- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
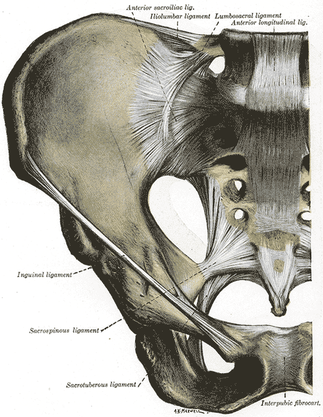
 Recently, The Manual Therapist wrote a blog post about what is most important when treating a patient: the what, the why, and the how. To relate it more directly, what you have refers to specific diagnoses. Why you have it refers to the theory of why the pathology occurred, i.e. movement impairment syndromes. The how refers to how we actually treat and assess. Much of medicine and physical therapy is often stuck in the "what" phase. We tend to assign diagnoses to tissue pathology and often look to treat what we believe is the source of the pain, not the original cause. Many physical therapists are moving towards the "why" mindset where we look at a more complete chain of the body to determine why our patients are in pain. This typically leads to a more well-rounded treatment approach. The "how" comes back to what we are actually doing and how we are treating our patients. I recommend reading the original post by Dr. E to get further clarification. This post comes with good timing in the wake of Tiger Woods' "sacrum" comments. In case you missed it, Tiger Woods recently played in a golf tournament and had to withdraw, because he claimed his "sacrum went out." As a result, there was a backlash from much of the young PT community claiming how it was a horrible diagnosis, Woods' physical therapist had poor communication skills, etc. The discussion lead to many physical therapists and physical therapy students ranting about how the research for SIJ Dysfunction as a diagnosis is poorly supported based on higher level evidence (which is correct) and some even saying how the SIJ doesn't move at all. Based on these comments, it would appear many do not assess or treat the Sacroiliac Joint. While I may agree that we shouldn't worry about actual tissue diagnoses, I get frustrated by people's reluctance regarding any potential SIJ treatment given my personal clinical success. In the residency at Scottsdale Healthcare, we were taught various assessment and treatment techniques for the SIJ, but the distraction manipulation could be used as a "shotgun" approach and treat typically any form of SIJ dysfunction. In my limited experience, in the patients I feel would benefit from the manipulation, they tend to be 100% within just a few visits. Now a manipulation by itself is never the answer alone, but it can be an extremely useful tool. We need to build on preventing future recurrences of pain and teach our patients to maintain improvement independently. Some patient's arrive at clinic in excruciating pain and are nearly pain-free after manual treatment. A manipulation and mobilization are not the only potential treatment for what some would diagnose "SIJ Dysfunction." Repeated motions towards the directional preference may be appropriate as well. Basically, many of treatment techniques like these have theories to support them, but the evidence is not always as established. That doesn't mean successful treatment techniques should be discounted. I again recognize our limited ability (and