- Home
- About Us
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
|
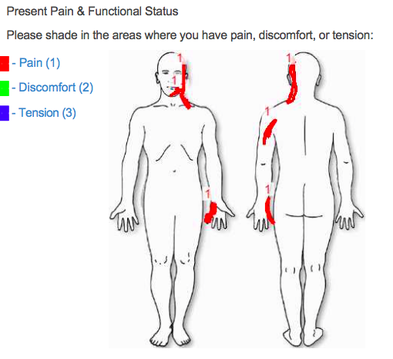
A patient recently presented to my cash-based clinic (Heafner Health) with the pain diagram seen above. The patient had a three-year history of left upper extremity pain that has been limiting almost all daily activities. From the picture alone, my first three clinical pathoanatomical hypothesis' were cervical radiculopathy, ulnar nerve peripheral neuropathy, or a double crush syndrome (thoracic outlet syndrome could be included in the double crush category). Additionally, due to the chronicity of his symptoms, I knew the patient would have some degree of central sensitization.
During the initial evaluation, he presented with the movement impairment syndrome of left scapular downward rotation and depression. Primary impairments included decreased left thoracic rotation, decreased scapular upward rotation, hypomobility in the CT junction and mid thoracic spine, poor serratus anterior and lower trapezius strength, and a positive ulnar nerve tension test. Additionally, the patient was unable to maintain cervical stability with any shoulder movement above 90 degrees. Following the objective examination, manual treatment included a supine thoracic manipulation, Grade IV CT junction mobilizations, IASTM to the left upper trapezius and scalene muscles, and active assistive sidelying scapular upward rotation. Following the OPTIM treatment paradigm, the manual interventions were followed with corrective exercises. These included seated upper trapezius shrugs (with arms resting on a pillow), serratus anterior presses with the shoulders at 90 degrees, and seated chin tucks with upper thoracic extension. We attempted ulnar nerve tensioners, but I did not feel comfortable prescribing them as part of his HEP. The patient was given education on chronic pain (told to watch ‘understanding pain is less than 5 minutes’ and the ‘Lorimer Mosely TEDx Talk’) and ergonomic set-up. Following the treatment session, the patient's upper limb tension test had improved by nearly 40 degrees. What other initial diagnoses were you suspecting based on the pain diagram? Anything else you would add to the initial treatment? -Jim Heafner PT, DPT, OCS
7 Comments
Felipe Baeza
8/29/2016 05:21:05 am
I would add a cervical (articular) assesment and if it is necessary make cervical manipulación. And excercises for cervical stability. And find trigger points.
Reply
El
8/29/2016 06:18:32 am
I feel you have done too many things at once -if he returns better or worse you won't know what did what and will have troubles to diagnose and rehabilitate appropriately.
Reply
Steve
8/29/2016 07:35:00 am
Does it really matter if he "did too many things at once"? The patient feels better and is presenting better. That's what counts.
Reply
chad
9/6/2016 10:45:31 am
I agree w/ El, perhaps to many things all at once. But the end goal is to decrease pain as rapidly as possible and it sounds like this was accomplished very well. I generally perform one movement and look for a change & prescribe as hep (mostly because patient are non compliance), but also that way I can be more confident it what will and will not help the patient.
Reply
I curious to see what you mean by doing too much El! I always try to find the top primary impairment(s) and address those issues. For this case, each one of those interventions were successful in the clinic so I want them to be part of his home program. Addtionally, all 3 exercises in the HEP focus on improving upward rotation (or meet a requirement that is necessary for upward rotation)
Reply
Richard Field
12/16/2017 09:22:55 am
In absence of a palpatory exam of cervical and thoracic spine I diagnose a facilitated segment at C2/3 Left. Together with same at C6/7 Right. This may be as result of lateral scoliosis D/L concave Right.
Reply
5/16/2024 11:50:44 pm
In the intricate realm of healthcare, the pursuit of an accurate diagnosis is paramount. Amidst the complexity of symptoms, tests, and medical histories, clinicians navigate the terrain with precision and empathy. Within this framework, the concept of "Border Free Health" emerges, emphasizing inclusive, accessible care for all. Whether deciphering the subtleties of a mysterious ailment or unraveling the layers of a chronic condition, the diagnosis becomes a beacon of clarity and hope. It signifies not just a label, but a pathway to understanding, treatment, and ultimately, healing.
Reply
Leave a Reply. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|






 RSS Feed
RSS Feed