- Home
- About Us
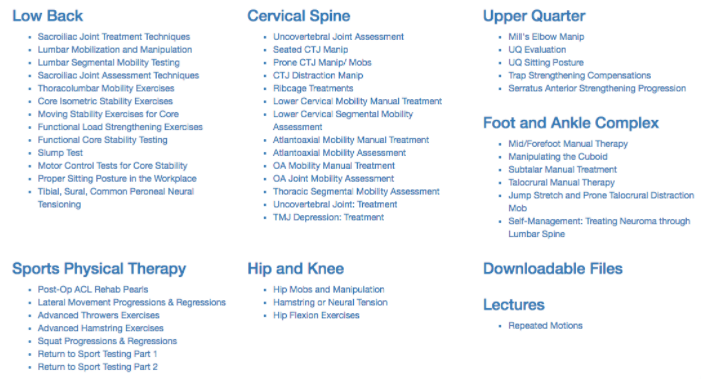
- TSPT Academy
- Online Courses
-
Resources
- Newsletter
- Business Minded Sports Physio Podcast
- Day in the Life of a Sports PT
- Residency Corner
-
Special Tests
>
-
Cervical Spine
>
- Alar Ligament Test
- Bakody's Sign
- Cervical Distraction Test
- Cervical Rotation Lateral Flexion Test
- Craniocervical Flexion Test (CCFT)
- Deep Neck Flexor Endurance Test
- Posterior-Anterior Segmental Mobility
- Segmental Mobility
- Sharp-Purser Test
- Spurling's Maneuver
- Transverse Ligament Test
- ULNT - Median
- ULNT - Radial
- ULNT - Ulnar
- Vertebral Artery Test
- Thoracic Spine >
-
Lumbar Spine/Sacroiliac Joint
>
- Active Sit-Up Test
- Alternate Gillet Test
- Crossed Straight Leg Raise Test
- Extensor Endurance Test
- FABER Test
- Fortin's Sign
- Gaenslen Test
- Gillet Test
- Gower's Sign
- Lumbar Quadrant Test
- POSH Test
- Posteroanterior Mobility
- Prone Knee Bend Test
- Prone Instability Test
- Resisted Abduction Test
- Sacral Clearing Test
- Seated Forward Flexion Test
- SIJ Compression/Distraction Test
- Slump Test
- Sphinx Test
- Spine Rotators & Multifidus Test
- Squish Test
- Standing Forward Flexion Test
- Straight Leg Raise Test
- Supine to Long Sit Test
-
Shoulder
>
- Active Compression Test
- Anterior Apprehension
- Biceps Load Test II
- Drop Arm Sign
- External Rotation Lag Sign
- Hawkins-Kennedy Impingement Sign
- Horizontal Adduction Test
- Internal Rotation Lag Sign
- Jobe Test
- Ludington's Test
- Neer Test
- Painful Arc Sign
- Pronated Load Test
- Resisted Supination External Rotation Test
- Speed's Test
- Posterior Apprehension
- Sulcus Sign
- Thoracic Outlet Tests >
- Yergason's Test
- Elbow >
- Wrist/Hand >
- Hip >
- Knee >
- Foot/Ankle >
-
Cervical Spine
>
- I want Financial Freedom
- I want Professional Growth
- I want Clinical Mastery
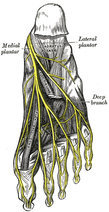 Plantar Fasciosis can be a very difficult condition to treat because of the intricate anatomy of the foot and ankle complex. To complicate issues, we now know that many lower quarter problems root from lumbopelvic and hip dysfunction as well. In previous posts, TSPT has done a literature review of the condition as well as talked about new treatment methods regarding plantar fasciosis. In these posts, one aspect of management we did not discuss in depth is assessing for neuropathic pain. From my clinical experiences and the experiences of my colleagues at the Harris Health System, many patients with plantar fasciosis have positive neural provocation tests for the distal branches of the tibial nerve. Anatomy Review After the tibial nerve passes around the medial malleolus, it splits into three distal branches: the medial plantar nerve, lateral plantar nerve, and medial calcaneal branch. Specifically, the lateral plantar nerve innervates the fifth and lateral 1/2 of the fourth toes and provides motor input to many of the intrinsic foot muscles. The nerve passes laterally across the foot and splits between the flexor digitorum brevis and quadratus plantae. Assessment To assess for tibial nerve adverse neural tension, have the patient lie supine. Passively extend the toes, dorsiflex and evert the ankle. This combined movement place a stress across the tibial nerve and its distal branches. Ask the patient if this position changes their primary symptoms (better, worse, or the same). Next, passively perform a straight leg raise maintaining the foot and ankle components. If this position recreates their primary symptoms, they have positive neural tension in the tibial nerve* (remember to test bilaterally as well). To further assess the tibial nerve, adduct and internally rotate the lower extremity. If the test is positive, appropriate treatment options include nerve sliders, tensioners, and manual therapy. *When performing a straight leg raise, you are changing the hip component. No musculoskeletal structure courses from the hip to the ankle, so if symptoms change it must be the nervous system that is being assessed. Conclusion -Lateral plantar nerve pain can be a contributing factor to plantar fasciosis pain. -By performing the proper assessment (discussed above), you can identify if neural tension is part of your patient's symptoms. -Do not underestimate the impact of the peripheral nervous system in musculoskeletal dysfunction. Lower Extremity Peripheral Nerve Testing [Video taken from TSPT Insider Access Library- subscribe to learn other advanced assessments!] Author: Jim Heafner PT, DPT, OCS is one of the founders of The Student Physical Therapist. He is owner of Heafner Health Physical Therapy in Boulder, Colorado. Are You on the Inside?Looking for advanced sports and orthopedic content? Take a look at our BRAND NEW Insider Access pages! New video and lecture content added monthly.