importance) of truly diagnosing what we think we see with the SIJ, but I must continue to stress the impact of when we assess, treat, and reassess. This is the importance of the how I discussed at the beginning. If the patient feels better immediately after a treatment technique, something I did had the desired effect! We currently are unable to be certain in knowing the exact mechanism our techniques have, but we should not ignore positive results. I have written extensively in the past about the problems with the studies regarding manual therapy, especially the SIJ, but that is not important in the end. What is important is that we find effective ways in getting our patients better as soon as possible. If that means doing a manipulation or mobilization where we think we are targeting the SIJ, then so be it. Do not let the limitations in higher level research prevent you from providing your patients with the most effective care. -Chris
17 Comments
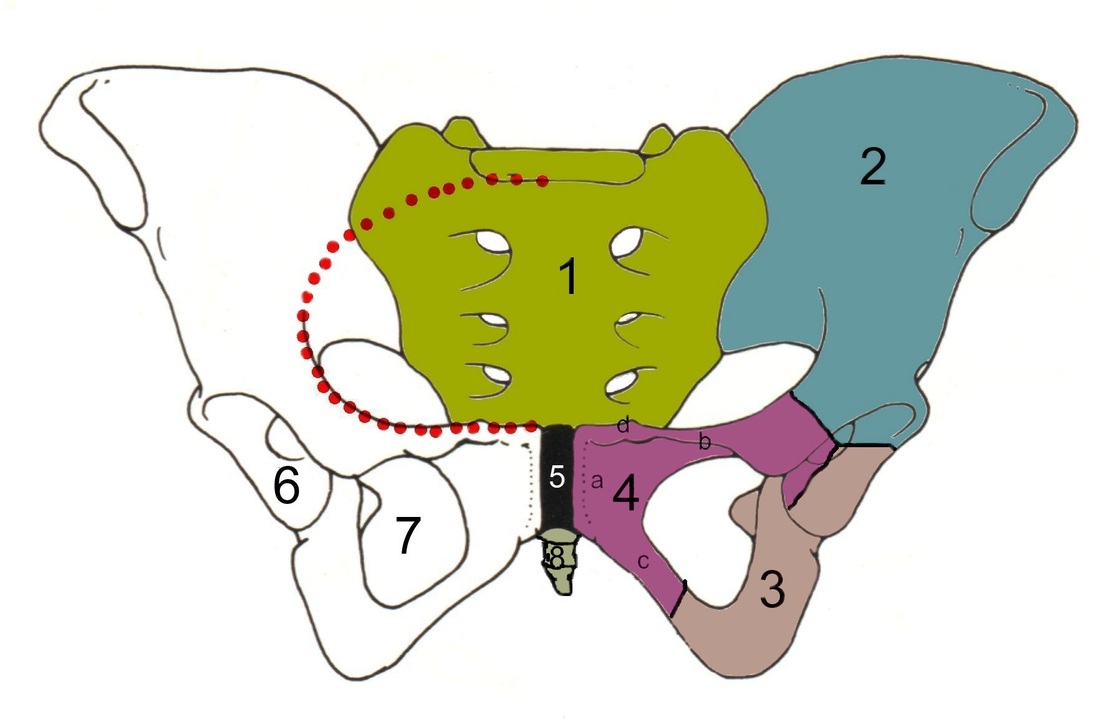
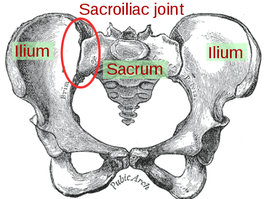 We are once again back on the topic of SIJ Dysfunction. A couple months ago, we had a pretty controversial post about non-painful sacroiliac joint dysfunction. A large part of our discussion was on the basis of how limitations in SIJ mobility could alter the normal stresses in adjacent joints. While we still believe this is an important aspect, in the past few weeks we have become aware of yet another reason for regularly assessing the sacroiliac joint. Something that is often lost in the effects of SIJ dysfunction is impact on muscle alignment. Any time there is a deficiency in the alignment of the joint surfaces, the origin or insertion of the muscles are altered, thus changing the moment arm of the muscle as it crosses its respective joint. These changes may seem small and insignificant, but they can result in both muscle pain and weakness. The significance of a muscle alignment issue is that these patients will likely not have many positive pain provocation tests, because it is not the joint that is painful - it is the muscle (or structures near the muscle). Therefore, when assessing the sacroiliac joint, be sure to assess the symmetry and depth of SIJ structures such as the PSIS, sacral sulci, sacral ILAs, ischial tuberosities, and more. In the past few weeks, we have had multiple patients with pain or weakness that was eliminated or minimized simply by doing a sacral mobilization or other manual technique to correct the asymmetry. These patient's had negative pain provocation testing but noticeable bony landmark asymmetries. We are aware of the fact that SI mobility tests are unreliable according to several research studies, but we again argue that they should not be forgotten. This brings up the importance of testing and re-testing after a treatment. A muscle that appeared weak initially in your eval may be normal after correction. If you can show immediate changes in pain and strength from a treatment directed at the SIJ, not only will it potentially alter your plan of care, but it also builds your patients' confidence in you as a clinician!
