- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
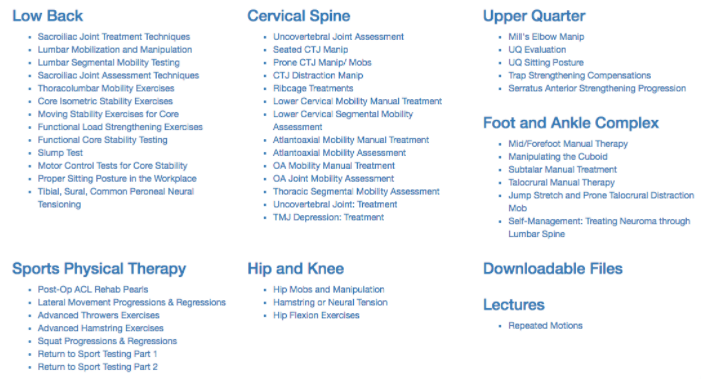
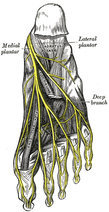 Plantar Fasciosis can be a very difficult condition to treat because of the intricate anatomy of the foot and ankle complex. To complicate issues, we now know that many lower quarter problems root from lumbopelvic and hip dysfunction as well. In previous posts, TSPT has done a literature review of the condition as well as talked about new treatment methods regarding plantar fasciosis. In these posts, one aspect of management we did not discuss in depth is assessing for neuropathic pain. From my clinical experiences and the experiences of my colleagues at the Harris Health System, many patients with plantar fasciosis have positive neural provocation tests for the distal branches of the tibial nerve. Anatomy Review After the tibial nerve passes around the medial malleolus, it splits into three distal branches: the medial plantar nerve, lateral plantar nerve, and medial calcaneal branch. Specifically, the lateral plantar nerve innervates the fifth and lateral 1/2 of the fourth toes and provides motor input to many of the intrinsic foot muscles. The nerve passes laterally across the foot and splits between the flexor digitorum brevis and quadratus plantae. Assessment To assess for tibial nerve adverse neural tension, have the patient lie supine. Passively extend the toes, dorsiflex and evert the ankle. This combined movement place a stress across the tibial nerve and its distal branches. Ask the patient if this position changes their primary symptoms (better, worse, or the same). Next, passively perform a straight leg raise maintaining the foot and ankle components. If this position recreates their primary symptoms, they have positive neural tension in the tibial nerve* (remember to test bilaterally as well). To further assess the tibial nerve, adduct and internally rotate the lower extremity. If the test is positive, appropriate treatment options include nerve sliders, tensioners, and manual therapy. *When performing a straight leg raise, you are changing the hip component. No musculoskeletal structure courses from the hip to the ankle, so if symptoms change it must be the nervous system that is being assessed. Conclusion -Lateral plantar nerve pain can be a contributing factor to plantar fasciosis pain. -By performing the proper assessment (discussed above), you can identify if neural tension is part of your patient's symptoms. -Do not underestimate the impact of the peripheral nervous system in musculoskeletal dysfunction. Lower Extremity Peripheral Nerve Testing [Video taken from TSPT Insider Access Library- subscribe to learn other advanced assessments!] Author: Jim Heafner PT, DPT, OCS is one of the founders of The Student Physical Therapist. He is owner of Heafner Health Physical Therapy in Boulder, Colorado. Are You on the Inside?Looking for advanced sports and orthopedic content? Take a look at our BRAND NEW Insider Access pages! New video and lecture content added monthly.
5 Comments
11/15/2014 12:44:26 pm
Great post and I think screening the peripheral nervous system for potential involvement is great. My question is when doing this lateral plantar nerve/tibial nerve test, how do you know that the set up for the neurodynamic test is not just reproducing the patient's symptoms due to increased tension in the plantar fascia during the toe extension/dorsiflexion/eversion step prior to the SLR. The toe extension/dorsiflexion/eversion is very close the "windlass test" which is essentially a plantar fascia tension test. Would perhaps a slump be too general to pick it up by tension from the top down? Or bowstring tests at the dural tension point in the SLR but with the ankle in resting position so as to not create tension along the plantar fascia and potentially limit the false positive? Just a thought.. great post.
Reply
Alfred
1/19/2015 01:56:53 am
I believe the answer (correct me anyone if I'm wrong) lies in adding the SLR component and then rechecking sx (better, worse, same). If it is worse by adding the hip component, you tend to think there is a neural component over muscular. Hope that helps
Reply
Jim
9/12/2016 01:57:58 pm
Yes! Alfred is correct. By adjusting a proximal component (i.e. the hip), the examiner can determine if the symptoms are coming from a nerve or plantar fascia. A change in symptoms by changing the hip component will implicate the nerve structure.
Reply
Teresa J Anderson
3/9/2019 09:52:32 am
Thank you for doing this video, I just have a suggestion that there needs to be a variation in the color of the clothing, when the tester and the patient are all wearing black it all blends together in the video and I can't really see much about hand placement Etc. Thank you very much
Reply
5/2/2023 10:45:01 pm
Great! I love to read this! Thank you. If you want to gain more insights about foot problem, surgery and others. Try to visit this site.
Reply
Leave a Reply. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|






 RSS Feed
RSS Feed