- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 As physical therapists, we will commonly be asked about running shoes. What is the best shoe on the market? Should I try a minimalist shoe? In this gait guys blog post, they discuss the Dual Density Foam Running Shoe. The authors, Shawn and Ivo, go into detail on what a patient's static posture in a Dual Density shoe could potentially indicate. You need to ask yourself.... Is the person a supinator in a stiff shoe? Is the person an over-pronator that statically stands in excessive supination for support? Could a Tibial Varum be influencing the position of the foot? Where exactly is the pronation occuring? Rearfoot or Midfoot/ Forefoot Pronation? These are all valid questions and performing that differential diagnosis is important! The answer is, it all depends on that individual patient. You must do a complete evaluation with the shoe on and shoe off to see how the patient reacts in both circumstances. Note: Since the Gait Guys have a continuous, running blog, you might have to scroll down to November 21 Post (look for dates on the left side of the blog to see the specific article we are discussing. Look for the title "Dual Density Foam Running Shoes."
2 Comments
 No matter where you do your rotations or practice physical therapy, you are bound to work with both people who target the VMO with their interventions and people who think it's impossible to do so. Following trauma, knee surgery, or patellofemoral pain syndrome, many practitioners claim selective atrophy and weakness of the VMO relative to the rest of the quadriceps. This becomes a focus of several interventions in the patient's care plan. Due to the controversial state of this case, we thought we would do a review on the isolation of the vastus medialis muscle. CONTINUE READING  In order to appreciate this article from Dr. Craig Liebenson, we must first define regional interdependence. "Regional Interdependence: Seemingly unrelated impairments in a remote anatomical region may contribute to, or be associated with, the patient's primary complaint. (Wainner 2007)" You must look both proximally and distally to the site of pain. It is important to note that this term is not the same as referred pain. This article poses the question: could a neck dysfunction be related to a problem in the lower extremities? The forward head posture is commonly seen in many of our patients. They often present with hypertonus in the upper trapezius and suboccipital muscles. BUT is the neck hypertonicity the primary problem? What if the patient's symptoms are greatly different in sitting vs. standing? If the tension is lessened by sitting (without changing the upper quadrant in any manner), then the patient's symptoms changed simply by altering the position of the lower extremity. The author also states that you must look at other possible causes of neck dysfunction, such as faulty respiration. Potentially the patient breathes differently in sitting vs. standing so the common denominator may not be the lower extremity after all. In all cases, it is extremely important to assess- correct (perform an intervention)- then reassess in order to determine to true origin of a patient's symptoms. Wainner RS, Whitman JM, Cleland JA, Flynn TW. Regional interdependence: a musculoskeletal examination
model whose time has come. The Journal of orthopaedic and sports physical therapy. Nov 2007;37(11):658-660. 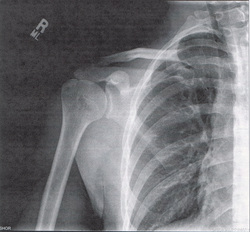 Mike Reinold is back at it again offering a different perspective on scapular exercises. It's standard procedure to include scapular strengthening with our shoulder patients. At almost any clinic, you'll see practitioners prescribing the infamous I, T, Y exercises. Reinold discusses whether or not we should be trying to achieve full symmetry, whether or not we should be performing these exercises bilaterally, and cueing our patients to "pinch your shoulder blades together." Check out his post for a different perspective along with some solutions.
