- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
One of the methods of examination that physical therapists is goniometry. It is an essential course taught as a foundational skill in school where a device (goniometer) is used to measure joint range of motion (ROM). There are additional methods of ROM measurement used as well (some more reliable than others), such as tape measure, double inclinometers, selective functional movement assessment (SFMA), percentages, etc. While there is plenty of debate about the usefulness of goniometry, I want to instead focus on discussing how to perform goniometry. While there are several ROM texts out there, the majority of them advocate for using a 3-point system when using a goniometer. The method includes picking one point on each axis and centering the fulcrum over the joint. While maintaining those points, the joint is moved to the desired range. In theory this method should work without fail, however, due to the difficulty of maintaining these points, I recommend the 4-point system, which instead you maintain 2 points along each axis without focusing excessively on the fulcrum. That is not to say it should be ignored, but the fulcrum instead should just hover around the joint. The reason why is that when you use a 3-point system, for certain joints it is extremely difficult to maintain those exact 3 points. Inevitably, the fulcrum gets moved somewhere away from its point of origin and if you try and stabilize with one hand, one of the arms of the goniometer deviates from its starting point. By using the 4-point system, you can use one hand on each arm to stabilize the arm against its respective 2 points while moving the joint. In my opinion, it is far easier and far more accurate. Now I am not saying that the goniometer is the best tool for measurement. It is inaccurate (primarily due to user error) by about +/- 5 degrees each direction. There are certain joints I think that can be better measured with an inclinometer or double inclinometers, like the spine or using a tape measure/ruler for TMJ. Personally, I primarily use the SFMA. I find it is much more accurate to say yes/no by determining whether or not a motion meets certain criteria and it is easier to spot asymmetries. That being said, I still use the goniometer for surgical cases and some other indications, so it is a tool that we need to be as accurate as possible, when used. -Dr. Chris Fox, PT, DPT, OCS
0 Comments
A few weeks ago, I had the opportunity to sit down with Dr. Ryan DeBell from The Movement Fix. During the interview, we discussed everything from movement assessment, to great physical therapy resources, and the relationship between physical therapists and chiropractors. Chiro vs. Physical TherapyIn the United States there is some political controversy regarding which states can perform manipulations; but the conversation should stop there. The fact that people still place a 'vs' in the question is hilarious. Both professions were founded on principles of health and wellness. We all have the same goal of getting people better! As Dr. DeBell states, "if you have time to worry about other people's professions, you need to figure out some stuff to do...go read a book and get better!" From a clinical standpoint, if someone finds another professional a threat to their practice, I suggest looking internally. There are definitely some insecurities that lie beneath the surface. The day we start talking about collaboration over competition will be the day we start placing the patient at the center of care! Movement AssessmentI initially interviewed Dr. DeBell for a new online resource I have been working on, The Movement Corner, so I was curious to see how he performed his evaluations. From a movement perspective, Dr. DeBell utilizes principles of the SFMA, Shirley Sahrmann, Stuart McGill, among a few others. However, I was excited to hear how much he focuses on the biopsychosocial approach to care. When I asked him about his standardized movement assessment, Dr. DeBell initially told a story about looking at the entire person first and foremost. The purpose of the story: not everyone needs a detailed movement examination! Sometimes identifying recent lifestyle changes or environmental factors is more important. As Dana Tew PT, DPT, OCS FAAOMPT, from the OPTIM Manual Therapy Fellowship states, "Don't miss the forest for the trees!" In other words, do not lose site of the entire person and solely focus on the impairments. Suggested ResourcesDuring the interview, Dr. DeBell and I discussed several of our favorite resources and great starting points for clinicians looking to improve their practice. Below the resources are broken down into both professional and personal development. Physical Therapy/Healthcare Books: 1) Stuart McGill: Low Back Disorders (or any book from McGill) 2) Shirley Sahrman Textbook 3) Gray Cook: Movement Life Improvement Books: 1) The Go Giver: A little story about powerful business ideas 2) The Slight Edge: Turning Discipline into Massive Success 3) The Richest Man in Babylon 4) Daily Domination Journal <-- Dr. Ryan DeBell's Product! Watch the Full Interview with Dr. DeBellThank you again Dr. DeBell!
