- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
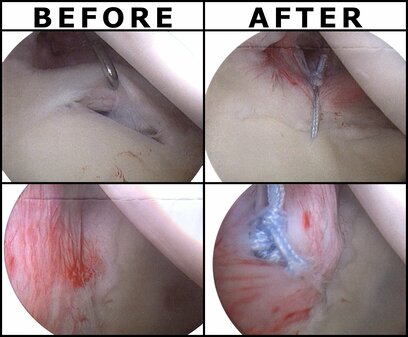
Last week, I woke up one day with severe R anterolateral shoulder pain and inability to raise my arm above shoulder height. In the days preceding, I had completed approximately 8 hours of painting and a heavy shoulder workout, all without pain. Initially, because of the severity of the pain and inability to raise my arm above my shoulder, I became extremely fearful of my inability to fully treat my patients, sleep, or do much of anything with my right arm. Self Exam: Right Shoulder AROM: flexion 80 deg, abd 45 deg, ext 30 deg, IR 45 deg, ER 20 deg R shoulder isometric strength: strong and painless in all directions at 0 deg abd Cervical AROM: full and pain-free in all directions (+) Obrien's Test My shoulder was strong and essentially pain-free when at my side. Treatment: My primary treatment was to limit motion of my RUE to range with minimal discomfort, 5-directional resisted isometrics of the right shoulder at my side, and Quad Rock Back to perform CKC shoulder flexion AAROM. Additionally, I performed repeated shoulder extension with horiz. abduction in CKC between each patient treatment session. I took some anti-inflammatories each day to help encourage movement as well. Over the span of the next few days, my shoulder gradually improved and I got back into some weight-lifting with my focus being legs, posterior shoulder/scapular and some running. Some of the initial testing was positive for labral tear. That plus my significant loss of ROM made my mind start running off into hypotheticals: will I need surgery, how long will I need off work, how can I support my family? As we are all aware from pain science research, these thoughts only serve to raise my pain-level. I had to continually remind myself not to jump to conclusions and to remember people have injuries like this all the time and recover. I'm not sure if the pain was due to RTC syndrome or labral tear or something else, but it shouldn't matter too much due to the lack of correlation between pain and imaging findings. While I am grateful to be nearly fully recovered, the experience was enlightening to me about how various factors can impact a patient's fear and pain experience. It reinforced the importance of addressing all concerns of the patient for an injury, especially the biopsychosocial factors. -Dr. Chris Fox, DPT, OCS
4 Comments
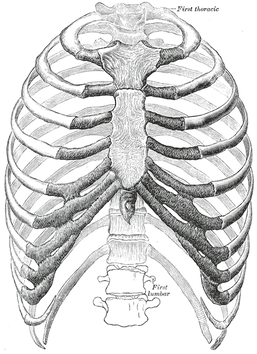
Last weekend, a colleague of mine called me because her husband had severe "rib pain," so I went to take a look at it. Apparently about a week ago he developed pain in his R chest and back but significantly worsened earlier that day when playing basketball with his daughters. The pain was located pin point at sternal end of 3rd rib and some mild pain at vertebral end as well. The pain was constant but had a significant increase with transfers, rolling, and laying on his side. Examination: Cervical AROM had a slight increase in pain with rotation but no change with flexion and extension. Mobility was moderately limited with all motions. Thoracic rotation was mildly painful and BUE myotomal strength was 5/5 throughout. Pinpoint tenderness was noted over the R anterior 3rd rib near the sternal attachment. It "appeared" anterior and hypomobile relative to the surrounding ribs, but testing like this has pretty poor diagnostic capability. Treatment: I did a thoracic, rib and CT junction manipulation. The patient was instructed to do some general thoracic/rib mobility exercises, use various methods to address the pain (OTC pharmaceuticals, heat/ice, gradual increase/resumption in activity). I educated the patient on the fact that injuries like these can be painful initially, but they do get better typically quickly. It's important to stay away from pathoanatomical diagnoses as it can make the patient think they are fragile. While I referred to the case study as "rib dysfunction," I do not and cannot know if the rib was truly involved, even with how abbreviated the examination was. My goal was to lower the threat level by introducing motion to the involved areas. Once the restricted areas were identified, lowering the threat level was done through education, manual therapy and exercise. The key is to guide the patient through the painful experience, by being a resource and assisting self-management for addressing the injury. -Dr. Chris Fox, PT, DPT, OCS
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|






 RSS Feed
RSS Feed