- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
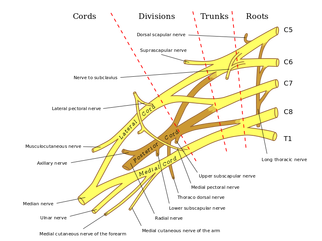
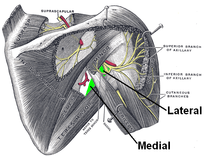
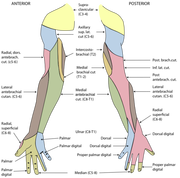
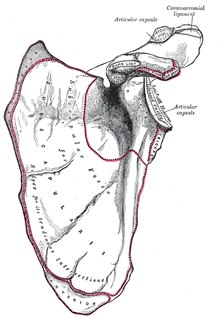
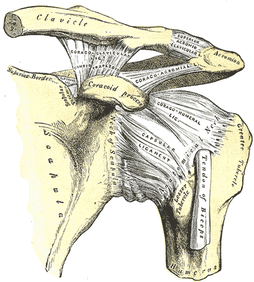
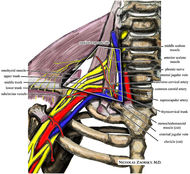 One of the greatest risks following an anterior shoulder dislocation is damage to the neurovascular structures which surround the glenohumeral joint. Due to their anatomical location, certain nerves are at a higher risk of injury than others following a dislocation. Additionally the position and displacement of the arm during the injury is another factor to consider. For example, "a fall with the arm in full abduction and internal rotation causes major tension on all nerves and cords." The Visser et al article also mentioned that concurrent fractures and the presence of a hematoma increasead the risk of nerve damage. Nerves that are at the greatest risk of injury include the axillary, suprascapular, and musculocataneous nerves. Throughout the literature, authors have found that the axillary nerve is most frequently and severely damaged (Visser). The axillary nerve originates from the upper trunk, posterior cord of the brachial plexus carrying nerve fibers from C5-C6. It courses around the surgical neck of the humerus before entering the quadrilateral space (see middle picture below to review the space boundaries). The nerve gives off muscular branches to the deltoid, teres minor, and long head of the triceps brachii. Due to the close association to the surgical neck, the axillary nerve is often compromised during an anterior-inferior shoulder dislocation. A study by Visser et al found that 42% of their 77 patients had axillary nerve insult following a low-velocity trauma anterior shoulder dislocation. Due to the high incidence of nerve related injuries, a complete neurovascular examination is warranted following a shoulder dislocation. This examination should include MMT of the shoulder and arm musculature, palpating for the brachial pulse, and examining sensation of the arm. When assessing for axillary nerve damage in particular, a clinician should look for muscle atrophy of the teres minor and deltoid muscles. One should suspect weak flexion, abduction, and external rotation of the shoulder. Observation and palpation would reveal a flat shoulder deformity due to deltoid atrophy. Additionally, they will have a lose of sensation over the upper lateral arm around the deltoid region due to denervation of the superior lateral cutaneous nerve of the arm (see right picture above). -Jim References:
Visser, C. P. J., L. N. J. E. M. Coene, R. Brand, and D. L. J. Tavy. "The Incidence of Nerve Injury in Anterior Dislocation of the Shoulder and Its Influence on Functional Recovery." The Journal of Bone and Joint Surgery 81.4 (1999): 679-85. Web.
