanding the difference requires knowledge of cervical spine anatomy, neuroscience, clinical presentation, and more! OverviewChronic cervical degeneration is the most common cause of progressive spinal cord and nerve root compression. In fact, ~70% of asymptomatic people >70 years have degeneration in cervical spine. These spondylotic (arthritic) changes can result in stenosis of the spinal canal, lateral recess, and/or foramina. Stenosis is defined as ANY narrowing of a canal leading to nerve compression. Stenosis can occur centrally, compressing the spinal cord, OR laterally, compressing the nerve root. Chronic cervical degeneration is the most common cause of progressive spinal cord and nerve root compression. Cervical MyelopathyCentral spinal stenosis is known as myelopathy. An individual with myelopathy will present with Upper Motor Neuron signs and symptoms. These symptoms include gait ataxia, a positive Babinski test, a positive Inverted Supinator sign, a positive Hoffman's test, hyperreflexia, potential bowel and bladder changes, among other findings. Since the spinal cord is compressed, a referral for imaging is recommended to assess the amount of compression. Assuming the patient does not have severe compression with hard neurological findings, the patient will likely be appropriate to continue resume their Physical Therapy plan of care. How to Clinically Diagnosis Cervical Myelopathy
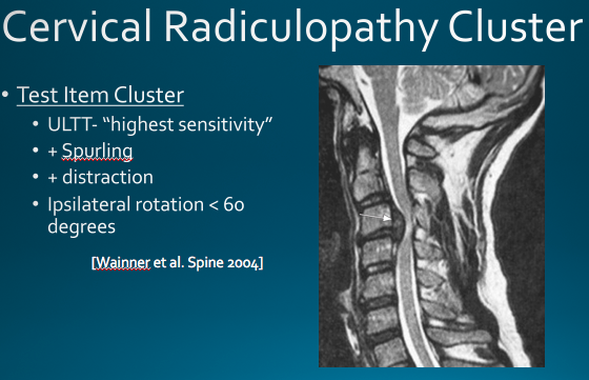
Cervical Myelopathy TreatmentConservative management (PT and anti-inflammatories) has been shown to be beneficial in providing short term relief of symptoms in Cervical Myelopathy. The goals of physical therapy should be symptom management, pain relief, preventing further neurological decline, and maximizing function. Additionally, patients should know that surgical management has not shown superior outcomes vs. conservative management at two year follow-up (1). Cervical RadiculopathyCervical Radiculopathy has significantly different symptoms than myelopathy. In radiculopathy, the nerve root (not the spinal cord) is the involved structure. When the nerve root undergoes compression or tension (any additional stress), individuals will typically have myotomal weakness, sensory loss in a dermatomal pattern, hyporeflexia, positive Spurlings Maneuver, positive Distraction Test, decreased cervical rotation to the involved side, and a positive median nerve tension test. How to Clinically Diagnosis Cervical RadiculopathyMost cases of cervical radiculopathy can be treated conservatively. Cleland et al found favorable treatment outcomes if the patient was <54 years old, a multi-modal treatment approach was used for >50% of the visits, the non-dominant arm was involved, and looking down did not aggravate symptoms. Cervical Radiculopathy TreatmentTSPT now offering a comprehensive Cervical Spine CourseInterested in learning more about the cervical spine?
