- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
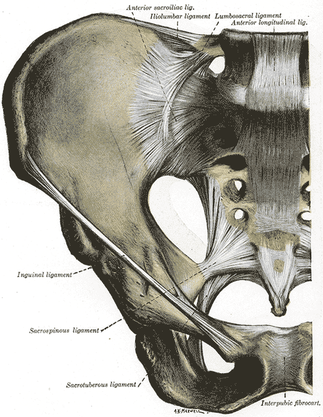
Jackson and Porter bring up the fact that there is essentially no research on the topic of non-painful SIJ Dysfunction. Once again, just because there is no research in an area, does not indicate that it should be dismissed as non-existent. We tend to become overly reliant on our pain provocation tests. So what do we do? We definitely recommend still utilizing your clusters, palpating soft tissue, and utilizing subjective information such as Fortin's Sign to aid in diagnosing painful SIJ Dysfunction. As for non-painful dysfunction, practice and implement the motion restriction tests that you are taught in school. We are trained to be competent in tests like Lachman's and Drawer Tests that require identification of differences in movement around a few millimeters. In theory, we should be able to identify some abnormalities in the sacroiliac joint as well. Now, we recognize that research has shown poor reliability for those tests and for good reason, but they may still aide in picking up severe restrictions that will lead to diagnosis and treatment in order to facilitate the return to normal mobility. Reference:
Jackson R and Porter K. The Pelvis and Sacroiliac Joint: Physical Therapy Patient Management Utilizing Current Evidence. Current Concepts of Orthopaedic Physical Therapy, 3rd Ed. La Crosse, WI. 2011.
8 Comments
Jerome french PT
8/27/2013 11:27:27 pm
I recommend to read the Diane Lee's book "the pelvic girdle" which is a great tool for the lombo-pelvi-hip complex's assesment and treatment.
Reply
Steve
8/29/2013 03:36:09 am
While I have not read your reference, but plan to, it seems that if a joint is not painful, then there are two ways you are brought to assess it: motion (increased or decreased) or by default (nothing else is working). The default position occurs in chronic pain patients or when the level of pain reduction or functional limitation is not acceptable to the patient...or maybe even the clinician. At that point a discussion should be undertaken so the patient knows you are trying something new.
Reply
Thank you for your comment Steve. We definitely recognize the limits in detecting mobility and alignment consistently and reliably in the SIJ, especially due to the lack of natural symmetry in the bones. However, just because the evidence has been weak thus far in the area does not necessarily mean the possibility should be eliminated. I think we would be fools to ignore all other impairments and instead focus on what we "think" we are seeing in the SIJ, regarding alignment and mobility. That being said, I think we should lean more towards the approach of "nothing else is working," except that we might instead decide to incorporate the treatment of the SIJ into our program in addition to the regular impairment-focused interventions of the rest of the body.
Reply
Jerome french PT
8/29/2013 04:44:04 pm
Studies show 4° of mobility for the SIJ which is hard to feel , you can test it not neccessary in motion but with compression, distraction or the P4 test, at this point if you find a reproduction of symptom you can go with motion assesment. However, i think the symptom is the key to incorporate it or not in the treatment.
Reply
You are correct in that those listed tests are excellent for detecting pain coming from the SIJ, especially if clustered. However, what we are discussing here is when pain is not coming from the SIJ, but the SIJ's mobility impairments are contributing to the pain produced elsewhere. Again, you are correct in that there is little measurable motion in the SIJ, which is hard to detect. But the difference in detecting an intact ACL and a ruptured ACL is something like 3 mm. We are still able to appreciate the difference there. Obviously, the reliability for mobility testing of the SIJ is pretty low, but just because something has poor evidence does not mean we should completely eliminate the possibility from our minds. Instead we should be looking for ways to better those examination methods!
Reply
Steve
9/2/2013 11:50:57 am
Yes, but with a Lachman's you have or do not have an end point. I believe the tibial translation is also closer to 10mm. The 3 mm I was referring to is with a difference between sides. And the point I was making about Lachman's was more along the lines of our ability to just detect movement. I absolutely agree that there are proper ways of evidence based practice to better our skills, what I meant was we should not simply rule something useless because of some evidence. For example, look at skills of the examiners in studies. And absolutely we want to look at hip, thoracic, and more for LBP patients. I was only indicating that we shouldn't exclude the SIJ.
Reply
Leave a Reply. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|






 RSS Feed
RSS Feed