- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 Over the last year I have seen more and more athletic pubalgia in the clinic. Some of this is because of the population of athletes I have seen and some of this is because of the sports medicine doctors I work with. Athletic pubalgia (also known as sports hernia) is also defined as non-specific referral of groin pain. This injury can be complex to treat or very straightforward depending on the severity. Understanding how to determine if this is a AP and how to effectively treat it to return back to sport is crucial for the sports clinician. Typical presentation of athletic pubalgia includes:
Other pathologies to consider:
One of the key points to make with AP is that despite the term “sports hernia”, AP is not a hernia. Furthermore, this injury can be chronic in nature. With all that in mind, there are many conservative treatment options. From a conservative standpoint, treating AP has some non-negotiables. The first phase as many pathologies require, it to control the pain and symptoms. The length of this phase will be determined by severity, sport demands, and previous injury history. However, there are many other things you can do during this phase away from the site of injury to keep the athlete in shape. It is crucial to maintain cardiovascular endurance and strength elsewhere to give the athlete the best chance of returning without another injury later. Following the first phase you can you can start to work on more advanced core strengthening with “neutral spine”. I say neutral for the purpose of discussion and because most research articles advocate neutral spine but understand that everyone’s “neutral” is different. Another important point to consider during this phase is the influence of the lumbar spine. As with almost all hip injuries, we MUST consider the influence of the lumbar spine. Make sure full ROM is achieved and good control over the stability of the lumbar spine as it will influence the pelvis. More often than not, we can indirectly influence AP with lumbar spine treatment. Lastly, slowly adding adductor specific exercises from isometric in nature to more dynamic is important to add proper strength back to this athlete. I like the Copenhagen plank for a good isometric exercise vs squeezing a ball because it is hard to quantify the “squeeze”. There are many different forms of Copenhagen exercises and I would urge you to watch youtube videos, try them yourself, and determine if and when each variation can assist (or not) with your athlete’s rehabilitation. Finally, as with all injuries, proper return to sport criteria MUST be measured. While hip return to sport tests are few, there is good research on some tests and more importantly, a proper “battery” of tests must be put together. There is no one approach for return to sport and for those of you who have gone through our “Sports Management for the Orthopedic Clinician” course, you already learned how to put your own battery of tests together for various hip pathologies and how to properly construct return to sport testing. Dr. Brian Schwabe, PT, DPT, SCS, COMT, CSCS Board Certified Sports Physical Therapist