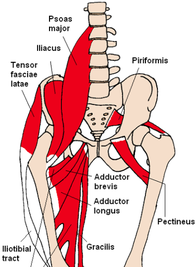
-Jim Heafner PT, DPT, OCS Why We Do a Systems Review One often overlooked but essential component of the examination is the systems review. The systems review is one of several components of our examination that help us to determine if referral or consultation with another practitioner is needed. Unfortunately, many practitioners skip over different parts of the systems review, but picking up a positive finding can lead to better results faster and even potentially saving a life. Check out my post on the Foothills Sports Medicine blog for more information on the topic. -Dr. Chris Fox, PT, DPT, OCS When I started practicing a few years ago, most of my exercise training was based on lower level exercises, like on the treatment table. What I found was that there was a significant gap in my patients discharging and their return to normal activity. As humans, we are active and have to move significant weight to function in our lives. Simply completing some lower level table exercises doesn't help with transitioning back to prior level of function. Thankfully, I learned quickly that I needed to incorporate higher level strengthening exercises to improve my patients' health AND fitness, because in reality they are the same. Coming up in a couple weeks, Michael Mash, PT, DPT at Modern Manual Therapy will be teaching a webinar on how to teach your patients to perform Squats and Deadlifts correctly. I absolutely recommend checking it out. Make sure you register. -Dr. Chris Fox, PT, DPT, OCS BackgroundClamshells are one of the most prescribed exercises for individuals with knee pain. This exercise is intended to target the hip abductors, specifically the gluteus medius muscle. EMG studies have found good activation of both the gluteus medius and gluteus maximus muscles during the clamshell. Additionally, the clamshell has been shown to preferentially activate the gluteus medius while minimizing activity in the tensor fascia latae (TFL).
Common CompensationsWhile the clamshell is intended to have good activation of the gluteal muscles, the exercise will only be as effective as the person instructing the movement. In regards to movement patterns, the body always takes the path of least resistance (i.e. the repetitive, facilitated movement pattern). Individuals who will benefit from performing the clamshell exercise likely have difficulty engaging the gluteus medius. Proper cueing is necessary to avoid compensatory motions.
How to PrescribeThe video below contains a 3-part progression for performing the clamshell exercise. When the client can perform 20-30 repetitions without compensation, I progress to the next level of the exercise. Author: Jim Heafner PT, DPT, OCS
Citations:
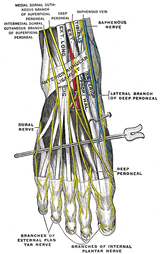
Sahrmann, S. (2002). Diagnosis and treatment of movement impairment syndromes. St. Louis: Mosby. One of the concepts we like to teach at Optim Manual Therapy is developing hypotheses of sources of injury. As soon as you see the script (if you get one) or the location of pain on the intake form, you should immediately have several hypotheses for pain. I recommend at least 5. For example, if someone comes in with lateral ankle/foot pain, my initial hypotheses may include: This list is not all inclusive as there are other potential sources of pain, such as a fracture. Additionally, this list is not mutually exclusive. For example, when someone rolls their ankle, a lot of times they have ligamentous disrution, strain of peroneal tendons, cuboid dysfunction, and intermediate dorsal cutaneous neural tension. Walking abnormally for awhile after injury can then lead to back issues and potentially S1 radiculopathy. Now this is an extreme case, butwe want to be able to narrow down our hypotheses in order to better manage the patient. Following the subjective interview, we should be able to eliminate a couple hypotheses and each remaining one should have some sort of reasoning behind it. Finally, we can use our objective testing to further narrow down our hypotheses to a final PT diagnosis. While we call it final, it doesn't have to be. Sometimes, throughout our treatment, our diagnosis changes based on a patient's response or lack of response to treatment. While we like to challenge our COMT and Fellowship participants to identify possible structures of injury, it is important to remember the involvement of the central nervous system. There are many cases where it is not truly a structural issue and instead we need to focus on retraining the nervous system, especially in chronic pain patients. In these types of patients, it is essential that a non-structural assessment is taken into play and instead is shifted towards a functional assessment. We worry less about pain, other than re-educating the patient on pain science, and more about improving their livelihood and activity. -Dr. Chris Fox, PT, DPT, OCS
One of the most difficult issues about treating patients with chronic pain is that they typically don't respond to manual treatments and exercise the same way more acute injuries do. Those with acute injuries will often have significant changes in pain, mobility and more either within treatment or within a couple days. A patient with pain that is chronic in nature requires a different treatment approach. Education plays an essential role with these patients. With the lack of correlation between pain and structural pathology, part of our role as physical therapists is to make sure our patients do not get dragged into the state of mind that a pathological diagnosis can be assicated with and instead empower them to become aware of the link between various parts of their brain and their pain. Following the initial evaluation, I often give my patients a pain questionnaire to assess their initial beliefs on their condition and prescribe that they watch the 2 videos below in order to initiate discussion at follow up visits. Some additional beneficial resources include the books Explain Pain and Therapeutic Neuroscience Education. -Dr. Chris Fox, PT, DPT, OCS
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|
















 RSS Feed
RSS Feed