1 Comment
 In recent years, Physical Therapy research has emerged that compares surgical interventions to placebo surgeries. For certain conditions, there is now fairly substantial evidence that surgical intervention is not always necessary despite what is considered standard societal practice. The most recent example of this is a December 2013 article written by Sihvonen et al, that investigated arthroscopic surgical menisectomy compared with placebo surgery for individuals with degenerative meniscal tears. The results were pretty interesting! In a recent post by Leonard van Gelder at Dynamic Principles, he discusses the reasons behind why this appears to continually be happening & gives several good examples of when conservative management is either more successful or equally successful as surgery. Questions you need to ask yourself: -If patients have similar results in surgery vs. placebo surgery, what is at fault in the patient? The mechanical system cannot solely be the answer. The answer lies in the patient's belief system regarding tissue healing and surgery. -How should this change the type of education you give a patient regarding certain conditions? -How do you manage a patient that strongly believes surgery is the answer (after a disc herniation for example) despite knowing that surgery is not always the best course of action. (As Leonard discusses in his post, we are well aware that certain conditions require surgical intervention. By no means are we saying surgery is a bad thing. We are simply bringing light to certain conditions that respond positively from conservative management.) 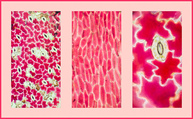 Dosage is one of the most important factors to consider when prescribing an exercise. This decision is often made based off level of acuity, tissue type, anatomical location, patient age, and more. In school, one learns the general principles of exercise prescription, but what is often neglected is WHY you prescribe in certain ranges. "Mechanotherapy: how physical therapists' prescription of exercise promotes tissue repair" is a 2009 article published in the Journal of Sports Medicine that elaborates on this topic. Physiologically, what stimulates tissue repair of articular cartilage, muscles and tendons is a term called Mechanotransduction. In this article Mechanotransduction is defined as "the process by which the body converts mechanical loading into cellular responses." This can be thought of in clinical terms as what is occurring at the histological level to allow one to prescribe a certain exercise dosage without increasing the risk of injury. Mechanotransduction can be broken down into 3 phases: 1) Mechanocoupling: This is the physical load cells undergo while in repair. The physical load is transferred into chemical signals which stimulate cellular changes. 2) Cell-Cell Communication: When one cell is stimulated, other cells in the area (whether directly stimulated by the initial mechanical stimulus or not) will undergo a cellular response. 3) Effector Response: When a cell is mechanically stimulated through compression, distraction, etc., several processes will occur intrinsically to allow change to occur. Now knowing each of the 3 stages, you must think about them in relation to the Type of Tissue involved to understand how that tissue heals. Tendon Healing: When a tendon is trying to heal, there is up-regulation of insulin-like growth factor, other growth factors, and cytokines which allows for cellular proliferation and tissue remodeling. Because healing is occur at the cellular level, too much stress OR too little stress on the tendon tissue could cause an alteration in the up-regulation, not allowing the tendon to rehabilitate optimally. The research up-to-date shows that tendons responds positively to "controlled loading." Research focusing on the type and intensity of controlled loading (eccentrics, assisted, resisted) is still ongoing. Muscle: The authors Khan and Scott state that "muscle offers one of the best opportunities to exploit and study the effects of mechanotherapy" because of how muscle tissue responds to loading. We know there is an overload of mechanogrowth factor (MGF) released when load is induced on the muscle force. This in turn causes muscle cell hypertrophy due to a cell-to-cell communication with nearby satellite cells. At this point, the research shows that early loading after a brief immobilization period is essential for minimizing atrophy and restoring normal cellular structure of the muscles. Articular Cartilage: Articular cartilage is comprised of a large population of mechanosensitive cells. It is hypothesized that by repetitively stimulating the articular cartilage with a low load/high repetition exercise dosage, better outcomes will result. One study assessing full thickness cartilage defects following periosteal transplantation demonstrated that individuals who used continuous passive motion (low load/high repetitions) had greater outcomes