2 Comments
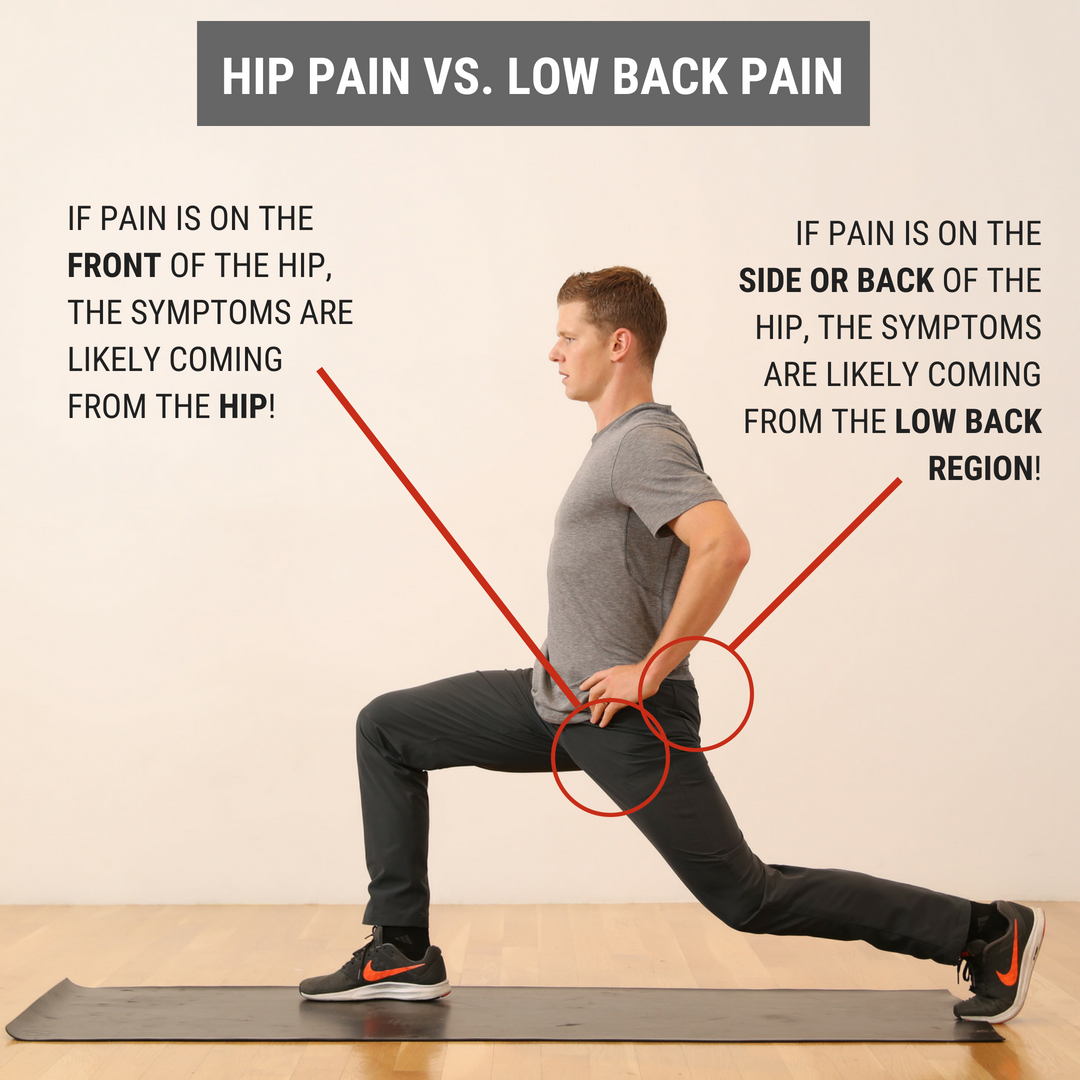
 I recently evaluated a patient who came into the clinic with the self- diagnosis of right hip pain. When I asked him where his hip hurt, he pointed to the back of his hip joint, just lateral to his sacroiliac joint. Upon further subjective history, he stated the current pain was very similar to his left hip pain that forced him to have a hip replacement 3 years prior. Needless to say, he was worried his current hip pain would lead to another hip replacement in the future. During the objective examination, I found this patient to have decreased hip flexion, internal rotation, and extension. While he had limitations in joint mobility, general hip quadrant and scour testing was negative. Looking at regional joints, the patient reported exquisite tenderness to palpation with PA assessment from L4-S1. Additionally he experienced pain with end range lumbar flexion and right rotation as well as various core stability tests. Most notably, his primary report of hip pain was reproduced during the lumbar cardinal plane testing. Since this gentleman had both hip and lumbar impairments, where was the BEST place to start? Initiate Treatment at the Hip or Low Back?During any hip examination, I always assess the lumbar spine. Since these body regions are connected via the pelvis, pain or symptoms in one region can directly impact the other. Additionally, I always use the patient's location of symptoms and mechanism of injury to help guide my diagnosis. As a general rule, if the patient reports that their pain is located anteriorly, symptoms are likely coming from the hip joint. From a movement perspective, less motion exists in hip flexion, adduction, and internal rotation, which places the anterior hip joint in a compromised position if pathology, such as hip OA or FAI, is present. If the patient reports their pain is located posteriorly, symptoms are likely coming from the low back region. Both the lumbar facet joints and regional nerves often refer posteriorly. While the L1-2 dermatomes can refer to the anterior hip joint, these nerve roots are less often irritated, which decreases the likelihood that the spine is causing anterior hip pain. There are always exceptions to this rule, but it is a great starting point to help guide your treatment selection. What Did I Do with My Patient on Day 1? Since his pain was reproduced with low back cardinal plane testing, I focused FIRST on the lumbar spine, then SECOND on the hip joint. During the initial visit, I did Trigger Point Dry Needling at the L4-5 multifidus and gluteal muscles. Then, I performed L5-S1 joint PA mobilizations to improve lumbar mobility and a hip long axis distraction manipulation. For his exercise prescription, he was given quadruped hand to heel rocks & repeated supine hip internal rotations. These both focused on improving mobility in general and desensitizing the patients pain.
Interested in learning more about the hip?
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|






 RSS Feed
RSS Feed