References:
1. Kadanka Z, Bednarík J, Vohánka S, Vlach O, Stejskal L, Chaloupka R, Filipovicová D, Surelová D, Adamová B, Novotný O, Nemec M, Smrcka V, Urbánek I. Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomised study. Eur Spine J (2000) 9 :538–544 2. Cleland JA, Fritz JM, Whitman JM, et al. Predictors of short-term outcomes in people with a clinical diagnosis of cervical radiculopathy. Phys Ther. 2007;87(12):1619-1632 GENERALIST OR SPECIALIST?When I graduated with my clinical doctorate, I entered the workforce as a general Physical Therapy practitioner. In other words, I knew a little bit of information on a wide array of topics. For example, I could perform an outpatient orthopedic evaluation, but it was relatively sloppy and inefficient. During these early evaluations, I remember performing 20+ special tests and identifying upwards of 50 impairments. Looking back, I probably gathered enough information to give the patient ten different diagnosis. Unfortunately, the diagnosis’ were not clinically significant. Physical Therapy school gave me a general foundation, but I lacked expertise for ranking and prioritizing impairments (plus, the inefficiency added hours to my documentation!)* EXPERTISE REQUIRES EFFORT Similar to most physical therapists, I strive for excellence in both my personal and professional life. As a new graduate, I wanted to be a great practitioner, and I wanted to arrive at that gate quickly. The reality of becoming a clinical expert is that it always takes time and effort. You cannot shortcut your efforts because gaining experience is a key part of the process. Clinical expertise happens when research, experience, and intuition flow together. Shortcutting any aspect of this equation changes the final output. Becoming a clinical specialist in Orthopedics took months of time and preparation. I remember working my full time job as a clinic manager, enjoying a few hours with my wife, and then hitting the books from 10 p.m. to 1 or 2 a.m. They were long days. When looking back, it is natural to ask if the months of preparation were worth the ‘OCS’ credentials. The answer is a resounding, “Yes!” For me, there was no alternative. The idea of showing up to clinic average and not maximizing my results was not an option. The hard work and effort is a rite of passage from generalist to becoming a specialist. It is still the road less travelled, but a worthwhile adventure that will make you a better clinician. SPECIALIZATION MADE ME A BETTER CLINICIAN If you have remotely considered taking a specialty examination, it is likely that a colleague has said, “Why waste your time? The examination is a few years outdated and does not apply to real clinical problems.” Our profession is driven by our most up to date research. Without this research, the physical therapy profession would suffer immensely. Preparing for the Orthopedic specialty examination forced me to truly understand the research. For example, how many people perform eccentric contractions for Achilles tendinopathy? Great! Eccentrics are important. However, if your results are not 100% it is because there is more information behind the eccentric research studies. Some of the best eccentric research assessed ATHLETES with MID-PORTION Achilles tendinopathy. The athletes performed 180 repetitions each day often while working through pain. (1) The clinical practice guidelines for Achilles Pain, Stiffness, and Muscle Power Deficits Achilles Tendinitis mentions that insertional tendinopathy and non-athletes do not respond as positively to eccentric loading. An expert clinician tailors their treatment to the person, current irritability, pathology, and other biopsychosocial factors. The research helps guide the clinician on the best path and allows the expert clinician to intelligently pivot when something does not directly match our current literature. Specialization does prepare you for the clinical world! Expert practice forces you to critically analyze the decisions you make on a patient-to-patient basis. TAKE HOME ADVICE
*To clarify- this does not mean Physical Therapy school is not preparing students adequately. We are competent and safe entry-level professionals when we graduate. Physical therapy schools help people pass the NPTE. They do not have the bandwidth nor time to allow for specialization. Reference 1. Alfredson H, Lorentzon R. Chronic Achilles tendinosis: recommendations for treatment and prevention. Sports Med. 2000;29(2):135-146. OPTIM PREP COURSEOPTIM is offering $50 off the first 25 course participants with promo code First25. (Only 5 codes are still active before our October 1st launch date!) NEW TSPT INSIDER ACCESS LIBRARY!Looking for advanced sports and orthopedic content? Take a look at our BRAND NEW Insider Access pages! New video and lecture content added monthly.  About the Author: Jim Heafner PT, DPT, OCS is one of the founders of The Student Physical Therapist. He is owner of Heafner Health Physical Therapy in Boulder, Colorado.  