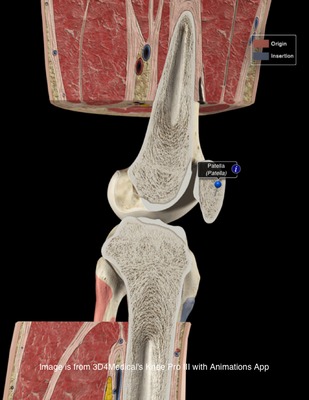
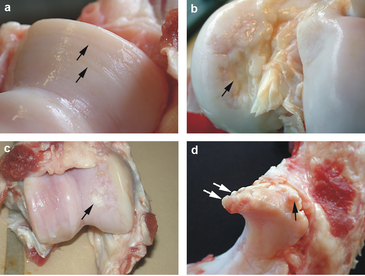
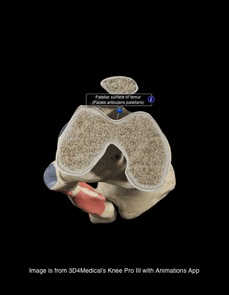 There is a lot of confusion in the health care community about chondromalacia patella (CP). Many practitioners use it simply to identify individuals with anterior knee pain. This can lead to difficulty when researching the evidence regarding CP. Due to the relationship between CP and patellofemoral pain syndrome, many of the treatment methods are similar. This will be explained in further detail later on. Clinical Presentation: Patients with chondromalacia of the patella will often complain of pain with knee flexion and extension, difficulty climbing stairs, crepitus, and pain that increases progressively. The pathology tends to affect women more than men, has an insidious onset, and is usually bilateral. Often there is no specific traumatic injury. These patient's will frequently demonstrate an increased Q-angle and contracture of the lateral retinaculum of the patella. Additionally, patients may present with patella alta (creating increased wear in the lateral part of the patella), increased valgus angle, and femoral condyle hypoplasia, which predispose the individual to changes in the cartilage (Harman, 2003). The patella functions as a mechanical lever for the quadriceps muscle. As knee flexion increases, the compressive force of the patellofemoral joint increases as well, further stressing the joint. Localized pressure at the middle and inferior facets of the patella results when the knee is hyperextended or the knee is flexed beyond 90 degrees. The altered articular cartilage and changes in synovial fluid can create a chronic inflammatory state within the knee joint, which can accelerate the degenerative processes occurring in the knee. One study looked at the pathological process in the development of CP, "The initial lesion was at the matrix of cartilage, the collagen network was disrupted, then proteoglycan was lost. The microenvironment of chondrocytes was changed with degradation of matrix. So the chondrocytes became degenerative and necrosis from superficial to deep layer, then feed back the matrix again. Finally, the total cartilage layer might disappear, and the bone under cartilage might proliferate. At late stage, the cartilage was completely destroyed and had no self-restorative ability" (Ye et. al, 2001). CP can have both acute and chronic causes. Acute chondromalacia is associated with instability, direct trauma and fracture, while chronic chondromalacia is related to subluxation, increased Q angle, quadriceps imbalance, posttraumatic mal-alignment, excessive lateral pressure syndrome, late effects of direct trauma or pressure and PCL injuries (Harman, 2003). Repetitive microtrauma to the patellofemoral joint, external trauma, or sudden increases in leg exercise load/frequency can contribute to chondromalacia (McMullen et. al 1990). More recently, practitioners are looking at core muscle weakness as a potential cause of chrondromalacia in the knee. Decreased hip abductor and hip extensor strength has been shown to create poor pelvic support, decreased femoral internal rotation, and poor valgus positioning. The strength deficits can also create gait abnormalities such as in-toeing and a trendelenburg pattern.  Diagnosis: As stated earlier, chondromalacia is sometimes used by clinicians to identify individuals with anterior knee pain. To develop a true diagnosis of chondromalacia, visual observation of the articular changes on the cartilage must be performed (Brotzman & Wilk, 2003). Dehaven et. al went so far as to say that patients are diagnosed with patellofemoral pain syndrome until visual observation of cartilage degradation occurred. At that point, the diagnosis would be changed to chondromalacia. The change in articular cartilage that occur is "arthritis in it's truest description" (Chevestick 2012). Because the articular cartilage is aneural, the patient's pain reports are always secondary from capsular, synovial or subchondral bone irritation (Gomoll 2006). One study reported that clinical examination for chondromalacia patella is relatively unreliable, which may present an issue for physical therapists. The most common feature is tenderness on palpation of the medial undersurface of the patella. Other signs that are reported are patellar crepitus, a positive apprehension test and effusion and pain on compressing the patella onto the distal femur (Macmull et. al, 2012). It should be noted that none of these signs are highly specific for chonrdomalacia. In fact, there is no correlation at all with the severity are amount of symptoms compared to staging of chondromalacia; therefore symptomatic severity should not be used when determining the need for an arthroscopy (Pihlajamäki HK et. al, 2010). One test that some practitioners choose to use is the Clarke Sign. Doberstein et. al reviewed the validity of the Clarke Sign in identifying individuals with chondromalacia. The test involves the examiner placing his/her 1st webspace of the hand against the superior pole of the patella. The patient is then asked to isometrically contract the quads (the examiner is blocking the patella from moving superiorly at this point). The test is considered positive if the patient is unable to maintain the contraction for >2 seconds due to pain. Unfortunately, this test was found to have low diagnostic accuracy: sensitivity (.391) and specificity (.675). On average the articular hyaline cartilage behind the patella is 3 mm thick, which often gives the appearance of a space when visualized on a radiograph. As the collagen becomes degraded, there is a decrease in sulfated mucopolysaccharides within the ground substance, which can alter the collagen matrix. X-rays can display decreased joint space in individuals with degradation, along with tracking issues of the patellofemoral joint; however, x-rays are basically only able to aid in diagnosis of late stage CP. Standard MRIs are not useful with early stages of chondromalacia as well. In fact, all imaging techniques have low sensitivity for early degeneration, but a MRA is the most sensitive with early stages. Essentially all imaging techniques are able to detect changes in the later stages (Harman 2003). Another study looked at the diagnostic accuracy of 1.0-T MRI for detecting chondromalacia: sensitivity (.60), specificity (.84), PPV (.75), and NPV (.72); however, the authors found sensitivity values .26-1.00 and specificity values .50-.94 when looking at other studies (Pihlajamäki HK et. al 2010). This means there is a lack of consensus on the various methods of MRI techniques and their diagnostic accuracies for detecting chondromalacia.