5 Comments
 In a previous post we have written extensively about the diagnosis and management of plantar fasciopathy. Our literature review regarding conservative management showed modest improvements with the use of calcaneal taping, low level laser therapy, stretching, changing footwear, and others. In many of the controlled trial studies we read, both groups demonstrate improvement (intervention and control) and/or the study has severe limitations. It appears as if time and lifestyle modification are more important than the physical intervention performed. If the literature is consistently lacking, this tells us one of two things: our understanding of the pathology is limited OR we understand the pathology yet are still poorly managing it. In the video below, podiatrist Dr. Ray McClanahan poses some interesting arguments regarding the management of Plantar Fasciosis. For example, he discusses the negative effects of stretching the foot into dorsiflexion, which lengthens the plantar fascia. Dr. Ray states it is more important to stretch the toe extensors into flexion to take tension off the plantar fascia. Additionally he performs soft tissue work to the ADDuctor hallucis muscle in attempt to relax the lengthened and taut ABductor hallucis. His rational: when the ABductor hallucis is taut, the muscle blunts the blood supply to the plantar fascia and dorsal surface of the foot. Check out the video below and let us know what you think! -Jim 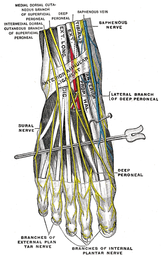 Following a lateral ankle injury, a patient often presents with swelling, pain, decreased ROM, an acute joint dysfunction, and decreased proprioception in the foot and ankle. Depending on the severity of the injury, these symptoms usually begin to improve within a matter of weeks. However, occasionally symptoms persists despite doing all the proper things during your treatment sessions. Most commonly, if a lateral ankle injury occurs the Anterior Talofibular Ligament (ATFL) will be stressed and injured. The mechanism of injury stressing the ligament typically includes adduction and traction of the talus on a plantarflexed and inverted foot. What many individuals fail to consider is the close interaction between the Intermediate Dorsal Cutaneous Nerve (a branch of the superficial peroneal nerve) and ATFL. The Intermediate Dorsal Cutaneous Nerve courses just superior to the ATFL and can also undergo a significant amount of stress during a lateral ankle inversion injury. The nerve is purely sensory and provides sensation to the dorsal aspect of the foot. When the nerve has been irritated, common clinical findings include pain, paresthesia, and a + Tinel's Sign. To check for neural tension in the superficial peroneal nerve (you cannot solely tease out the Intermediate Dorsal Cutaneous Nerve), have the patient lie in supine. Bring the affected foot and ankle into plantar flexion and inversion. Next, perform a straight leg raise on the affected limb while maintaining the foot in PF and Inversion. If pain increases, this is positive neural tension. It is very important to perform the straight leg raise because if you only perform PF and Inversion, pain could be coming from either the ligamentous injury or neural tension. You must further tension the nerve proximally. One should be quick to point out that neural tension may be present, but it is not always the cause of a person's symptoms. In order for the neural tension to be considered relevant adverse neutral tension it must fulfill 3 criteria: 1) Does the test reproduce their pain? 2) Is there a side to side difference? 