Jackson and Porter bring up the fact that there is essentially no research on the topic of non-painful SIJ Dysfunction. Once again, just because there is no research in an area, does not indicate that it should be dismissed as non-existent. We tend to become overly reliant on our pain provocation tests. So what do we do? We definitely recommend still utilizing your clusters, palpating soft tissue, and utilizing subjective information such as Fortin's Sign to aid in diagnosing painful SIJ Dysfunction. As for non-painful dysfunction, practice and implement the motion restriction tests that you are taught in school. We are trained to be competent in tests like Lachman's and Drawer Tests that require identification of differences in movement around a few millimeters. In theory, we should be able to identify some abnormalities in the sacroiliac joint as well. Now, we recognize that research has shown poor reliability for those tests and for good reason, but they may still aide in picking up severe restrictions that will lead to diagnosis and treatment in order to facilitate the return to normal mobility. Reference:
Jackson R and Porter K. The Pelvis and Sacroiliac Joint: Physical Therapy Patient Management Utilizing Current Evidence. Current Concepts of Orthopaedic Physical Therapy, 3rd Ed. La Crosse, WI. 2011.  We may have touched on Lower Crossed Syndrome in the past, but it is seen so frequently that is does not hurt to mention it again. Lower Crossed Syndrome is a common musculoskeletal disorder related to postural imbalances. In this syndrome, the patient will often present with short/strong hip flexors and lower back extensors. Contrarily, they will have lengthened/ weak abdominals and gluteal muscles. These diagonal patterns of imbalance create an imaginary "X" on the patient (hence the name "crossed" syndrome). This syndrome is typically seen in people who sit for long periods of time, allowing the hip flexors to shorten. Additionally, it can be found in athletes who use repetitive movements such as running. Clinically you will see an anterior pelvic tilt, lumbar lordosis, lateral rotation of the lower extremities, genu recurvatum, and alterations in arm/leg swing patterns during gait. The anterior pelvic tilt and lumbar lordosis may create increased compressive forces along L4, L5, and S1. Any compromise of the lumbopelvic muscles may lead to instability throughout the lower extremities, so your patient may present with low back pain, knee pain, or ankle issues. For example, the gluteus maximus is an important eccentric decelerator for hip flexion, internal rotation, and adduction. If the gluteus maximus is weak, it cannot stabilize the tibiofemoral joint properly during dynamic motion. Additionally, the tight hip flexors are placed in a better position for muscle contraction and consequently receive increased neural input. This reciprocal inhibition can lead to further tibiofemoral instability and knee pain. When treating these patients, postural awareness, lifestyle modification, stretching, and strengthening will be important. Remember to address the shortened muscle prior to intensive strengthening. The patient needs to have adequate muscle length before beginning a strengthening program. Also, always direct your attention to the cause of the patients symptoms. While they may be having regional symptoms, the true cause may be either proximal or distal to the symptoms.
As you might be aware, there are quite a few tests out there for the Sacroiliac Joint, many of which are based on alignment. Due to the low inter-rater and intra-rater reliability of these tests based on identifying asymmetries, pain provocation tests are preferred when identifying pain arising from the Sacroiliac Joint. Unfortunately, there is not one pain provocation test that has been shown to have sufficient diagnostic accuracy by itself. This has led to the use of clusters. Two of the commonly used clusters include: a) SIJ compression, SIJ distraction, POSH Test, Sacral Clearing Test, Resisted Abduction Test; b) POSH Test, Resisted Abduction Test, FABER Test. But how do we decide which one to use? This is an example of why we need to review the literature to assess the methodological quality.
Broadhurst and Bond performed a double blind study that utilized placebo and active injections to find the effects of each test. Pain had to be decreased by 70% to be determined as originating from the SIJ. None of those injected with saline had a sufficient decrease in pain. The study found that when Resisted Abduction Test, POSH Test, and FABER Test were clustered together, there was a high likelihood of pain of SIJ origin. This test, upon initial examination, appears to have respectable methodological quality. Stuber performed a systematic review that ended up including 6 studies that looked at special tests identifying SIJ Dysfunction. Broadhurst and Bond's study was included in the review. One of the components of the study was to assess methodological quality of each one. Broadhurst and Bond's study was ranked 3rd overall, due to deficits in number of participants, drop outs, and lack of description of the examiners and tests performed. While the cluster suggested by Broadhurst and Bond may still be useful, we should be cautious given the methodological flaws. The cluster with the highest evidence according to Stuber includes: -SIJ Compression -SIJ Distraction -POSH Test -Sacral Thrust -Resisted Abduction Test When any three tests out of the five listed below are positive, there is a sensitivity of .87 and a specificity of .91 |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|






 RSS Feed
RSS Feed