Conservative Treatment: Patients with chondromalacia of the patella are first directed to physical therapy for conservative management. A primary intervention of conservative treatment is a strict quadriceps strengthening program to help centralize the compressive forces during quadriceps contraction. Gomoll et. al believes placing the patients on a stretching program, emphasizing the quadriceps, hamstrings, and Iliotibial band is an important component. Additionally, they emphasized isometric and short arc closed-chain concentric and eccentric exercises. Isometrics are thought to avoid unusual loading on the defected cartilage. It is important to identify the contributing factors and address them when treating patients with chondromalacia. The McConnell taping technique, which is often used with patellofemoral pain, is a good intervention to help promote proper patellar tracking. The primary goal is to "restore soft tissue balance in the patellofemoral joint (Gomoll 2006)." Patients with knee pain often present with poor strength in the hip and pelvic musculature. Therefore, these muscles should be a focus in treatment, especially the hip lateral rotators and extensors. These muscles can decrease the valgus stress places on the patellofemoral joint, resulting in less stress on the articular surface of the patella. Check out our previous post on treating patellofemoral pain syndrome for exercises that specifically address these impairments! One study looked at static and isokinetic exercises in treating chondromalacia. With static exercises (knee extended), compressive forces of the patellofemoral joint are minimized, because the patella is contacting the supratrochlear fat pad. Therefore, the quadriceps would could be strengthened, while minimizing stress on the knee. With high-speed isokinetic strengthening, the theory is that the surfaces of the joint are moving so fast that "hydroplaning" would occur. Stress would be minimized because the surfaces are moving too quickly. The study found that both static and isokinetic exercises improved several functional outcomes (walking, running, jumping/twisting, overall activity, and stairclimbing); however, no change in pain occurred (McMullen et. al 1990). Yildiz et. al performed a study on the effects of an isokinetic protocol for individuals with chondromalacia as well. The participants experienced improved functional ability, strength and pain following the protocol. Isokinetic exercise may be something to consider in rehabbing your patient. Chondromalacia is a frequent (and likely incorrect) diagnosis in athletes. In one particular study, the effect of a protocol that had 4 phases was reviewed: symptomatic control, progressive resistance exercise program of isometric quadriceps and isotonic hamstring exercises, a graduated running program, and a maintenance program. To decrease symptoms, the patients would stop activities that aggravate symptoms and take salicylates regularly. The progressive resistance exercises included isometric quad exercises and isotonic hamstring exercises. These were performed 3 sets of 10, 5-6 days/wk. The running program was begun once the symptoms were controlled and the patient could lift 30 lb with quads. Initially, jogging was all that was permitted. As the patient progressed in quadriceps weight levels, so did the running style increase: 30 lb - jogging, 35-40 lb - half speed, 40-50 lb - three quarter speed, 60 lb - full speed/cutting. The final phase involves unrestricted activity, continued use of the progressive resistance exercise program at least 2-3 days/wk, and other adjunctive measures like knee pads, patellar braces, and shoe orthotics (Dehaven et. al, 1979). The program was found to be successful in 82% of the patients. There is often debate about the choice between open and closed-chain exercises for treating knee disorders. One study looked at the benefits of each method for chondromalacia; however, the authors identified chondromalacia as "anterior knee pain," so the participants did not truly have chondromalacia (big surprise). The CKC group performed partial squats, whle the OCK group performed SLR. Each group performed their exercises 20x, twice every day for 3 weeks. Every 2 days, an additional 5 reps would be performed. The results found both groups improved upon pain, but the CKC group had significantly greater improvements in thigh circumference, Q-angle, crepitus, and