- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
As many of you know, we recently launched a Home Exercise Portion to our website. They consist of many exercises that we prescribe and programs like VHI don't contain. I wanted to highlight one exercise today, the Quad Rock Back, because of all of uses for it. The exercise is a staple of the Shirley Sahrmann philosophy. While it is listed under the "Low Back" section, it is often prescribed for cervical, shoulder, and hip patients as well. We will break down how the exercise can be used for each region. As described in the video, when this exercise is performed for cervical patients, often the head begins to extend or flex while rocking back. This is a result of abnormal movement and compensatory patterns in the cervical spine. For cervical spine patients, we encourage a chin tuck so that no neck movement occurs during the rocking.
There are many reasons why I like to give this exercise to shoulder and hip patients, one being joint compression. We are taught in our manual therapy classes that joint compression can be beneficial for healing; it also can help mobilize the posterior capsule. It also helps mimic the developmental patterns of weight bearing on the upper extremities, and thus is a critical part of rehabilitation. Additionally, the quad rock back exercise can be use to help normalize scapulohumeral movement patterns and avoid any compensatory activity. While performing the exercise, the movement can be completed by actively flexing the hips, instead of pushing away with the UE's. This allows the shoulder to move in a more normal pattern. Similarly, the exercise can help with unwanted hip musculature activity. By reversing the directions (instructing the patient to push with the hands and not actively flex the hips), the patient can decrease abnormal femoral head sliding and thus compete hip flexion less painfully. The exercise can be used both for treating and assessing and low back dysfunctions, and not just because it is one of the more comfortable positions for low back pain. If you take your patient into quadruped and have them rock back, pay attention to the pelvis, hips, and low back. You may note a deviation to one side, suggesting increased muscle activity, stiffness, or movement patterns. Often you will note premature lumbar flexion compared to end-range hip flexion. This is secondary to all the sitting we do throughout the day - our lumbar spine becomes more flexible compared to the hip! By encouraging the patient to maintain a stable lumbar spine while rocking back (this can be done by placing a stick across the low back - if it falls off, we know there has been abnormal movement). This teaches our patients to isolate hip movement from back movement. While I may not subscribe to all of Sahrmann's theories on movement impairment syndromes, especially in the acute phase, I do appreciate the focus she places on changing compensatory patterns with her exercises. Many of these patterns stem from abnormal postures or repetitive tasks that we perform throughout our daily lives. The rehab focuses on resisting any changes in movement that occur as a result. I have found that I get better results with incorporating repeated motions into my treatment, but I continued to use Sahrmann exercises to try and retrain movement afterwords. -Chris
1 Comment
A couple months ago, I subscribed to the premium portion of The Manual Therapist. Dr. E presents a very eclectic approach with various techniques with which I had not been familiar. One of the prime components of Dr. E's assessment and treatment techniques includes repeated loading. While this might be associated with the McKenzie school of thought, his reasoning has more of a neural approach. Since my neck hurt more on one side, I wanted to look for an asymmetry to treat. With cervical retraction and sidebend, both sides were painful, but I was especially limited to the R. Noting the asymmetry, I proceeded to perform repeated motions in the limited direction which resulted in increased range and decreased pain. Part of the theory is that by getting to the end-range repeatedly, we can re-teach the nervous system that it is okay to go in that direction and possibly others. A common saying for McKenzie type exercises is 10 repetitions 6-8 times a day. With Dr. E's approach, the more the motion is performed, the better. This applied to me. I noted the more I did the exercise, the longer I could go without pain and with increased motion. That evening I had my girlfriend do a cervical manipulation and thoracic manipulation which helped my pain, but within 30 minutes, I was back to the prior levels. The next 2 days, I did the cervical retractions and right sidebend 10x every 30 minutes throughout the day (give or take). Each time I did the exercises, I found I could go longer before the pain and stiffness returned. After 48 hours, I was 95% better.
