- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 Dosage is one of the most important factors to consider when prescribing an exercise. This decision is often made based off level of acuity, tissue type, anatomical location, patient age, and more. In school, one learns the general principles of exercise prescription, but what is often neglected is WHY you prescribe in certain ranges. "Mechanotherapy: how physical therapists' prescription of exercise promotes tissue repair" is a 2009 article published in the Journal of Sports Medicine that elaborates on this topic. Physiologically, what stimulates tissue repair of articular cartilage, muscles and tendons is a term called Mechanotransduction. In this article Mechanotransduction is defined as "the process by which the body converts mechanical loading into cellular responses." This can be thought of in clinical terms as what is occurring at the histological level to allow one to prescribe a certain exercise dosage without increasing the risk of injury. Mechanotransduction can be broken down into 3 phases: 1) Mechanocoupling: This is the physical load cells undergo while in repair. The physical load is transferred into chemical signals which stimulate cellular changes. 2) Cell-Cell Communication: When one cell is stimulated, other cells in the area (whether directly stimulated by the initial mechanical stimulus or not) will undergo a cellular response. 3) Effector Response: When a cell is mechanically stimulated through compression, distraction, etc., several processes will occur intrinsically to allow change to occur. Now knowing each of the 3 stages, you must think about them in relation to the Type of Tissue involved to understand how that tissue heals. Tendon Healing: When a tendon is trying to heal, there is up-regulation of insulin-like growth factor, other growth factors, and cytokines which allows for cellular proliferation and tissue remodeling. Because healing is occur at the cellular level, too much stress OR too little stress on the tendon tissue could cause an alteration in the up-regulation, not allowing the tendon to rehabilitate optimally. The research up-to-date shows that tendons responds positively to "controlled loading." Research focusing on the type and intensity of controlled loading (eccentrics, assisted, resisted) is still ongoing. Muscle: The authors Khan and Scott state that "muscle offers one of the best opportunities to exploit and study the effects of mechanotherapy" because of how muscle tissue responds to loading. We know there is an overload of mechanogrowth factor (MGF) released when load is induced on the muscle force. This in turn causes muscle cell hypertrophy due to a cell-to-cell communication with nearby satellite cells. At this point, the research shows that early loading after a brief immobilization period is essential for minimizing atrophy and restoring normal cellular structure of the muscles. Articular Cartilage: Articular cartilage is comprised of a large population of mechanosensitive cells. It is hypothesized that by repetitively stimulating the articular cartilage with a low load/high repetition exercise dosage, better outcomes will result. One study assessing full thickness cartilage defects following periosteal transplantation demonstrated that individuals who used continuous passive motion (low load/high repetitions) had greater outcomes than those who did not receive this intervention. As with all things, research is ongoing. Bone: When assessing bone healing, osteocytes are the primary mechanosensors. A recent study looking at individuals following a distal radius fracture had stronger bone growth if they received intermittent compression as an adjunct to the standard of care (compression & gripping exercises). The pneumatic compression allowed for extra stimulation of the bone cells and an increased healing rate. We know parts of this article are dense, but understanding what is occurring at the cellular level can greatly change your viewpoint of how various tissues heal. Through each of these tissues we can see that Mechanotherapy plays a unique role in healing of different tissues types. The healing of osteocytes differs from that of chondrocytes which differs from myocytes. It is fundamental to understand these differences in order give appropriate doses during exercise - just as it is important to know the tissue type you should be treating following your examination. As a general rule of thumb: Articular Cartilage: Low Load, High Repetition; ~15% 1 RM; Thousands of repetitions. Tendon: Controlled Loading; consider eccentric exercises, but do not overload the tissue. Muscle: allow for a brief period of immobilization to restore homeostasis following injury. Bone: Based on location of the fracture, consider adding compression to your treatment to improve rate of bone growth and decrease healing time. References:
Khan and Scott. (2009) "Mechanotherapy: how physical therapists' prescription of exercise promotes tissue repair." British Journal of Sports Medicine. 2009; 43: 247-251. Web. 5 Dec. 2013.
2 Comments
2. Check Patient Compliance: This is a big one and a common culprit. It is our job to educate our patients on why it is essential that they are regularly performing their HEP. If you think how much time our patients spend working with us compared to being outside the clinic, any significant gains must be made (or maintained) independently. With regular performance of an HEP, we should expect to see a weak muscle get stronger, an adaptively shortened muscle lengthen, etc. If we are not seeing the expected improvements, it's time for another chat with the patient. Patients will often complain of not having time to do their HEP. It is here we must tell the patient that we cannot accomplish what we want to do in the clinic without the expected results from a regularly performed HEP. If they are too busy, maybe they need to reschedule their appointment once they have found time.
