- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
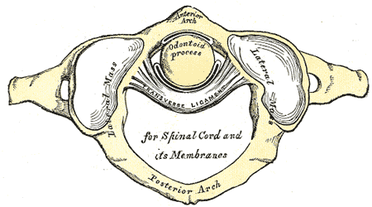
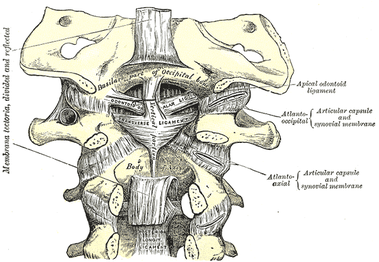
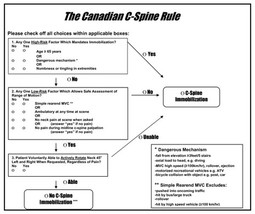
Something that should be included in every upper quarter evaluation, especially following a MVA, is ligament integrity testing. As physical therapy moves towards primary care, we must be certain we screen our patients for any potential instability or hypermobility in the cervical spine that may impact the patient. In general, you want to check both the transverse and alar ligaments both for integrity and laxity. With integrity deficits, the patient must be referred back immediately. With laxity, we may just choose not to utilize certain manual therapy techniques like manipulation. Anatomy The transverse ligament attaches at the medial side of each large, lateral process of the atlas with the anterior side of the middle part touching the odontoid process. The transverse ligament is responsible for maintaining the space of the vertebral canal by preventing the atlas from translating anterior relative to the dens. When damaged, the atlas slides anteriorly, impinging upon the spinal cord. There are two alar ligaments. The distal portion of each attaches to the respective sides of the odontoid process of C2. The proximal portion attaches to the tubercle on the medial side of the respective occipital condyle. When the head rotates or sidebends one direction, the tension in both alar ligaments (especially the contralateral one) is responsible for the spinous process of C2 moving the opposite direction. Performing the Tests Supine Transverse Ligament Stress Test: Place one hand on the occiput with the index finger on the space between C2 spinous process and occipital protuberance (where the posterior arch of C1 lies). Place the other hand on the forehead. Lift the head straight up in a vertical plane (not flexion, more of a protraction motion). The test is positive if the patient experiences some feelings of weakness, dizziness, numbness, nystagmus, or an odd feeling in the back of the throat. There is normally a firm end-feel. You should also note immediate motion of C2 spinous process when PA is applied to C1 posterior tubercle. If there is a delay, there may be laxity present. It should be noted that pain, by itself, is not a positive finding. We are looking for the neurological symptoms or "lump in the throat." Sharp-Purser Test (for Transverse Ligament): The patient should perform a slight cervical nod. The examiner then places one hand on the forehead, while the other hand is placed on the spinous process of C2 (both arms should be parallel to the ground!). A posteriorly directed force is applied by the hand on the forehead, while the hand on the spinous process of C2 just stabilizes. There should be a firm end-feel. A positive test occurs if there is a sliding movement of the head or a decrease in symptoms (often neuro symptoms; “clunk” may occur). Pain is not a positive finding. Alar Ligament Test: Place one hand on the occiput and use the other hand to palpate the spinous process of C2. Laterally flex or rotate the head to one side; you should feel the spinous process move to the opposite side. Repeat on the other side. Absence of the spinous process moving to the opposite side may indicate alar ligament injury. If you block the spinous process of C2 from moving, you may stress the ligament, looking at laxity. You should encounter a firm end-feel in this case. Significant movement may indicate ligamentous injury. Pain is not a positive finding. These tests are not enough by themselves, but when incorporated with your other exam findings, are essential for screening patients for instability. The reason I wanted to discuss this topic was the fact that I had a patient recently who had no cervical imaging following an MVA but was "cleared" for PT by a physician, even though the patient met part of the Canadian C-spine rules. This patient in particular was referred back for imaging, especially due to the potential "clunk" felt during Sharp-Purser test. Additionally, while I indicated in all the tests that pain is not a positive finding for the ligament stress testing (we are looking for neurological findings), the presence of pain may potentially indicate a sprain of the ligament. Typically, it just represents a hyper-sensitization of the nervous system in that region, however. Unfortunately, some specialties of physicians lack sufficient orthopaedic knowledge and training. It is for this reason that we must be highly skilled with our screening, especially if we want to increase our direct access. -Chris Fox PT, DPT, OCS Check out our Insider Access Page for advanced content!Other Similar Posts:
0 Comments
Leave a Reply. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|







 RSS Feed
RSS Feed