- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
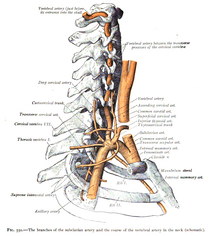 With the physical therapist's increased emphasis on incorporation of manual therapy when treating the cervical spine, the concern of vertebrobasilar insufficiency is frequently discussed. Even though fewer people have adverse effects from cervical manipulations compared to NSAID's, there is still a stigma revolving around the disease, and rightfully so. Part of the reason the incidence of adverse effects following cervical treatment is due to appropriate screening methods. We all know that the Vertebral Artery test has insufficient psychometric properties for diagnosis. If a test is negative, it doesn't change anything. If it is positive, the patient might have VBI. The sensitivity and specificity of the test is so low that some clinicians actually prefer not using the test. Personally, I still use it, due to the public perception that it is required for "screening"; however, I consider the diagnostic accuracy in my clinical reasoning. What is more beneficial in the screening process is a thorough subjective history. There are signs and symptoms that increase the likelihood of the patient having the disease. We should be asking about nausea and vomiting, the 5 d's (dizziness, drop attacks, diploplia, dysphagia, dysarthria), and look for nystagmus. Also, consider other past medical history like cardiovascular disease. Most programs and manual therapy classes spend time going through how to properly take the subjective and what to look for when determining the likelihood of VBI. So what do you do when both the subjective and objective are ruling in VBI? I recently had a patient with "neck pain" come to my clinic for an evaluation. I noticed immediately that the patient had a sense of caution when turning her neck. She described her neck pain extremely vaguely on both sides of her cervical spine and upper trap. As part of my screening process for upper quarter patients, I ask about dizziness, N&V, and a few other questions that are linked to various pathologies. The patient reported she did have some dizziness when turning her head and changing positions. Initially I suspected BPPV, but also wanted to continue exploring other possible symptoms. The patient reported dizziness, fainting, blurred vision when turning her head, and difficulty forming words occasionally. That is 4/5 D's and she ended up having positive nystagmus with full cervical rotation after about 10 seconds which also recreated her dizziness. The patient apparently never told the doctor about her dizziness, fainting, or trouble speaking because she thought they were unrelated. Additionally, the patient reported a history of HTN and was in her upper 50's. Having never actually encountered someone with a collection of these S&S that may be associated with VBI, I knew I would not perform treatment without further work-up by the physician. I called her doctor and they wanted her to come in that day. I was unsure; however, if, had I not been able to get a hold of the doctor, should I have sent her to the ER. She had been walking around with these symptoms for 6 months, but with the risk for stroke, should we be referring these patients to the ER? It is a tough decision that may be based on each patient's individual presentation. We don't want to send any patient with neck pain and dizziness to the hospital. A single "red flag" does not have much clinical value, but a collection of them does and we need to act appropriately. What do you think is the next correct step? -Chris
13 Comments
mary
2/25/2015 08:35:40 pm
U did the right thing I have had this happen...I work alot with vestibular pts too..chances are if u think its something more serious Ur right, now finding someone to properly do the right rest and assess them medically now that's another story right?!! I like Ur blogs by the way!!
Reply
2/26/2015 01:09:41 am
As mary said, the tough part is finding someone who will treat them properly! Good Luck!
Reply
2/26/2015 08:25:54 pm
I read your case story with a lot of interest. It's indeed a tough decision. Your patiënt does have some serious symptoms that could be connected with VBI. Good luck!
Reply
Steve
3/3/2015 01:26:49 am
A few things:
Reply
Hi Steve,
Reply
Greg
3/6/2015 11:56:13 pm
Hey Chris, 2nd year studemt here. While I knoe this is absolutely of secondary concern behind the patient's safety, how did you handle explaining to the patient your concerns without scaring her and was she upset that you wouldn't treat her?
Warda
10/1/2018 09:12:24 am
I have a similar case. Pt has sx of VBI post MVA. She also has bicep tear and teres major and infraspinatus pathology. Coming from a third world country, our doctors are loaded so my pt can only seen at the end of this month! Her injury was about a month ago. I've been advised to keep seeing her for her other injuries but I'm concerned that nothing is being done about the VBI. Could I work on cervical stability at least? What treatment would the doctors provide anyway? (A common mismanagement is painkillers :/)
Reply
Hi Greg,
Reply
zainab Hasan Ali
4/11/2018 10:06:27 am
Hy,i am doing internship in hospital, pt department, i saw a patient, having spondylosis at c5-c6 level, having spasm around neck ,on treps specially ,her doc send her to pt on her frst visit pt did hot pack thing then stretching of neck ,when i asked her (pt) about her vbi test she said its posotive she was also feeling numbness in her limbs specially in right hand, she was depressed as well, now question is, is. It permissible to perform any stretching or any physical treatment despite being knowing that she was feeling dizziness on every movement of her neck and vbi is positive?
Reply
TSPT- Jim
4/22/2018 08:36:48 pm
I would do some further workup and testing personally. It sounds like her symptoms could be either radiculopathy OR VBI. If you retest VBI and it is positive, I would not perform any stretching until further work up.
Reply
Donna Carter
6/12/2019 06:51:12 am
I have been diagnosed with VBI and have lost vision temporarily 3 times (once while driving). My PCP doesnt seem to know what to do about this or who to refer me to. Do I need to see a neurosurgeon or a vascular surgeon? Headaches and neck pain are killing me.
Reply
TSPT
6/12/2019 07:10:44 am
We would recommend following up with a vascular surgeon or cardiologist. Good luck!
Reply
Leave a Reply. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|






 RSS Feed
RSS Feed