As you are well aware, there are many applications for repeated motions. They can address deficits in mobility, strength, neural tension, DTR's, movement patterns, pain and more. One of the things that stood out to me the most when I was first learning about repeated motions, was how it applied to extremities through the spine. Just because there wasn't "radicular pain," neural symptoms, or central pain, didn't mean that we should just ignore the spine altogether. Having recently started at my new position, I have taken over several cases from other PT's. One older individual started PT with leg pain (no back pain), which is now resolved, but he was still having difficulty lifting his leg for ascending stairs or performing bed transfers. Upon examination, he had some passive hip mobility restrictions but his active SLR and hip flexion mobility were both significantly less than passive mobility. He also had significant restriction with lumbar extension (no major SGIS limitation noted). From my experience, a lot of hip mobility, strength and pain issues are resolved with treatment to the lumbar spine, even when no pain is present. I proceeded with some lumbar mobilizations. Following the lumbar treatment, he had full hip flexion PROM and nearly symmetrical active SLR. Now I may not fully understand the mechanism of why these changes have occurred, but I try to relate it to neural physiology. With any restriction in neural mobility, we see a loss in axoplasmic flow, which makes it easier for nerves to not function appropriately. I always relate it to a "kink" in the hose with water running through out. I simply try and help the patient get the "kinks" out by either performing a manual treatment or teaching the patient an exercise the gets the joints moving better that are limiting the nerve. What I try and apply to each patient is: start with assessing the spine (no matter the patient complaint!) and work your way down. By treating any restrictions you see, you will at the worst improve that areas mobility. You may, however, start to see some trends with subjective reports responding to spinal treatment. -Dr. Chris Fox, PT, DPT, OCS
Each year numerous athletes get “re-injured”. What are you doing for your return to sport process?!
Return to sport testing is always an interesting topic discussed within sports medicine. It is an ever-growing subsection of sports physical therapy. While we wait for research to catch up to validate and create reliable tests, what else can we do to put our athletic patients into the best possible situation for a healthy return? The most important thing with the return to sport process is understanding what components are necessary to consider. For many physical therapists this means ROM, pain, strength, and a few validated tests in the research (think hop tests). Yet this is not nearly enough to consider. In fact, it’s not even close. Let me explain some of the things I look at when treating athletes. Basic Measurements:
Task Analysis & Sport Biomechanics:
Psychological
Fatigue
Part 2 will cover specifics on loaded vs unloaded movements, sports specific tests, and return to sport tests! Stay Tuned! Dr. Brian Schwabe, PT, DPT, SCS, COMT, CSCS Board Certified Sports Physical Therapist IG: @brianschwabedpt  Recently, my family and I moved to Boise, ID and I started practicing at a new private practice clinic that is one-on-one for 45 minutes with each patient. For those of you unfamiliar with my work history, I had previously worked in both a hospital-based outpatient ortho clinic (for 1 year) and a high-volume private practice ortho clinic (for 3 years). There are many differences between each setting and different pros and cons to each one as well. Let's start with obvious cons of high-volume clinics: less time with each patient, difficulty with case management and therapeutic alliance, and possibly tech oversight. The worst part of it is that it can be more difficult to develop your clinical skills and clinical reasoning as you are more worried about getting to your next patient or managing your schedule, instead of focusing on the patient in front of you. The pros of a high-volume clinic are that you often are paid better (not always), you may see a more active population, and you get A LOT of exposure to different types of body parts, injuries or surgeries. Having worked in an hospital-based outpatient ortho setting, I would say that 70% of my patient population was chronic low back pain, deconditioning or balance issues. I probably saw 1 case of TMD and 1 or 2 wrist/hand injuries the entire year. Comparatively, I probably had 1 each of TMD or wrist/hand dysfunction throughout most of my time in the high-volume setting. Seeing more patients not only exposes you to more injuries, but also allows you to practice your techniques and skills on more people! You can become a lot more comfortable or proficient treating less common things just via exposure. I am hoping that my new setting will bring the best of both worlds: one-on-one care, diverse population, good pay, and more. The most important aspect in my opinion is one-on-one care. I cannot wait to get into proper exercise prescription, loading techniques, and, above all else, patient education. Empowering and educating our patients helps to build their independence and restore their function. While I look forward to my new position, I am extremely grateful for my time I spent in a high volume clinic. I feel much more comfortable treating a variety of injuries, managing cases, and using certain manual techniques. The busy clinic can still be a useful part of clinical development, although, I don't recommend it long-term. -Dr. Chris Fox, PT, DPT, OCS
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|











 RSS Feed
RSS Feed