3) Does the pain change by moving a distant component? Assessing neural tension is one quality that differentiates the novice clinician from an expert. Next time you see a lateral ankle injury, consider the interaction between the Anterior Talofibular Ligament and the Superficial Peroneal Nerve.  Dosage is one of the most important factors to consider when prescribing an exercise. This decision is often made based off level of acuity, tissue type, anatomical location, patient age, and more. In school, one learns the general principles of exercise prescription, but what is often neglected is WHY you prescribe in certain ranges. "Mechanotherapy: how physical therapists' prescription of exercise promotes tissue repair" is a 2009 article published in the Journal of Sports Medicine that elaborates on this topic. Physiologically, what stimulates tissue repair of articular cartilage, muscles and tendons is a term called Mechanotransduction. In this article Mechanotransduction is defined as "the process by which the body converts mechanical loading into cellular responses." This can be thought of in clinical terms as what is occurring at the histological level to allow one to prescribe a certain exercise dosage without increasing the risk of injury. Mechanotransduction can be broken down into 3 phases: 1) Mechanocoupling: This is the physical load cells undergo while in repair. The physical load is transferred into chemical signals which stimulate cellular changes. 2) Cell-Cell Communication: When one cell is stimulated, other cells in the area (whether directly stimulated by the initial mechanical stimulus or not) will undergo a cellular response. 3) Effector Response: When a cell is mechanically stimulated through compression, distraction, etc., several processes will occur intrinsically to allow change to occur. Now knowing each of the 3 stages, you must think about them in relation to the Type of Tissue involved to understand how that tissue heals. Tendon Healing: When a tendon is trying to heal, there is up-regulation of insulin-like growth factor, other growth factors, and cytokines which allows for cellular proliferation and tissue remodeling. Because healing is occur at the cellular level, too much stress OR too little stress on the tendon tissue could cause an alteration in the up-regulation, not allowing the tendon to rehabilitate optimally. The research up-to-date shows that tendons responds positively to "controlled loading." Research focusing on the type and intensity of controlled loading (eccentrics, assisted, resisted) is still ongoing. Muscle: The authors Khan and Scott state that "muscle offers one of the best opportunities to exploit and study the effects of mechanotherapy" because of how muscle tissue responds to loading. We know there is an overload of mechanogrowth factor (MGF) released when load is induced on the muscle force. This in turn causes muscle cell hypertrophy due to a cell-to-cell communication with nearby satellite cells. At this point, the research shows that early loading after a brief immobilization period is essential for minimizing atrophy and restoring normal cellular structure of the muscles. Articular Cartilage: Articular cartilage is comprised of a large population of mechanosensitive cells. It is hypothesized that by repetitively stimulating the articular cartilage with a low load/high repetition exercise dosage, better outcomes will result. One study assessing full thickness cartilage defects following periosteal transplantation demonstrated that individuals who used continuous passive motion (low load/high repetitions) had greater outcomes than those who did not receive this intervention. As with all things, research is ongoing. Bone: When assessing bone healing, osteocytes are the primary mechanosensors. A recent study looking at individuals following a distal radius fracture had stronger bone growth if they received intermittent compression as an adjunct to the standard of care (compression & gripping exercises). The pneumatic compression allowed for extra stimulation of the bone cells and an increased healing rate. We know parts of this article are dense, but understanding what is occurring at the cellular level can