- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
Adhesive capsulitis (a.k.a frozen shoulder) is associated with synovitis and a capsular contracture of the shoulder joint. (1) Patients with frozen shoulder often have limited active and passive range of motion, significant pain throughout their shoulder range of motion, and associated upper quarter muscle strength deficits. Since the joint capsule is suggested to be the structure limiting movement, range of motion deficits are often greatest in shoulder external rotation > abduction > internal rotation. While adhesive capsulitis is often thought to be a self-limiting condition, studies have reported "ranges of between 20 and 50% of patients with adhesive capsulitis which suffer long-term ROM deficits that may last up to 10 years." (2) As a healthcare practitioner it is important to know the expected prognosis and understand the potential for long-standing symptoms does exist. It is also important to understand what is the current best evidence for treatment of adhesive capsulitis and common management strategies if conservative management fails. In this post, I will be discussing one of the surgical management options for adhesive capsulitis: Shoulder Manipulation under Anesthesia (MUA). How is a Manipulation Under Anesthesia Performed?While several different approaches exist, here is the shoulder manipulation under anesthesia technique as outlined by Shoulder Doc (see reference below): "The surgeon should stand at the head end of the table with one hand stabilizing the scapula in the resting position. The surgeon's other hand should then be placed in the patient's axilla such that the surgeon's forearm is resting against the whole of the inside of the patient's arm. First, abduction is taken to the patient's free limit, and then the patient is forcibly abducted while the scapula is maintained down in the anatomic position. The scapula must not move at any stage. This maneuver will rupture the inferior capsule. The shoulder is then forcibly adducted such that the affected elbow is pushed in front of the patient's chin to rupture the posterior capsule. Finally, forcible external rotation and internal rotation are added, but great care is taken here because it is during these final rotation maneuvers that a spiral fracture can be caused." (3)
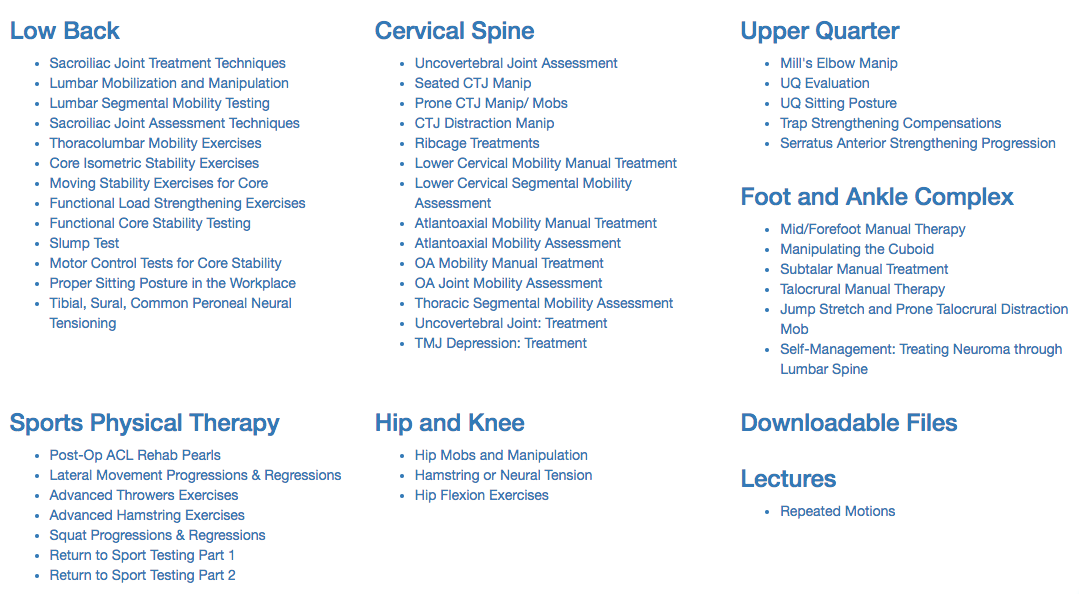
As a DPT, What Should I Consider Post-Manipulation?1. Post-manipulation range of motion should be initiated within the first few days following the procedure. This will vary from surgeon to surgeon, but many protocols recommend physical therapy within 24 hours post-surgery. Early range of motion and education is essential! 2. While the manipulation is targeted at the joint capsule, other structures are likely to be torn or injured. A 2005 study by Loew et al assessed 30 subjects with shoulder synovitis following MUA. They found "the capsule was seen to be ruptured superiorly in 11 patients, the anterior capsule was ruptured up to the infraglenoid pole in 24 patients, and 16 patients each had a capsular lesion located posteriorly. In 18 patients no additional joint damage was found after manipulation. In 4 patients, iatrogenic superior labrum anterior-posterior lesions were observed. Further injuries detected were 3 fresh partial tears of the subscapularis tendon, 4 anterior labral detachments (1 with a small osteochondral defect), and 2 tears of the middle glenohumeral ligament." In other words, the manipulation is not a specific technique. 