than those who did not receive this intervention. As with all things, research is ongoing. Bone: When assessing bone healing, osteocytes are the primary mechanosensors. A recent study looking at individuals following a distal radius fracture had stronger bone growth if they received intermittent compression as an adjunct to the standard of care (compression & gripping exercises). The pneumatic compression allowed for extra stimulation of the bone cells and an increased healing rate. We know parts of this article are dense, but understanding what is occurring at the cellular level can greatly change your viewpoint of how various tissues heal. Through each of these tissues we can see that Mechanotherapy plays a unique role in healing of different tissues types. The healing of osteocytes differs from that of chondrocytes which differs from myocytes. It is fundamental to understand these differences in order give appropriate doses during exercise - just as it is important to know the tissue type you should be treating following your examination. As a general rule of thumb: Articular Cartilage: Low Load, High Repetition; ~15% 1 RM; Thousands of repetitions. Tendon: Controlled Loading; consider eccentric exercises, but do not overload the tissue. Muscle: allow for a brief period of immobilization to restore homeostasis following injury. Bone: Based on location of the fracture, consider adding compression to your treatment to improve rate of bone growth and decrease healing time. References:
Khan and Scott. (2009) "Mechanotherapy: how physical therapists' prescription of exercise promotes tissue repair." British Journal of Sports Medicine. 2009; 43: 247-251. Web. 5 Dec. 2013.  Subacromial Impingement Syndrome (SAIS) is reported to be the most frequent cause of shoulder pain in an OP physical therapy clinic. Despite the high prevalence, physical therapists still struggle to appropriately diagnose the syndrome. The gold standard for diagnosing SAIS in arthroscopic surgery. Since we do not have access to this tool everyday, we must reply on our patient examination skills. A study by Michener et al, Reliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests for Subacromial Impingement, assessed 5 special tests commonly used to help rule-in SAIS. The 5 tests were Neers, Hawkins-Kennedy, Painful Arc, Empty Can (Jobe), and External Rotation Resistance Test. Specifically this article wanted to assess the interrator reliability of the tests, diagnostic accuracy of each test, and finally if clustering the tests would confirm or rule-out SAIS. The results of the study were surprising. Moderate to Substantial strength of agreement between raters was found for the empty can test, the painful arc sign, and external rotation resistance test. Surprisingly Hawkins Kennedy had the lowest kappa value at .39. We found this surprising because Hawkins-Kennedy is graded as painful or not painful. There seems to be little room for subjectivity, yet it received the lowest reliability among raters of all the tests. The difference likely lies in how the test is performed and thus perceived. It is easy to forget to not horizontally adduct the shoulder sufficiently or to ignore the patient's compensation of elevating the tested shoulder during IR as a means of avoiding/minimizing the pain provocation. Something we must always be wary of in studies of manual techniques is accepting the fact that all examiners perform/analyze movements the same. When looking at the diagnostic accuracy of each test individually, the External rotation resistance test had the highest positive likelihood ratio (LR) of 4.39, empty can had the second highest with 3.9, and the painful arc sign came in third at positive LR 2.25. Finally, the article found that when clustering the tests a "combination of any 3 positive tests out of the 5 have the best ability to confirm SAIS, with small to moderate shifts in the pretest to posttest probability." While this article provides interesting and useful clinical information, the results are different from other studies in the literature. A separate article on SAIS by Park et al found that the clustering Hawkins-Kennedy, Infraspinatus Muscle Test, and the Painful Arc Sign yielded a high +LR (10.56) for ruling-in SAIS. So what cluster should you use? Personally, we would use both. The etiology of SAIS is multifactorial. Several structures have the potential to be pain generators and the presentation of SAIS will vary based on posture, scapulohumeral rhythm, accessory joint mechanics, and more. The Michener article was quick to point out the importance of a thorough subjective history to help aide in the diagnostic process. Reference: Michener LA, Walsworth MK, Doukas WC, Murphy KP. Reliability and diagnostic accuracy of 5 physical examination
|
