- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
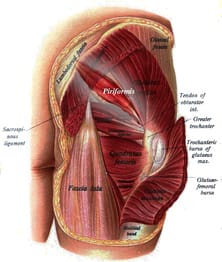 One of the frustrating aspects of research studies that is often overlooked is that patient population, and, more specifically, the diagnostic criteria for that population. Without a specific diagnosis (and conclusive method of diagnosing), the study immeidately presents with multiple confounding variables. Our ability to assess the benefit of an experimental intervention becomes inconclusive when there is a lack of homogeneity in the group. In one of mentoring sessions at Optim, there was a disagreement about pain referral patterns for piriformis syndrome. One individual stated that research well-supported piriformis syndrome up to the spine. I had disagreed as typically pain does not refer that far upwards. Of course, after hearing this disagreement, I went ahead to looked at some of the research behind piriformis syndrome. In this systematic review, the article basically starts out with explaining on piriformis syndrome is a controversial diagnosis and we have little to no clinical ability to diagnose it. Moving onto the actualy results, there was between 14-63% participants with low back pain. Looking simply at the results, it would appear that low back pain is a common finding in those with piriformis syndrome. However, based on the fact that we have difficulty even diagnosing the pathology, we can't rule out the possibility (in my opinion, likelihood) that the lumbar spine may be the source or the primary component (think Double Crush Syndrome). This conflict should basically have stopped the study as all findings, in reality, have fault in basis. So what does this mean clinically? For me, not much. I treat the impairments primarily in my patients. If a patient did come in with "piriformis syndrome," I'm going to address any lumbar mobility restrictions I find. If the hip is weak, I'm going to strengthen it. That be said, there are some conditions where specific diagnoses do have clinical impact. For example, if a specific diagnosis has been shown to benefit significantly from a particular intervention, that will absolutely be included. In most cases, we need to be more critical analyzing all aspects of the article, especially the population/diagnostic criteria before we implement the results in our practice. Evidence-informed, not evidence-restricted. -Dr. Chris Fox, PT, DPT, OCS Reference: Kevork Hopayian,1,3 Fujian Song,1 Ricardo Riera,2 and Sidha Sambandan1. The clinical features of the piriformis syndrome: a systematic review. Eur Spine J. 2010 Dec; 19(12): 2095–2109.
2 Comments
Mary Kate Mcdonnell
1/2/2017 07:10:05 am
Agree with post. Better to make distincton of Diagnosis as a Medical Diagnosis. Agree. Medical dx may not be well defined and does not always direct a PT. Consider, using movement system dxs along with medical dx to direct PT intervention. Ex- piriformis syndrome = PT dx - Hip Addiction Medial Rotation Syndrome. (Sahrman, SA. Movement System Dx. Mosby)
Reply
Leave a Reply. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|








 RSS Feed
RSS Feed