3. Due to the amount of stress across the shoulder, mitigating pain while maximizing range of motion should be your primary focus of treatment! What is my Patient's Prognosis After Manipulation?Depending on the research article, the post-manipulation prognosis is scattered with results ranging from no effect to moderately effective. Per the clinical practice guidelines on Shoulder Pain and Mobility Deficits: Adhesive Capsulitis, there is Grade C for effectiveness of a MUA. This indicates relatively weak evidence for use of the intervention in individuals who are not responding to conservative care. Picture taken from Shoulder Pain and Mobility Deficits: Adhesive Capsulitis, page A23. My Clinical RecommendationDespite the weak evidence, we will continue to see these patient's post-surgery. When explaining the evidence and procedure to your clients, be honest and upfront regarding the procedure, but do not perseverate on the other injured anatomy or weak evidence for outcomes. This information can create a negative mental impression of conservative treatment, and reduce the overall patient outcome. Focus on treating that individual patient and reinforce positive improvements in their range of motion and strength. While our current evidence is lacking, that does not have to dictate the outcome with future patients! -Jim Heafner PT, DPT, OCS References: 1. Adhesive Capsulitis - Physiopedia, universal access to physiotherapy knowledge. Physio - pediacom . 2017. Available at: http://www.physio - pedia.com/Adhesive_Capsulitis. Accessed March 28, 2017. 2. Bulgen DY, Binder AI, Hazleman BL, Dutton J, Roberts S. Frozen shoulder: a prospective clinical study with an evaluation of three treatment regimens. Ann Rheum Dis. 1984;43:353–60. doi: 10.1136/ard.43.3.353. 3. Manipulation under Anestesia. Shoulder Doc. 2017. Available at https://www.shoulderdoc.co.uk/article/1223. Accessed 12/25/17. Learn more from us at TSPT on our Insider Access Library
0 Comments
Something I have been assessing more lately is rib mobility for my upper quarter patients. In the past, unless there were signs indicative of rib dysfunction, I typically only checked the 1st rib's mobility. Lately, I have been assessing ribs 2-4 (and further down if significant restriction noted) for many of my upper quarter patients and seen some interesting effects.
Several patients I've seen recently with scapular and/or posterior shoulder pain have presented with restricted rib 2-4 mobility (or some variation). They didn't have any pain with breathing, however, had significant reduction in pain and improved mobility following simply grade IV mobilizations to the restricted ribs. Even greater improvement was noted in the following day. Now the mechanism is not fully understood as manual therapy can have quite a few different effects. It's possible the patient would have had just as effective or more effective response to other treatments. Nonetheless, with the excellent response by my patient, I plan on regularly incorporating upper rib assessment to determine if there are some patterns for application. -Dr. Chris Fox, PT, DPT, OCS Looking for advanced sports and orthopedic content? Take a look at our BRAND NEW Insider Access pages! New video and lecture content added monthly.
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|










 RSS Feed
RSS Feed