| After doing some reading about regional interdependence for the SFMA inservice, we thought it would be interesting to look at some research regarding thoracic spine manipulation for shoulder pathologies, especially with the evidence for thoracic manipulations for neck pain. Regional interdependence is the idea that impairments in a separate anatomical area can contribute to the patient's primary complaint. Due to the seemingly unconventional connection between the thoracic spine and shoulder, it may appear unusual to treat shoulder pathologies with t-spine manipulations, but let's remember that limited thoracic mobility can affect the shoulder position and potentially lead to pain. There have been several studies looking at this relationship, and others. Overall, there is a decent amount of evidence displaying short-term pain relief following thoracic manipulation for shoulder pathologies, such as shoulder impingement syndrome or rotator cuff tendinopathy, even though the mechanism is poorly understood. This could potentially hasten the rehabilitation process, by allowing more aggressive therapy. |
Boyles et al performed an exploratory study on the effects of a single thoracic spine manipulation on subacromial impingement syndrome. While no additional treatment was performed, the authors were able to find statistically significant changes in both pain and disability scores in just 48 hours; however, these results were not found to be clinically significant, based on the established minimal change for clinical significance. The methods of this study were lacking in several areas: low participant number, no randomization, no control group, and more. The authors realized this and emphasized the fact that this study should be used as a launching point for further studies. The fact that significant changes were created after one treatment alone in just 48 hours suggests the potential for a component of care in dealing with patient suffering from subacromial impingement syndrome. Just as manual therapy + exercise was found to be greater than exercise alone for cervical pain, maybe the same applies to these conditions. Additionally, when using thoracic manipulations for cervical pain or lumbar manipulations for low back pain, there exists specific inclusion criteria in order to have the desired results. Again, maybe the same applies to thoracic manipulation for subacromial impingement (or other should pathologies) and we just need to discover the criteria. Sounds like a perfect research opportunity! Obviously, solid evidence on this topic is still lacking, but we hope that this research has at least opened your mind to the possibility of regional interdependence in your patients and maybe treating either the cervical or thoracic spine (or both) the next time you have a patient with a shoulder pathology.
Boyles RE, Ritland BM, Miracle BM, Barclay DM, Faul MS, Moore JH, Koppenhaver SL, Wainner RS. (2009). The short-term effects of thoracic spine thrust manipulation on patients with shoulder impingement syndrome. Man Ther. 2009 Aug;14(4):375-80. Web. 15 May 2013.
Muth S, Barbe MF, Lauer R, McClure PW. (2012). The effects of thoracic spine manipulation in subjects with signs of rotator cuff tendinopathy. J Orthop Sports Phys Ther. 2012 Dec;42(12):1005-16. Web. 15 May 2013.
Strunce JB, Walker MJ, Boyles RE, Young BA. (2009). The immediate effects of thoracic spine and rib manipulation on subjects with primary complaints of shoulder pain. J Man Manip Ther. 2009;17(4):230-6. Web. 15 May 2013.
Walser RF, Meserve BB, Boucher TR. (2009). The effectiveness of thoracic spine manipulation for the management of musculoskeletal conditions: a systematic review and meta-analysis of randomized clinical trials. J Man Manip Ther. 2009;17(4):237-46. Web. 15 May 2013.
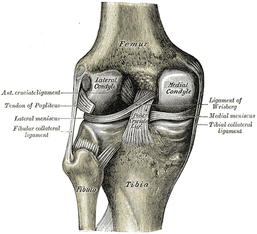
The article we looked at discusses using Joint Line Fullness as a clinical test. The patient is supine and the examiner palpates along the affected joint line to compare fullness to the uninjured side. If the joint line fullness causes a loss of joint compression, the test is positive. The lateral side of the knee is examined in 30-45 degrees of knee flexion to slacken the IT Band, while the medial side of the knee is examined at 70-90 degrees of knee flexion to slacken the MCL. The test had a sensitivity of .70 and specificity of .82. Again, by itself, this test's accuracy is still lacking. One might argue that it could potentially replace Joint Line Tenderness in the cluster to increase the diagnostic accuracy even more, however, we must look at the methods of the study first. The study excluded any patients with an acute injury (within 6 weeks of exam) or presence of osteophytes, joint space loss, or arthritis. Due to the fact that we often see our patients in the acute stage within 6 weeks of injury and frequently our patients have arthritis, the findings of this study become questionable. If many of our patients are bound to have the exclusion criteria, will the test still prove useful? Now, we are not suggesting that the test has no usefulness, but perhaps an additional study should be performed, where these patients are included.