There are two important components I took from this experience. First, repeated loading can be an incredibly useful assessment and treatment technique, when applied properly. With the majority of people being rapid responders, we should get almost immediate changes with pain and/or motion. Secondly, it is frustrating how long we often have to wait for patients to be evaluated due to length of time after referral, lack of awareness of what PT can offer, or other reasons. The sooner patients can access physical therapy, the sooner physical therapy can begin to help patients on the road to recovery. -Chris  General Overview Time and time again, the Occupational Therapists in my clinic get referrals for Carpal Tunnel Syndrome (CTS). In some of these cases, the patients also have cervical pain, shoulder pain, proximal forearm weakness, and/or palmar paresthesias. While these individuals may have compression within the carpal tunnel, many of them are suffering from nerve entrapment proximal to the carpal tunnel. Many develop adverse neural tension caused by postural dysfunctions, muscle imbalances, and systemic comorbidities which cause a breakdown of the nervous system. Am I saying CTS is over-diagnosed? That is exactly what I am saying. It has become a blanket term for pain in the wrist and hand just as lateral epicondylagia has at the elbow. Many times, the cause of someone's symptoms is not consistent with the referring diagnosis. In this mini-review, I will break down a few areas of entrapment of the median nerve and how to assess for adverse neural tension within the median nerve. Median Nerve Pathway The median nerve is formed from contributions of the spinal nerve roots C5-T1. After originating from the brachial plexus in the axilla, the medial nerve travels down the arm to the cubital fossa. Next, the nerve travels through the two heads of the pronator teres and between the flexor digitorum superficialis and flexor digitorum profundus muscles. At this point the median nerve splits into the anterior interosseous nerve (AIN) and palmar cutaneous nerve. Finally, the nerve travels through the carpal tunnel space. (Be aware there are many alternative anatomy presentations; this is simply one of the most common ones). As you can see there are many points of entrapment for the median nerve: the cervical spine, interscalene musculature, between the heads of the pronator teres, and within the carpal tunnel (among other less common ones). The patient's subjective reports and your clinical examination will point you to the correct structure and location of dysfunction. When suspecting neural tension, a clinical examination measure you should utilize is the Median Nerve ULTT. Assessing for Adverse Neural Tension & Different Sites of Entrapment We have discussed adverse neural tension several times before on The Student Physical Therapist (How to assess neural tension, Differential Dx in neural tension). At the Harris Health Orthopedic Residency, I use 3 distinguishing criteria for positive adverse neural tension testing. The symptom(s) must reproduce the patient's primary complaint, it must change by moving a component at a joint proximal or distal to the complaint, and it must be different side to side. To see the full test for adverse neural tension of the median nerve, click HERE. This test will not tell you the exact location of symptoms, but it will give you an understanding of the sensitivity of the nerve. In addition to performing neural tensioning tests, it is important to perform a thorough assessment of other potential areas of entrapment. For example, if you find muscle wasting in the FPL, pronator quadratus, and/or radial half of the FDP, the involved nerve is likely the AIN being compressed in the proximal forearm. Additionally, if the patient has comorbidities that affect the nervous system, such as a history of uncontrolled DM, this can significantly alter your patient presentation. Several clinicians I work with relate this to a form of double crush injury: the nerve is being mechanically entrapped and is also receiving compression from other intrinsic sources. Continue to use your differential diagnosis skills to determine the source of one's symptoms. It may save your patient from an unnecessary surgery. -Jim 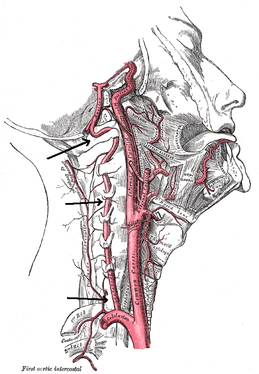 There is a common fear in treating the cervical spine (especially the upper portion) manually due to risk of injury. With the potential for damaging the vertebrobasilar artery system in the cervical spine, many people stray away from performing cervical manipulations. There have been a few situations where patients have died of ischemia following a cervical manipulation. The fatal reaction (and associated risk for lawsuit) to something that we can do as health care practitioners may discourage some from learning how to effectively apply manual therapy to the region. Is there really that much risk to injury? And what can we do to assess it? As with any fatalities in the health care system, media (and other professional disciplines) will try to make the public aware of the risk for injury following a treatment. The same case applies to cervical manipulations. Some people have a somewhat irrational fear of this technique following media coverage and word of mouth. But how much risk is there really? NSAIDS have a .0004% annual mortality rate (Vizniak 2015). There is a .00005% chance of dying from a lightning strike each year. With cervical manipulations, there is a .00002% risk of death. This means you are more likely to die from taking NSAIDS or being struck by lightning than a cervical manipulation. That being said, it is essential that proper patient selection is done before even considering this type of treatment technique. Start with patient history. Any patient with ligament laxity, rheumatoid arthritis, long-term corticosteroid use, osteoporosis/-penia, Down's Syndrome, osteoarthritis, and VBI be excluded. Naturally, we should perform our structural integrity tests and blood flow tests. We recently completed a review of the upper cervical spine that may prove beneficial reading as well. The structural integrity tests should at least include Transverse Ligament Test (and/or Sharp Purser Test), Alar Ligament Test, and a test for a Jefferson's Fracture. This last test is completed by compressing the transverse processes of the Atlas to assess for integrity. A positive test will occur with lack of stability or reproduction of neural symptoms. The artery test that is commonly performed is for Vertebrobasilar Insufficiency (VBI). While the test we show displays combined end-range motions, some say this is not necessary. With the manipulation techniques staying closer to mid-ranges, some suggest just