3. Refer Out: Physical therapy is sometimes used as a diagnostic tool for physicians. We are movement experts and often have a different perspective to offer when examining patients compared to medical doctors. This option actually has a couple different considerations. As you might have guessed, we all likely have impairments that would benefit from physical therapy. Whether or not these impairments are linked to the pathology is a separate issue. That explains why failure to respond to physical therapy after a month is a red flag. Another concern in this area is musculoskeletal pathology that sometimes benefits from skilled physical therapy. An example is meniscal tears. A study came out last year showing that conservative management of meniscal tears was just as successful as surgical outcomes. However, this does not mean that everyone will always respond to physical therapy. If after a few weeks the patient has not seen any significant improvements and is experiencing acute locking/catching in the joint, this patient may not be appropriate for conservative care. This applies to other pathologies as well.  As the new year is beginning, residency applications are nearing the deadline dates. As you have gathered from our previous posts, we are all learning a ton of useful information at our respective residencies. Each of us has our biases regarding who is learning more than the others, but what we do know is that we are each developing into great clinicians. Our specific residency deadline applications are due: Harris Health System Orthopedic Residency- February 3rd, 2014 Scottsdale Healthcare Orthopedic Residency- March 1st, 2014 University of Southern California (USC) Sports Residency- April 1st, 2014 See the full list of residencies here. 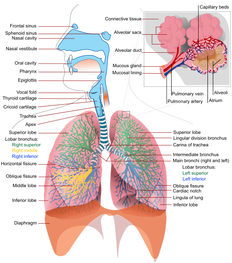 Physical therapy school teaches you some of the fundamentals of the respiratory system: anatomy, physiology, breathing patterns, etc. While these are important, sometimes the assessment and treatment techniques are over-simplified. Not all breathing or respiration deficits can be managed by attempting to train diaphragmatic breathing. The Manual Therapist recently had a post that reviewed some of the physiology and implications of managing breathing, along with the use of something called a Capnotrainer. What is really interesting about this post is how the physiology of the respiratory system impacts us as clinicians and what we can expect to see. This is something often lost upon us as we are scrambling to prepare an exam. With a true understanding, we can more appropriately select interventions for our patients. 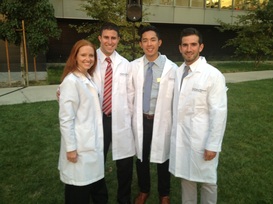 Who is going to CSM this February?! Many of you have emailed, tweeted, and facebooked us about meeting up and connecting. For those of you who would like to network and are going to CSM, this is the perfect time! One of our authors, Brian, will be attending CSM this February. Brian will be one of the representatives at USC's Sport's residency booth at the CSM Residency/Fellowship Reception on Wednesday, February 5th (6:30pm-8pm). If you can't make the Residency/Fellowship Reception at night, come check out USC's booth (#545) to learn more about both their sports and orthopedic residencies. Director Aimee Diaz will be working the USC booth on Tuesday (12:30pm-1:30pm) and Wednesday (1:30pm-2:30pm). Sports Resident Jon Hernandez will be at the booth on Tuesday (10:30am-12:30pm) and Brian will be at the booth Wednesday (11:30am-12:30pm) and Thursday (1:30pm-2:30pm). For those who would like to meet any of USC's orthopedic residents at CSM, email Brian and he will help set that up for you. All of us at TSPT would encourage any residency applicants to speak with residency directors and current residents to really know what the residency includes. See you at CSM! - TSPT  Some of you may remember reading this post on Doctors of Physical Therapy Website about a year ago, but we believe its message is consistent. One of the biggest barriers to changing our profession is a lack of patient education and understanding of who we are and what we do. This post presents a simple, consistent message: " I am (a) ___________." -Musculoskeletal Expert, Movement Analysis Specialist, Direct Access, Cost Effective, etc. We must advocate for our profession from the Patient-Upward and not strictly Top-Down. We cannot expect to persuade the AMA or Insurance Companies to give us rights if we have little support from our consumer. Spread the Word!!!
 We have made several posts on our residency experiences this year. These posts discuss in detail what a residency program is, how we chose our respective residencies (Harris Health Systems Orthopedic Residency, Scottsdale Healthcare, and USC Sports Residency), and most importantly why we chose to pursue a residency. We hope everyone found this information useful. Recently, Melissa Dreger, a University of Pittsburgh student added a post in the AAOMPT Student Sig discussing residencies and fellowships. This post is broken down into 4 main categories and gives you a step by step process to follow when making the decision to pursue a residency or fellowship program. The post also has links to different residency pages and links on how to apply. As Residencies and Fellowships continue to become more popular, there is a growing amount of information pertaining to these topics. We highly suggest you take full advantage of these resources. Choosing a residency program is similar to choosing a PT school. The right program can shape your career in ways you have never imagined. 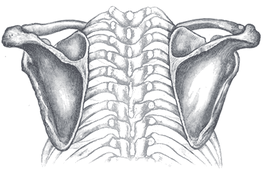 With the vast amount of locations that non-musculoskeletal conditions can present with pain in the thorax, one red flag that often stands out is pain in the middle of the back. A patient that presents with a case of simple neck or shoulder pain resulting from forward head posture may appear to have red flags with night pain of the mid thoracic spine. However, with further questioning you will often discover that the patient prefers to sleep with multiple pillows, reproducing the forward head posture and potentially disc irritation. A pain presentation that is fairly common that we should be aware of is Cloward Areas. Cervical disc irritation has the tendency to refer to the mid thoracic spine and the scapular border. Think about how lumbar disc irritation can essentially refer down to the knees (and sometimes below). The cervical spine has the same feature. With careful questioning of when the thoracic pain comes about, you may notice that it occurs with sustained positioning of forward head posture and disappears with correction, thus lowering the likelihood of non-musculoskeletal involvement. This article contains a good summary of the abstracts related to Cloward Areas. Some of the studies discuss the usefulness of various imaging methods in diagnosing symptomatic discs. This is interesting because it recognizes the difference between symptomatic and asymptomatic radiological findings - something many overlook. What we must remember however, is that we do not treat the pathology based on imaging. We treat the impairments. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|







 RSS Feed
RSS Feed