- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
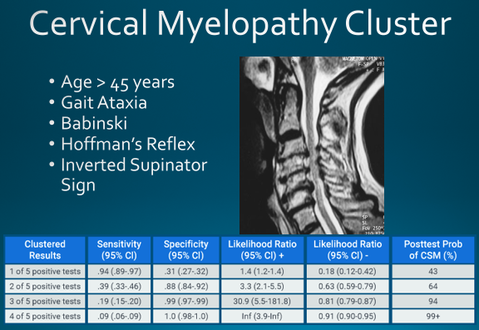
When I was going through Physical Therapy school, I remember struggling with the differential diagnosis of cervical radiculopathy versus cervical myelopathy. I knew both diagnosis' typically cause numbness and tingling, weakness, and sensory loss, but I did not fully comprehend the location of compression or WHY myelopathy had more widespread symptoms. Understanding the difference requires knowledge of cervical spine anatomy, neuroscience, clinical presentation, and more! OverviewChronic cervical degeneration is the most common cause of progressive spinal cord and nerve root compression. In fact, ~70% of asymptomatic people >70 years have degeneration in cervical spine. These spondylotic (arthritic) changes can result in stenosis of the spinal canal, lateral recess, and/or foramina. Stenosis is defined as ANY narrowing of a canal leading to nerve compression. Stenosis can occur centrally, compressing the spinal cord, OR laterally, compressing the nerve root. Chronic cervical degeneration is the most common cause of progressive spinal cord and nerve root compression. Cervical MyelopathyCentral spinal stenosis is known as myelopathy. An individual with myelopathy will present with Upper Motor Neuron signs and symptoms. These symptoms include gait ataxia, a positive Babinski test, a positive Inverted Supinator sign, a positive Hoffman's test, hyperreflexia, potential bowel and bladder changes, among other findings. Since the spinal cord is compressed, a referral for imaging is recommended to assess the amount of compression. Assuming the patient does not have severe compression with hard neurological findings, the patient will likely be appropriate to continue resume their Physical Therapy plan of care. How to Clinically Diagnosis Cervical Myelopathy
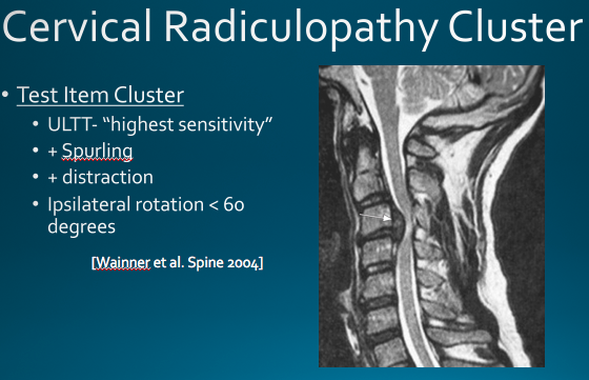
Cervical Myelopathy TreatmentConservative management (PT and anti-inflammatories) has been shown to be beneficial in providing short term relief of symptoms in Cervical Myelopathy. The goals of physical therapy should be symptom management, pain relief, preventing further neurological decline, and maximizing function. Additionally, patients should know that surgical management has not shown superior outcomes vs. conservative management at two year follow-up (1). Cervical RadiculopathyCervical Radiculopathy has significantly different symptoms than myelopathy. In radiculopathy, the nerve root (not the spinal cord) is the involved structure. When the nerve root undergoes compression or tension (any additional stress), individuals will typically have myotomal weakness, sensory loss in a dermatomal pattern, hyporeflexia, positive Spurlings Maneuver, positive Distraction Test, decreased cervical rotation to the involved side, and a positive median nerve tension test. How to Clinically Diagnosis Cervical RadiculopathyMost cases of cervical radiculopathy can be treated conservatively. Cleland et al found favorable treatment outcomes if the patient was <54 years old, a multi-modal treatment approach was used for >50% of the visits, the non-dominant arm was involved, and looking down did not aggravate symptoms. Cervical Radiculopathy TreatmentTSPT now offering a comprehensive Cervical Spine CourseInterested in learning more about the cervical spine?
References:
1. Kadanka Z, Bednarík J, Vohánka S, Vlach O, Stejskal L, Chaloupka R, Filipovicová D, Surelová D, Adamová B, Novotný O, Nemec M, Smrcka V, Urbánek I. Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomised study. Eur Spine J (2000) 9 :538–544 2. Cleland JA, Fritz JM, Whitman JM, et al. Predictors of short-term outcomes in people with a clinical diagnosis of cervical radiculopathy. Phys Ther. 2007;87(12):1619-1632
1 Comment
|
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|






 RSS Feed
RSS Feed