- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
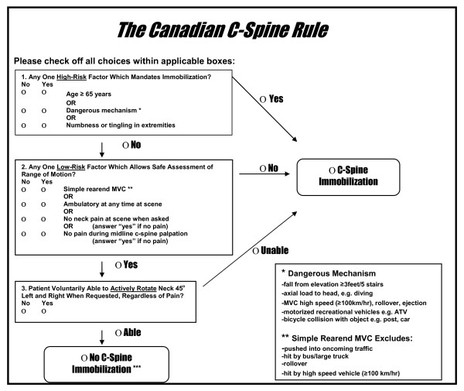
One of the more difficult types of diagnoses to manage in my opinion is neck pain after a motor vehicle accident (MVA). The patient often presents with some form of hypersensitization and a high fear avoidance behavior. This alone makes treatment difficult as the patients typically do not want to do much because "everything hurts." Prior to treating the patient (or even performing certain exam measures), it is essential that you review how the patient matches up with the Canadian Cervical Spine Rules. Check out the flowchart below. Should your patient meet the criteria, they should be referred for x-rays. If your patient doesn't meet the criteria, you can proceed with completing your examination more thoroughly. Treating patients with whiplash can be difficult as 2% of patients will still have significant pain and limitations a year after the accident. What complicates things further is that often there is a delay between the accident and when the patient actually seeks physical therapy treatment. This can be associated with central sensitization. These patients absolutely will benefit from therapeutic neuroscience education (TNE) in order to raise their pain threshold. Over the last year, I have noticed a trend in success with treatment options for patients following an MVA. Initially, I use IASTM (Instrument-Assisted Soft Tissue Mobilization) to the cervical and scapular musculature. This provides a non-threatening stimulus to again re-educate the patient's nervous system about how a normal input should be perceived. Once the patient is about 3 weeks s/p MVA, I typically implement some repeated motions (usually retractions or retractions with extension) hourly. This re-educates the patient's nervous system that end-ranges of cervical AROM can be non-threatening as well when given enough input. It's possible the patient can begin repeated motions earlier or later, but I typically find that patients are too hypersensitive earlier to get to end-range. Manipulations are often used to affect neurodynamics. The issue with patients suffering from whiplash is that their tissues are injured from an overstretch. A manipulation, in some theories, puts a stretch on the tissue as well, so early on may be contra-indicated. I will usually wait until the patient is 6 weeks s/p MVA before I consider performing a manipulation and will start with one directed towards the thoracic spine. Patient also frequently respond to some form of mild traction, so I include a manual component as well. What sort of treatments have you found to be successful with MVA's? Do you utilize manipulations and at what point do you feel it is safe? -Chris
Like this post? Then check out the Insider Access Page for advanced content! And check out similar posts below!
0 Comments
Leave a Reply. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|








 RSS Feed
RSS Feed