- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
 The Manual Therapist recently had a post regarding the usefulness of isometric exercises. Some research discussed in the article has shown immediate and significant pain relief after isometric contractions. The article is directed more towards "tendon" pain, but the usefulness likely extends beyond it. With the developments in pain science, we recognize that pain is more of a perception and has a significant contributing factor of fear. With isometric contraction, we can introduce muscle activity is as less threatening way, allowing the individual to decrease their fear avoidance behavior. Additionally, I like to utilize low level isometrics to help stimulate blood flow in post-surgical patients when permitted. -Chris Like this post? For more advanced information, join the Insider Access Page now! Also, check out similar previous posts below:
0 Comments
 In school, physical therapy students learn to find many impairments. Some are important and others may be irrelevant. They often find six or seven impairments and start treating them all during a single session. For example, a patient with glenohumeral joint dysfunction will likely have shoulder range of motion deficits, scapular strength deficits, 1st and/or 2nd rib dysfunction, thoracic and CTJ dysfunction and more. Ranking the importance of these impairments is difficult. Where should the clinician start their treatment? Knowing what region to address first is a difficult task. There is not one answer because each case is different. Generally, I work from the spine outward and proximal to distal. In the shoulder example above, I would treat the thoracic spine and CT junction prior to treating the glenohumeral range of motion deficits. I would strengthen the scapular muscles prior to addressing shoulder muscle strength. Regardless, I want to focus on one or two impairments per treatment session. Novice clinicians attempt to treat every impairment during each treatment session. This treatment method gives a small dose of treatment to several regions of the body. This is largely ineffective. My recommendation: Choose a SINGLE impairment goal for each patient and fix that one goal. In the shoulder example above, my primary goal would be to fix thoracic spine mobility. I would focus my entire treatment session on thoracic spine mobility and range of motion exercises. Of course I would want to sustain the mobility changes with scapular neuromuscular reeducation exercises, but only after the mobility has been achieved. This method simplifies the entire session. Instead of focusing on which impairment one should treat next, think about what exercise or treatment one can use to treat the primary impairment. Addressing impairment #1, often corrects problems two, three, and four. Jim Like this post? Check out our Insider Access Page. Want to make a Guest Post? Check out our current guest postings including this one on the Asterisk Sign.
This post is an introduction to the topic, and if it generates enough interest, I can expound more on the current topics and further discuss the art of this subject as well. Definition: Test, treat, re-test is executed by the PT performing a simple, reproducible, reliable test with a patient. The PT will then perform one or more treatments. The PT will then perform the same test. READ MORE  One of the foundations of physical therapy is exercise. We are trained to examine patients, find their impairments, and treat them with manual therapy, exercise, and education. Because of this, some view physical therapists as exercise specialists, which is a topic worthy of debate itself. There are several different schools of thought with exercise, primarily in regards to technique. Some focus on gross, functional movements, while others are very precise with corrections of movement impairment syndromes. Where it often gets difficult is with older, deconditioned patients. Some believe that these patients "just need to get moving." They are weak throughout, so any muscle stimulation is beneficial. It is easy to understand why many fall into this thought process, with less active individuals. Personally, I believe it is essential to correct the form for everyone for several reasons. One, when patients move, they generally choose the path of least resistance, meaning the muscles that are strongest or have preferred activation will be the prime movers. Think of a patient doing squats, but you observe the knees flying past the toes. There could be several mobility, strength, and motor control issues leading to this movement pattern, which leads to increased risk of injury. Second, when compensation occurs, the muscle we think we are targeting ends up not being activated as much as we desire. An example would be a sidelying clamshell where a patient's pelvis rocks backward with each repetition. Finally, it is just plain harder, and thus more effective, for the patient. When we correct the form of an exercise, there is an increased likelihood of targeting the desired muscles to improve the functional deficits. What you may have noticed is that all of the above examples are essentially the same. As physical therapists, we should include corrective techniques with all our patients as all will benefit from them. Even with gross strengthening exercises we can identify preferred muscle activation. With some practicing deadlifts or lifting techniques, we cannot allow excessive motion to come from the lumbar spine. The targeted areas are not reached as effectively and the patient's likelihood of injury increases. It is best that we be "picky" when correcting our patients' technique. -Chris Like this post? For more advanced information, join the Insider Access Page now! Also, check out similar previous posts below:
