- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
This past weekend at the Optim COMT course, we were discussing squats as a form of treatment. While the squat is an excellent exercise for a variety of ailments, it is an exercise that is prone to many compensations. Combine that with pain in the knees or elsewhere, and form may be compromised even more. There are several reasons why the pain may impact the ability to squat, but tissue tension may play a role. One of the common variations that is seen during squats is the "buttwink," otherwise known as posterior pelvic tilt and lumbar flexion. Typically we see this occur as the client nears their bottom depth of the squat. There are many possibilities as to why this may occur: lack of hip flexion, poor motor control, decreased spinal mobility/strength and more. Another possible explanation for lumbar flexion is poor quadriceps strength. As an individual with poor quad strength descends into a squat, they typically either stop early in the depth or display a compensation like lumbar flexion and forward trunk lean. To try and control the movement that the quads are insufficient to support, the body tries to rely on the passive tissue tension of the posterior chain and a shift in center of gravity anteriorly. As the "buttwink" occurs and the trunk shifts forward, the muscles, tendons, and ligaments become taut and provide a form of passive support to control the body during the motion. Over time, this may lead to injury. So how do we fix this? There are many avenues to address this client, but strengthening the lower quarter should absolutely be considered. There are many ways to strengthen the quadriceps, and it may be tempting to avoid squats due to the client's poor form; however, the exercise can be modified to the appropriate level. Using an assistive device like a TRX or leg press can simulate the motion at less than body weight to allow proper form. There are some cases where adding a load to the individual actually improves form! Regardless, improving an individuals functional squat may be as simple as improving their strength. -Dr. Chris Fox, PT, DPT, OCS
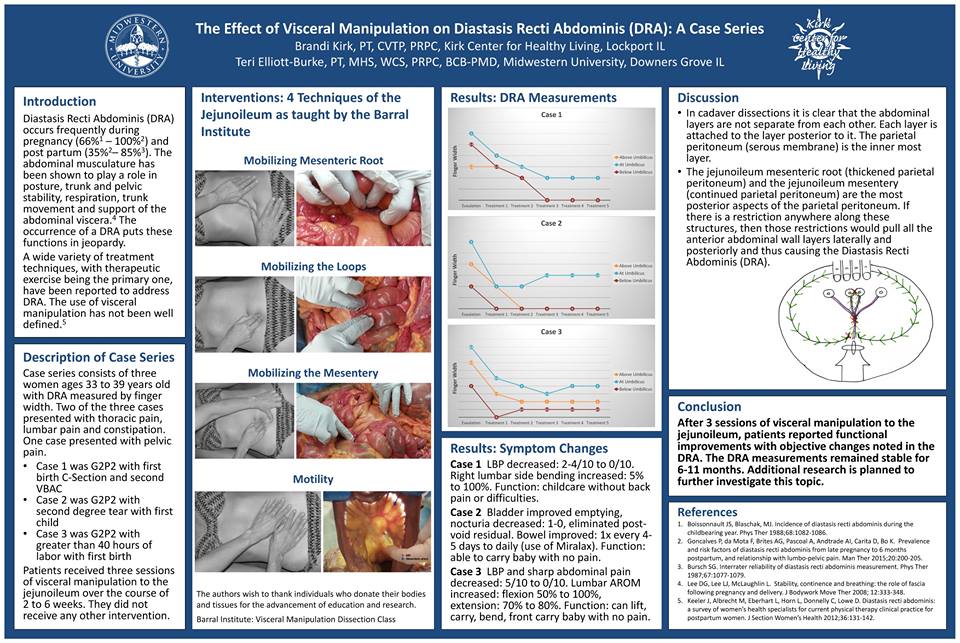
2 Comments
As graduation draws closer, good luck to all those taking the NPTE in a couple weeks. You've put in a lot of work thus far, and the reward awaits you at the other side. Keep at it! Upon starting your practice as a physical therapist, you will inevitably start looking towards what you can do next to improve upon your knowledge base and skills. There are many options out there, whether you are looking for a different perspective, new style of treatment, pain science management or something else, you will never run out of courses to pursue. Upon graduating, I knew I wanted to pursue a residency in orthopaedic. Ideally everyone would complete residency training; however, there aren't nearly enough residencies out there to fulfill the need. A couple years ago Optim Manual Therapy Fellowship was started for situations just like this. We simulate the residency experience at a far more affordable cost, weekend courses, online assignments and weekly mentoring. Our approach is an eclectic one. We look to improve upon typical components, such as anatomy and orthopaedic knowledge, manual skills, and exercise application. However, we differentiate ourselves by the diverse treatment approach and evidence-informed decision making. While we educate our participants on standardized mobility exams, Sahrmann's Movement Impairments Syndromes, and pain science management/education/treatment, our real goal is to help develop your clinical reasoning and facilitate your practice patterns. Below is a sample lecture on Sahrmann's Movement Impairment Syndromes, but check out optimfellowship.com for more information on the program. A new cohort is starting in Dallas in just a couple months, but expect cohorts to begin in St. Louis, Scottsdale and Houston this fall! -Dr. Chris Fox, PT, DPT, OCS This past weekend I went to a course I previously never would have though I would attend: Visceral Manipulation 1 by the Barral Institute. When I first got into PT, my mind was very biomechanical. If there wasn't a mechanical or evidence-supported explanation for how something worked, I didn't think it was worth learning. The more I've practiced and read research developments on pain science I have come to understand that not only does the mind and nervous system play an incredible role in treatment response, but that there is so much out there we don't understand at all. About 2 years ago, my wife was suffering from some pelvic/abdominal pain following her c-section that several doctors and PT's were unable to treat or determine the source. It was at that time she sought a visceral therapist and was back to playing soccer nearly pain-free after 3 sessions. This past summer I had developed the sensation of a lump in my throat (which was later diagnosed as GERD) that at one point was so bad I couldn't breathe while laying supine. It was about 90% improved after just a couple sessions of visceral treatment. These experiences had peaked my interest in at least learning more about the