performing complete rotation when assessing. In theory, combined rotation and extension significantly closes off the vertebral arteries greater than rotation alone. Now, the real question is: should we perform the Vertebral Artery Test? A compilation of studies revealed that there is a 0% sensitivity and .67-.90% specificity for the test (Cope et al, 1996). What this tells us is that a negative test means absolutely nothing and a positive test means a patient may have VBI. The testing we perform cannot rule out or rule in VBI. Vertebrobasilar Insufficiency is essential to consider as many of the symptoms mimic other orthopaedic cervical spine conditions: headache, neck pain, etc. (along with more traditional VBI symptoms - see link for symptoms). Even though there is poor diagnostic accuracy associated with the Vertebral Artery Test, it is recommended that the test be performed. There is a traditional thought that the vertebrobasilar artery system be tested prior to any manual therapy, no matter how poor the test is. Due to the media's perception that cervical manipulations risk VBI, any sign of "negligence" by not performing the test would likely place blame on the practitioner. As with any treatment technique, evaluate each patient individually for the potential benefit and associated risk factors prior to performing. In addition to performing the VBI test, Jim and I agree that the therapist should perform a pre-manipulative hold prior to any thrust procedure. The pre-manipulative hold allows the therapist to see how the patient will respond to the manipulative position prior to performing the thrust technique. Finally, we recommend following that process up with a "gut check" as well. Is the risk of the technique worth the reward/ benefit the patient will experience? Not everyone needs or should have a manipulation, but there are some instances where it has been shown to be highly beneficial. -Chris References:
Cote P et al. J Manipulative Physiol Ther. 1996. Vizniak, Nikita. Spinal Manual. Canada: Professional Health Systems, Inc, 2015. 156-157. Print. 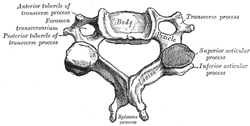 Individuals with mechanical neck pain often have pain and a loss of mobility in the upper cervical spine, specifically at the atlanto-axial (C1-C2) joint. This joint is primarily responsible for cervical rotation, but also contributes to small amounts of flexion and extension. Arthrokinematically, during left rotation, the left facet of the atlas(C1) glides posterior on the axis (C2) & the right facet of the atlas glides anterior. During flexion, the facet of the atlas glides anterior and rolls posterior in relation to the axis. The opposite happens with extension. There are 2 different theories as to how to assess the mobility of C1-C2. At Harris Health, I learned to maximally side bend the head, followed by opposite rotation. For example to assess C1-C2 rotation to the left, maximally side bend the head to the right, followed by maximal rotation to the left. The maximal side bend "locks out" the lower cervical vertebrae allowing for motion only at the C1-C2 junction. The other method to assess C1-C2, which I learned in PT school at St. Louis University, is the flexion- rotation test. To perform this test, maximally flex the cervical spine followed by maximal rotation either left or right. Flexion is thought to lock out all vertebrae below allowing for rotation at C1-C2 only. The difficulty with the flexion-rotation test is maintaining flexion while maximally rotating the upper cervical spine. From my experience, there is a tendency to lose upper cervical flexion. In the residency, I learned that the flexion-rotation test assesses C1-C3. One can then differenciate C1-C2 restrictions from C2-C3 restrictions by first performing the side bend rotation test first, then performing the flexion rotation test. If greater rotation is achieved during the flexion-rotation test vs. the sidebend then rotation, it can be assumed the dysfunction is greater at C1-C2 joint.
It is important to understand that different programs teach different methods of assessment. One method is not better than the next as long as there is sound reasoning behind your decision making. Does anyone else assess C1-C2 differently or have preference with one method over the other? Let us know! -Jim Thank you to the Harris Health Orthopedic Residency for letting me use images from their Cervicothoracic Module Workbook.  Last Tuesday I performed an evaluation on a traumatic C7 Disc Herniation. The 29 year old male presented with neck pain, medial scapular pain, and decreased function of the triceps muscle. This is the first traumatic cervical disc herniation patient I have treated and I thought I would do some research on the topic prior to his 2nd visit. It should be noted that traumatic is different from degenerative disc herniations, a component of DDD, which are present in "30-70% of all adults...as seen on Magnetic Resonance Imaging." As many people know, traumatic cervical disc herniations are seen much less frequently than lumbar disc herniations. This is primarily due to less load bearing requirements of the C-spine, but also in part due to the physiological construct of the cervical disc. The annulus fibrosis, outer ring of the disc, is discontinuous and "does not have complete concentric rings that surround the nucleus." (Neumann 2010) Cervical discs herniate either posterior or posterolateral. They do not typically herniate purely lateral due the uncinate processes blocking this motion. When the disc herniates, it may result in compression of the spinal cord or "radiculopathy, marked by compression and inflammation of the cervical nerve root." With a posterolateral herniation, symptoms include either sharp or dull pain down the medial border of the scapula with radicular symptoms present in a dermatomal pattern of the suspected nerve root. In certain cases, "numbness or tingling may also replace pain as the primary presentation." (Yeung 2012) A physical examination can guide you to a diagnosis, but the best diagnostic test to confirm a disc herniation is a MRI. Treatment of cervical disc herniations is a multimodal approach. Currently there is not a great deal of research regarding treatment options. I plan to treat this individual similar to a cervical radiculopathy patient. I will be using a cervical unloading device while performing active strengthening exercises and the appropriate manual therapy techniques. Additionally, I will be address scapular strength, nerve tension, and postural deficits that were found during the evaluation. More to come, -Jim References: Neumann, Donald A. Kinesiology of the Musculoskeletal System: Foundations for Physical Rehabilitation. St. Louis: Mosby, 2010. Print.
