- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
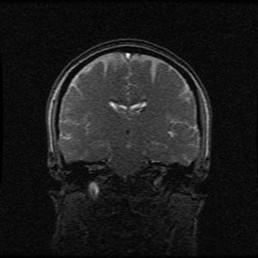
With the push for evidence-based practice, there is an increasing disregard for less common evaluation and treatment methods, such as craniosacral and visceral manipulation. Part of that may be due to the difficulty to formulate a quality and standardizd study using these theories. Personally, after PT school I thought the techniques were similar to the practice of witch doctors. My mind was set in a purely biomechanical perspective. Recently, I spoke with someone who had intense pelvic and abdominal pain after surgery that had her pain eliminated with visceral manipulation. I've heard of similar presentations after gall bladder removal, appendectomy and more. While I am still uncertain of the true mechanism, I have definitely become more open to the atypical approaches. With the development of pain science, we understand how crucial a role the mind plays in our patient's pain levels and treatment. Simply put, if a patient thinks a treatment will work, it will work. There was a time when I thought the use of modalities was equated with out-dated physical therapy, but I have become open to its use in patients who report prior "success" with it (I, of course, educate the patient on the benefits of a more active treatment approach). Going back to a patient's beliefs, we as clinicians can play a significant role in the process. If we build trust with the patient, our explanations of why the patient is experiencing their symptoms can impact the patient's response to treatment. A patient who trusts a craniosacral therapist and their explanation may be more open to whatever changes occur with the treatment. Same rule applies for all treatments. While it is not so simple as to give an explanation to the patient then treat according to that theory, these factors may at least influence our patients. The most difficult aspect occurs when patients have had many various explanations for their pain in the past or were convinced in the past about the source of their issues. My most difficult patients to treat are the ones who memorize their MRI findings. Educating them on how insignificant those findings are can almost completely eliminate any trust that was there in the first place. In conclusion, as a profession, we shouldn't be so quick to eliminate anything that isn't supported by higher levels of evidence. Things like craniosacral therapy and visceral manipulation have been around as long as they have because there is some sort of success. Maybe part of the success is due to a particular subset of the population being more open to the concept and maybe not. Regardless, we should be open to any form of treatment that may benefit our patients, thus increasing the importance of developing an eclectic approach. -Chris Like this post? For more advanced information, join the Insider Access Page now! Also, check out similar previous posts below:
4 Comments
Glenn
7/10/2015 02:45:59 pm
I disagree.
Reply
Thanks for your opinion Glenn! Im not saying you solely perform the unsupported treatment without any others. Absolutely you educate the patient on what the research shows and incorporate that into your management. However it is foolish to ignore patient perception. One of the pillars of evidence based practice is patient beliefs!! If the usual treatment doesnt work with the patient, all im saying is we should consider other styles. If you solely treated based on treatments supported by systematic reviews, youd have a lot of patients not improving. We cant ignore the impact pain science/patient perception has on our treatment.
Reply
Glenn
7/11/2015 07:19:15 am
Hi Chris,
Aaron
7/12/2015 01:34:14 am
I agree with your viewpoints. I feel like an important part of the patient interview is determining their perceptions/beliefs/preferences in terms of what the patient believes is the cause of their pain and what they believe will fix it. Some patients may not have many preconceived notions about their injury or preferences of treatment, but others may have very strong opinions and it is important to be aware in both circumstances. If we only selected interventions based on very high levels of evidence, we wouldn't have much to choose from and we likely wouldn't help many people. Luckily, we have the fortune of being able to spend significant time with our patients and individualizing a treatment approach based on many factors including patient preference.
Reply
Leave a Reply. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|







 RSS Feed
RSS Feed