style of treatment. On to the course. Throughout PT school, we are taught all about muscles, bones, ligaments, joints, nerves, etc., but the abdominal cavity is mostly ignored. Sure, we learn about organ function, pathology, and differential diagnosis, but how organs move is never even thought of. While there are certainly concepts that were explained that I am having a hard time wrapping my head around (motility, "listening" as an assessment, and mobilizing organs through ribs), the discussion on affecting mechanoreceptors and proprioceptors through the visceral manipulation is much more acceptable based on current research regarding manual therapy. The biggest "sell" to me was the within class changes that occurred. Yes, we felt improved organ mobility whenever we were finished with a technique, but the bigger changes were seen elsewhere. One clinician with a significant Thomas Test deficit had almost normal motion following mobilization of her cecum. I had a drastic improvement in SLR mobility following mobilization of my sigmoid colon. We saw improved shoulder elevation mobility following liver mobilization. One clinician who had a history of rectocele and cystocele had recreation of labial and rectal pain following a stomach mobilization. One of the aspects of research that is currently being developed by the instructor Brandi Kirk PT, PRPC, CVTP is regarding diastasis recti. She recently presented a case series poster at CSM 2017 on treating the disorder with manipulation of the mesenteric loop, root, and mesentery. In class, one of the clinicians presented with a diastasis recti of 4 finger-widths. After doing just one of the 3 treatments, the next day she had almost complete resolution of the disorder. The research has thus far shown retention a year later with no activity restrictions following discharge. Treatments like this could potentially help many to avoid surgeries. Thankfully the group at Barral Institute is working on developing higher level studies to show the potential benefits of visceral manipulation. Overall, I would say the class is an absolute must-take for every clinician. Visceral manipulation tends to be thought of more as a joke than an actual treatment style, unfortunately. In taking this course, not only am I better able to understand the proposed theory, but also how the successful treatments may be explained by current evidence. My only complaints about the class are that evidence hasn't caught up yet (and they are working on this as we speak!) and that not enough time was given to practice each technique 10 or 20 times (we only practiced each technique once or twice due to how many techniques there were and the complexity of them). Aside from that, the potential for this practice is incredible and changes can not only be seen within treatment but continue for weeks afterwards. While I'm not confident in applying these skills today, with practice, I look forward in implementing this treatment style into my practice and experimenting with further potential. Let me know if you have any specific questions about my experience. I highly recommend this class, as I plan on taking additional visceral manipulation classes in the future. -Dr. Chris Fox, PT, DPT, OCS
With today's research on pain science, we are moving away from pathoanatomical diagnoses. This is a wonderful development as not only does it minimize the fear of pathology in our patients, but it makes our job easier as well. That being said, it can still be easy to be drawn in excessively by the results of special tests, especially in the extremities. This past weekend I performed an evaluation of a middle-aged patient, where the script said "bilateral shoulder impingement." Based on the location of the patient's pain and some positive impingement tests, there may have been "impingement," but anytime I see bilateral symptoms I make sure to assess a central component. I'm not saying this always means the symptoms are driven by the spine, if presenting bilaterally, but that there may be an impairment in the trunk that contributes. In this patient's case, his cervical spine had minimal dysfunction, but his thoracic spine and parascapular musculature were significantly involved. He presented with excessive thoracic kyphosis and weak mid/low traps and serratus anterior bilaterally. His RTC presented with 5/5 strength throughout bilaterally. While there are some deficits in the extremities, the primary dysfunction appears to be located more centrally. In reality, if you are being thorough with your examination and treatment, this shouldn't be a novel concept at all. I always encourage assessing spinal mobility and proximal strength in all my patients. The key then is doing something to address the impairments found. It is not unusual for my foot/ankle patients to be doing lumbar mobility exercises or hip strengthening. We don't always know "why" a patient presented with a form of pain or disability, but we can be sure to address any strength, mobility, biopsychosocial factors with which the patient presents. -Dr. Chris Fox, PT, DPT, OCS
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|













 RSS Feed
RSS Feed