Reference:
Couture JF, Al-Juhani W, Forsythe ME, Lenczner E, Marien R, Burman M. (2012). Joint line fullness and meniscal pathology. Sports Health. 2012 Jan;4(1):47-50. Web. 14 May 2013.


This research article, The Ability of Clinical Tests to Diagnose Stress Fractures: A systematic Review and Meta-analysis, assesses the reliability of both therapeutic ultrasound and the tuning fork test. The review discusses when, why, and how these tests should be implemented. As Schneiders et al, points out "clinically lower-limb stress fractures can be difficult to diagnose, due to a wide range of potential differential diagnoses." This differential diagnosis process should include (but not be limited to) compartment syndrome, muscular strain, tendinitis, tendinosis, infection, and nerve entrapment. Additionally, it is important to know the gold standard for ruling in stress fractures. Currently, a triple phase technium-99 bone scan (scintigraphy) is the most accurate method of diagnosing stress fractures with a sensitivity of 100% and specificity of 76%. MRI has also shown to be highly reliable, but due to its expensive cost, they are less frequently used. Additionally, the single photon-emission CT scan is receiving a lot of attention for it's accuracy in diagnosing stress fractures, but further research is needed.
As therapists (excluding the military), we do not have the power to order the gold standard tests mentioned above, so we must rely on our own diagnostic tests to help us interpret our patient's clinical presentation. Clinical tests that are currently used and accepted include therapeutic US, the tuning fork test, superficial palpation, and palpable thickening or swelling of periosteum. This review looked at therapeutic US and the tuning fork.
| Therapeutic Ultrasound: Why it works? Following a stress fracture, there is increased osteoclastic resorption, which leads to periosteal damage. The increased resorption allows for increased heat absorption during ultrasound; therefore stimulating pain receptors at the site of injury. Additionally, mechanical waves from the ultrasound can become trapped between any break in the bone, which can stimulate periosteal nocioceptors. | The Tuning Fork: Why it works? Following a stress fracture, the bone periosteum is damaged. Under normal conditions, the intact periosteum has the ability to disperse vibratory forces across the bone. The damaged periosteum of a stress fracture, absorbs increased vibratory forces and stimulates pain receptors. |
Scneiders A, et al. (2012). The ability of clinical tests to diagnose stress fractures: a systematic review and meta-analysis. JOSPT. 2012; 42.9: 760-771. Web. 1 May 2013.
Insider Access pages
We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!
Archives
July 2019
June 2019
May 2019
March 2019
February 2019
January 2019
December 2018
November 2018
October 2018
September 2018
August 2018
July 2018
June 2018
May 2018
April 2018
March 2018
February 2018
January 2018
December 2017
November 2017
October 2017
September 2017
August 2017
July 2017
June 2017
May 2017
April 2017
March 2017
February 2017
January 2017
December 2016
November 2016
October 2016
September 2016
August 2016
July 2016
June 2016
May 2016
April 2016
March 2016
February 2016
January 2016
December 2015
November 2015
October 2015
September 2015
August 2015
July 2015
June 2015
May 2015
April 2015
March 2015
February 2015
January 2015
December 2014
November 2014
October 2014
September 2014
August 2014
July 2014
June 2014
May 2014
April 2014
March 2014
February 2014
January 2014
December 2013
November 2013
October 2013
September 2013
August 2013
July 2013
June 2013
May 2013
April 2013
March 2013
February 2013
January 2013
December 2012
November 2012
October 2012
September 2012
August 2012
Categories
All
Chest
Core Muscle
Elbow
Foot
Foot And Ankle
Hip
Knee
Manual Therapy
Modalities
Motivation
Neck
Neural Tension
Other
Research
Research Article
Shoulder
Sij
Spine
Sports
Therapeutic Exercise







 RSS Feed
RSS Feed