muscle force (Bakhtiary & Fatemi, 2008). Some potential adjuncts to exercise may include utilization of NSAIDs, injections, and warming needling. If the chondromalacia is not complex, NSAID's have been shown to be beneficial. The more degradation that has occurred in the cartilage, the more invasive treatment becomes. Typically patients with more complex chondromalacia are given a viscosupplementation injection to help increase viscosity and lubrication within the knee joint. Dry needling is becoming a more prominent treatment option for many pain disorders. The theory is that with application of needles, endorphins in the CSF and serotonin in the peripheral blood have increased levels, leading to an analgesic effect. Ling et. al found that warming needling combined with rehabilitation training was more effective in reducing long-term pain than rehabilitation training plus NSAIDs. Surgical Management: When conservative measures fail, surgery is typically the next course of action. The surgical procedure is dependent upon the stage of chondral disease with which the client presents. If the patient has patellar tilt (Outerbridge Level I or II*) The goal of this surgical operation is to restore proper tracking of the patella. Another common surgical procedure is a tibial tubercle osteotomy. The osteotomy attempts to normalize the tibial tubercle to trochlear groove distance. By achieving this, normal congruency is achieved at the patellofemoral joint and less contact stress is induced. One study looked at the effects of arthroscopic debridement for chondromalacia grades III & IV (Outerbridge levels). The treatment involved shaving the remaining cartilage until bleeding bone was reached. Additionally, all the joints were lavaged, and intra-articular debris was removed; this included partial meniscectomies. Following surgery, patients would assume partial weight-bearing on crutches for 5 days before being progressed to full weightbearing. The authors were unable to provide any true indications for when arthroscopic debridement should be performed in grade III & IV chondromalacia, but they still believe it is indicated for certain populations to prolong additional surgery (van den Bekerom et. al, 2007). Given the lack of findings, the evidence is questionable. Other surgery techniques you may see include Bone Marrow Stimulation (Microfracture begins the healing process by making perforations in the subchondral bone), Autologous Chondrocyte Implantation, Osteochondral Grafting, and Patellofemoral Prosthetic Arthroplasty (for patients too young for a TKA). Macmull et. al looked at autologous chondrocyte implantation versus matrix-assisted chondrocyte implantation for chondromalacia. The study found that both methods improved patient symptoms and function, but matrix-assisted chondrocyte implantation was more effective (Macmull et. al, 2012). Again, the type of surgery is largely based off the degree of articular cartilage degradation and other biomechanical influences. Regardless of the surgical technique, patients will go through a strict physical rehabilitation process afterward. A potentially overused treatment for chondromalacia (and patellofemoral pain syndrome) is surgical release of the lateral retinacular fibers. In one study, patients with Q angle >20 degrees did not benefit by lateral release as much as patients with normal Q-angle. The theory is that lateral retinacular fiber release can decrease some of the lateral tracking forces of the patella. Additionally, severing the nerve endings in the internal retinaculum may explain some of the analgesic effects (Vaatainen et. al, 1994). Another study found lateral retinacular release to be as effective as lavage and may be appropriate for patients with patella decentration 5-10 mm and appropriate pain symptoms (Kruger et. al, 2002). Given the conflicting findings, lateral retinacular release should not be an initial course of action. *Outerbridge Classification is used to grade amount of articular cartilage arthritis. (Chevestick 2012) Grade 0: Normal Cartilage Grade 1: Cartilage with softening and swelling Grade 2: Partial Thickness defect with fissures on the surface that do not reach subchondral bone or exceed 1.5 cm in diameter Grade 3: Fissuring to the level of subchondral bone in an area with an area >1.5 cm in diameter Grade 4: Exposed subchondral bone. References:
Bakhtiary AH, Fatemi E. "Open versus closed kinetic chain exercises for patellar chondromalacia." Br J Sports Med. 2008 Feb;42(2):99-102. Web. 9 Nov 2012. Brotzman, S., & Wilk, K. Clinical Orthopaedic Rehabilitation. 2nd ed. Philadelphia: Mosby, 2003. 320. Print. Chevestick, A, et al. "Anterior knee pain: the pitfalls of plica and chondromalacia patellae." Advance Newsmagazines. 2.6 (2012). Web. 7 Nov. 2012. Dehaven K, Dolan W, & Mayer P. "Chondromalacia patellae in athletes: Clinical presentation and conservative management." Am J Sports Med. 1979 Jan-Feb;7(1):5-11. Web. 8 Nov 2012. Dehaven KE, Dolan WA, Mayer PJ. "Chondromalacia patellae and the painful knee." Am Fam Physician. 1980 Jan;21(1):117-24. Web. 9 Nov 2012. Doberstein ST, Romeyn RL, Reineke DM. "The diagnostic value of the Clarke sign in assessing chondromalacia patella." J Athl Train. 2008 Apr-Jun;43(2):190-6. Web. 9 Nov 2012. Gomoll, Adreas, et al. "Treatment of Chondral Defects in the patellofemoral joint." Journal of Knee Surgery. 19.4 (2006). Web. 7 Nov. 2012. Harman, Mustafa, et al. "MR Arthrography in chondromalacia patellae diagnosis on a low field open magnet system." Journal of Clinical Imaging. 27 (2003). Web. 8 Nov. 2012. Krüger T, Göbel F, Huschenbett A, Hein W. "Significance of lateral release in the therapy of patellar chondromalacia." Zentralbl Chir. 2002 Oct;127(10):900-4. Web. 9 Nov 2012. Ling Q, Min Z, Ji Z, Le-nv G, Da-wei C, Jun L, Jia-yi S, Ling W, Jin-yan Y, Le-ping H, & Yang B. "Chondromalacia Patellae Treated by Warming Needle and Rehabilitation Training." Journal of Traditional Chinese Medicine. June 2009; 29: 90-94. Web. 8 Nov. 2012. Macmull S, Jaiswal PK, Bentley G, Skinner JA, Carrington RW, Briggs TW. "The role of autologous chondrocyte implantation in the treatment of symptomatic chondromalacia patellae." Int Orthop. 2012 Jul;36(7):1371-7. Web. 9 Nov 2012. McMullen W, Roncarati A, Koval P. "Static and Isokinetic Treatments of Chondromalacia Patella: A Comparative Investigation." JOSPT. Dec 1990. 12:6: 256-265. Web. 8 Nov 2012. Murphy E, FitzGerald O, Saxne T, Bresnihan B. "Increased serum cartilage oligomeric matrix protein levels and decreased patellar bone mineral density in patients with chondromalacia patellae." Ann Rheum Dis. 2002 Nov;61(11):981-5. Web. 9 Nov 2012. Pihlajamäki HK, Kuikka PI, Leppänen VV, Kiuru MJ, Mattila VM. "Reliability of clinical findings and magnetic resonance imaging for the diagnosis of chondromalacia patellae." J Bone Joint Surg Am. 2010 Apr;92(4):927-34. Web. 9 Nov 2012. Salehi I, Khazaeli S, Hatami P, Malekpour M. "Bone density in patients with chondromalacia patella." Rheumatol Int. 2010 Jun;30(8):1137-8. Web. 9 Nov 2012. Vaatainen U, Kiviranta I, Jaroma H, Airaksinen O. "Lateral Release in Chondromalacia Patellae Using Clinical, Radiologic, Electromygraphic, and Muscle Force Testing Evaluation." Arch Phys Med Rehabil. 1994 Oct;75(10):1127-31. Web. 8 Nov. 2012. van den Bekerom M, Patt T, Rutten S, Raven E, van de Vis H, & Albers G. "Arthroscopic Debridement for Grade III and IV Chondromalacia of the Knee in Patients Older Than 60 Years." J Knee Surg. 2007; 20: 271-276. Web. 8 Nov. 2012. Ye QB, Wu ZH, Wang YP, Lin J, Qiu GX. "Preliminary investigation on the pathogeny, diagnosis and treatment of chondromalacia patella." Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2001 Apr;23(2):181-3. Web. 9 Nov 2012. Yildiz Y, Aydin T, Sekir U, Cetin C, Ors F, Alp Kalyon T. "Relation between isokinetic muscle strength and functional capacity in recreational athletes with chondromalacia patellae." Br J Sports Med. 2003 Dec;37(6):475-9. Web. 9 Nov 2012.  A novice clinicians, we often struggle gathering a thorough Subjective History. Even if we obtain the necessary information, we might not always apply the information properly. This post comes to you from The Manual Therapist.com. He discusses 5 key reasons why the patient's history is so important. 1) The patient will tell you what makes them better and what makes them worse 2) The patient will describe the behavior of their symptoms 3) The patient will describe the location of their symptoms 4) They will mention old surgeries and previous injuries to the area 5) A good history will find any red flags that will affect your treatment. Being able to identify this information will make your physical examination, goal setting, and intervention selection much easier! |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|








 RSS Feed
RSS Feed