Almost every physical therapy clinic in the country uses cryotherapy (ice packs, ice massage, spray and stretch, etc...) as an intervention for pain management and decreasing inflammation following an acute injury. In theory, these interventions make sense. Cold is a method of vasoconstriction, which will blunt blood flow and reduce swelling to an injured region. However, what other processes are we altering by constricting blood flow? Are there negative effects to icing an acute injury? A New Paradigm for the Use of Cold Inflammation is a natural part of the healing process. With inflammation, inflammatory mediators, leukocytes, and macrophages flood the region. These cells function to clean up and repair the injured area. Additionally, the lymphatic system is designed to eliminate excessive fluid accumulation and the musculoskeletal system uses movement to power the lymphatic system. In other words the body has systems and processes established to eliminate swelling. A study by Meeusen and Lievens found that prolonged icing affected the permeability of the lymphatic channel and increased local swelling. Another experimental study performed on rats found that icing following an acute injury decreased the amount of macrophages and reduced the number of regenerating muscle cells. This post is not intended to convince the reader to avoid using cryotherapy as an intervention, but rather provide a different perspective. There is not strong evidence supporting or refuting the use of ice to decrease inflammation. Understanding both sides of the conversation is important. What do you think? Check out the original post on post/article HERE Like this post? Get exclusive information on our Insider access page  MMT: A neuromuscular perspective A couple weeks ago I was evaluating someone with low back and groin pain. I did my usual systematic examination that included various mobility and strength measurements. I was surprised to find the patient had MMT (Manual Muscle Test) strength of 2+/5 in her gluteus maximus bilaterally. The patient was in her mid-20's, an avid rock climber, and had reported doing clamshells for strengthening regularly. The patient immediately showed a positive response to approximately 20 repetitions of repeated lumbar sideglides. Continue Reading  One of the things we encounter as physical therapists is a need for an eclectic approach. What this means is that we need to have many different methods to accomplish the same goal. Why is that? Often, patients will present with certain restrictions that may limit the effectiveness or safety of another approach. For example, when addressing cervicothoracic junction mobility using joint mobilization/manipulation, we recently posted a video on the Insider Access Page describing 3 manual techniques for this. They included a seated distraction manipulation, a prone chin pivot mobilization/manipulation, or a seated PA mobilization. Some patients will not be able to tolerate all these techniques. A patient with shoulder pain/instability would have difficulty with the seated distraction manipulation. A patient with TMJ dysfunction could not tolerate the prone chin pivot technique. Not every technique is appropriate for every patient. Another reason for knowing a multitude of methods for treatment includes the case where not every patient will respond as well to the same technique. I recently had a patient who I had regularly performed distraction manipulations, repeated motions, dry needling, IASTM, and mobilizations in OKC and CKC to improve talocrural mobility. While there was some progress, the results were limited compared to what was expected. I consulted another PT with two additional techniques I was unfamiliar with in order to trial them on my patient (soon to be shown on Insider Access!). He immediately displayed significant improvements in mobility and pain. This is a perfect example of why we should continue to learn as many treatment techniques as possible. Not all patients will respond as significantly with the same technique. -Chris Like this post? For more advanced information, join the Insider Access Page now! Also, check out similar previous posts below:
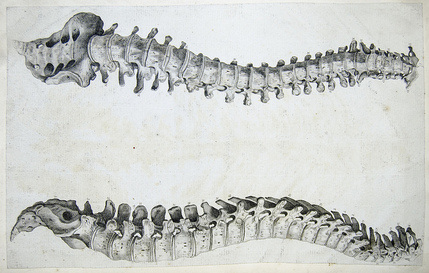
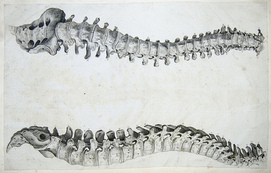