Yeung, Jacky T., John I. Johnson, and Aftab S. Karim. "Cervical Disc Herniation Presenting with Neck Pain and Contralateral Symptoms: A Case Report." Journal of Medical Case Reports 6.1 (2012): 166. Web.  This study was released in the March 2013 edition of JOSPT. Anyone who has worked in a physical therapy clinic understands that neck pain is a very common problem. Researchers estimate that as many as 1 in 4 patients in an outpatient PT clinic are referred for neck pain. This specific study by Masaracchio et al assessed the short-term (1 week follow up) effects of adding thoracic spine thrust manipulation in addition to cervical spine Grade III non-thrust P-A mobilizations. 66 participants were randomly selected to either the experimental or control group. Subjects were excluded if they had symptoms distal to the shoulder, pain for >3 months, or a Neck Disability Index score <20%. The subjects in the experimental group who received both the thoracic spine and cervical spine manual therapy had statistically significant changes in their pain as indicated by decreased scores on the Numeric Pain Rating Scale and significantly lower scores on the Neck Disability Index. These results add to the body of literature suggesting the benefits of manual therapy in patients with mechanical neck pain. Different theories exist as to why the thoracic spine manipulation group showed greater improvements. First, there is a clear biomechanical link between the C-spine and T-spine. By moving the thoracic spine, the cervical spine pain generators experience decrease stress. Another explanation discusses changes in mechanoreceptor sensitivity when a thoracic spine thrust manipulation is performed. While thoracic spine manipulation may not have high specificity, several studies have demonstrated that "regardless of the manual therapy intervention chosen, individuals experienced a reduction in pain levels following manual therapy interventions." Some people may argue that this study only assessed patients at 1-week follow up, and it did not investigate long term reductions in pain. With that said, by having the capability to significantly reduce a patients pain in 1-weeks time, you have much more freedom with your intervention selection. Lowering the significance of pain and disability will greatly improve patient satisfaction, patient buy-in, and your ability to prescribe the necessary exercises. To view the full article click here. References:
Masaracchio M, Cleland JA, Hellman M, Hagins M. (2013). Short-Term combined effects of Thoracic spine thrust Manipulation and Cervical spine nonthrust Manipulation in Individuals with Mechanical Neck pan: A Randomized control trial..JOSPT. 2013 March; 43(3): 118-127. Web. 20 September 2013.
 While the thoracic spine is often not the source of a patient's symptoms, decreased mobility in this region can create problems up and down the chain. For example, in his book Movement, Gray Cook discusses the importance of thoracic mobility when assessing scapular stability. Additionally, mobility of the ribs, breathing pattern, and referred pain from the cervical spine must all be considered when working with the thoracic spine. In this post from Dr. E, he discusses several innovative techniques to mobilize the thoracic spine. Below is a direct link to the video.  In the previous post, we discussed a clinical prediction rule for patients presenting with neck pain who would benefit from thoracic manipulation. We would like to clarify that the CPR only provides the ability to a priori identify individuals who would likely have early success after being treated with thoracic spine manipulation. A priori is defined as reasoning that proceeds from theoretical deduction rather than experience or observation. Cleland et al stated in their original article that further studies needed to be performed in order to validate this CPR. A follow-up study found that this CPR did not prove valid. However, Cleland et al did point out that while the CPR lost validity, patients with mechanical neck pain who were treated with thoracic spine manipulation had significantly greater improvements in short and long term disability (based off the Neck Disability Index). Additionally, these individuals had less pain at 1-week follow up compared with individuals who only received exercise. In conclusion, the CPR for patients presenting with neck pain who would benefit from thoracic manipulation was not validated. As clinicians, still be cognizant that thoracic manipulation can improve your patient's neck pain and disability status. While the 6 predictive variables of the CPR cannot be used in isolation, the importance of these factors should still be documented to help guide your differential diagnosis. A quick thank you to Steve who brought this information to our attention! Neck Disability Index criteria for scoring can be found HERE. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|












 RSS Feed
RSS Feed