 In my fellowship course this weekend, the instructors were discussing the role of the multifidi muscles in relation to low back pain. During the conversation they stated that while pain often decreases acutely, the muscles remain atrophied if not specifically trained. They cited articles from Hides et al (1996, 2001) who found that individuals with specific multifidi training had reduced recurrences of low back pain 3 years after initial onset. To review, the multifidi are the most medial and largest muscles of the low back. They run the entire length of the spine and play a vital role in protecting the low back. The main function of these muscles is to oppose the abdominal muscles as they produce rotation (not produce rotation as commonly thought). Why does this matter? In the initial stages of treatment, use your standard low back interventions (repeated movements, spinal manipulation, dry needling). These interventions help decrease pain, decreased fear avoidance, improve mobility, and more. Once the individual's pain has decreased, incorporate core strengthening and movement pattern re-education to ensure these muscles are properly supporting spine to prevent recurrence of symptoms. While many of us do a great job treating the acute pain, are we appropriately managing the problem from reoccurring? -Jim Like this post? Check out our Insider Access page for more exclusive information!  Neural Tension vs. Muscle Strain? As many of you know, I have written about cases several times in the past about examining and treating chronic "strains." In the outpatient setting, odds are you will frequently be presented with cases where the patient reports straining a muscle months/years ago and never fully recovering. Continue Reading  A few weeks ago, a student introduced me to the topic of DermoNeuroModulation. It's a concept that brings to light the importance of peripheral cutaneous nerves. Much of what Butler's current work on pain science surrounds involves thorough examination of the nervous system. While Butler's practice focuses primarily on the larger nerves, he does show the ability to stress the smaller superficial nerves as well. DermoNeuroModulation claims that we can use these superficial cutaneous nerves to alter our patient's pain perception and function. A couple years ago, I took a course on IASTM (Instrument Assisted Soft Tissue Mobilization). The mechanism through which IASTM was claimed to have worked was stimulation of peripheral nerves and altering the perception in the CNS. After looking at some of the information surrounding DermoNeuroModulation, likely we are affecting our patients via this mechanism, but with other techniques. Think about the function of IASTM, STM, trigger point release, etc. All are able to stimulate these nerves in theory and all can show success. Like many other theories, little substantial evidence has been found thus far, but in continuing research in the area, we may better be able to implement the proper treatment techniques. What have your experiences been with DermoNeuroModulation? -Chris Like this post? For more advanced information, join the Insider Access Page now! Also, check out similar previous posts below:
 The other day my boss and I were discussing the usage of aerobic machines (total gym, bike, UBE) in our treatment sessions. Prior to attending the Harris Health Residency and my manual therapy fellowship, I viewed these machines as “fillers” in patient care. The machines were an easy place to stick a patient when I was busy. Ironically, after going through these advanced training courses, I use these machines more than ever BUT for different reasons. Collagen is the principle component of most connective tissue (ligaments, tendons, fascia, joint capsules). After an injury, the normal collagen matrix is disrupted. Evidence shows that this collagen is remodeled by continuous motion, blood supply and oxygen, vitamin C, and protein intake. For example, the inner 2/3’s of the meniscus has poor blood supply. To heal a meniscal lesion, those collagen fibers need 1000’s of repetitions. The leg bike or total gym (on a low level) are the best ways to target those fibers. The same principle applies to the glenoid labrum and the upper extremity ergometer. These tissues needed to be trained at ~15% of 1 RM to allow for proper fluid exchange and healing to occur. Sometimes the warm-up seems meaningless for our patients, but with the proper education and instruction, we can teach them the importance of these long duration interventions. -Jim Like this post? Check out our Insider Access page for more exclusive information.
 I recently presented an interesting case to my fellowship class. On 4/3/15 the patient presented to my PT clinic with L medial scapular border and L cervical pain with N&T along radial border of L forearm. The patient was a 45 year old female. The symptoms were intermittent symptoms and began 4 months prior with insidious onset. Symptoms were increased by sleeping, prolonged sitting, and having her L arm unsupported. Symptoms were improved with arm support and being active. Pain intensity was described as dull and was 2/10 at the time of the evaluation on NPRS and 6/10 at its worst. Patient denied any N&V, fever, significant changes in weight in last 6 months, B&B problems, and S&S of cauda equina syndrome. Patient’s job requires prolonged sitting at a computer, with turning her head to the L frequently. Patient also has to fly across the country every week for work. Patient denied any significant PMHx, past surgical history, and taking any medications. CONTINUE READING... Like this post? For more advanced information, join the Insider Access Page now! Also, check out similar previous posts below:
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|












 RSS Feed
RSS Feed