greatly change your viewpoint of how various tissues heal. Through each of these tissues we can see that Mechanotherapy plays a unique role in healing of different tissues types. The healing of osteocytes differs from that of chondrocytes which differs from myocytes. It is fundamental to understand these differences in order give appropriate doses during exercise - just as it is important to know the tissue type you should be treating following your examination. As a general rule of thumb: Articular Cartilage: Low Load, High Repetition; ~15% 1 RM; Thousands of repetitions. Tendon: Controlled Loading; consider eccentric exercises, but do not overload the tissue. Muscle: allow for a brief period of immobilization to restore homeostasis following injury. Bone: Based on location of the fracture, consider adding compression to your treatment to improve rate of bone growth and decrease healing time. References:
Khan and Scott. (2009) "Mechanotherapy: how physical therapists' prescription of exercise promotes tissue repair." British Journal of Sports Medicine. 2009; 43: 247-251. Web. 5 Dec. 2013.  If you feel like we having been referencing The Gait Guys a lot recently... it is because we have! They have put out a few great segments recently including this 2 part series on the Power of Observation. As clinical novices, we often do not have enough opportunities to see pathological gait patterns and conditions. As former students, almost of our lab "patients" were healthy classmates. While those experiences were rewarding, they were far from a real situation. In this series, Shawn and Ivo dissect a triathlete's gait pattern. The patient presents with chronic low back pain, but has impairments throughout the entire lower chain. One interesting impairment they discuss is a "clenched fist on the L," which they attribute to flexor dominance and related to decreased arm swing and proprioceptive deficits. Their explanation: the proprioceptive system feeds the cerebellum. The cerebellum helps fire axial extensors. Because proprioception is limited in this athlete, the patient is naturally drawn into a flexor dominant position. Check out the entire post to gain more gems like this one! Because the gait guys use a Tumblr format, you may have to scroll down to June 25 and June 26. Enjoy!  Ankle Dorsiflexion: The What, Why, and How is a recent post from Adam Kelly, ATC at www.eatrunrehabiliate.com. I like this post for a number of reasons: First, I recently had an ankle sprain myself and like a true physical therapist, failed to take the necessary and appropriate rehab measures. I am now dealing with the chronic side-effects of an ankles sprain and am constantly working on my ankle ROM and mechanics. Second, Adam does an excellent job reviewing the anatomy, kinesiology, and mechanics of the ankle. He incorporates the importance of assessing the whole lower chain as well identifying proximal and distal impairments in his patients. Third, he presents a case scenario explaining how deficits at the talocrural joint could affect the average person. Finally, Adam references other professional links and videos, allowing the reader to have a much more comprehensive understanding of evaluation and treatment of the ankle. Some take home points from the the post: 1) When a person lacks ankle mobility, you may not see an immediate decline in functional mobility. The human body has an amazing ability to compensate. It is our ability as practitioners to find these subtle substitutions. 2) When it comes to increasing ankle mobility with manual interventions, a multi-faceted approach is important. We must be dynamic during our treatment sessions. What is successful for one patient may not be appropriate for another patient with similar impairments. 3) Do not forget the above and below. Regional interdependence is so important. As competent clinicians, evaluating tibial torsions, hip mechanics, and mobility of the rearfoot and midfoot must all be considered as contributing impairments. Thanks for the post Adam! -Jim Due to the complexity of the rearfoot and movement in multiple planes, understanding the motions at the talocrural and subtalar joints can be very difficult. This 3D demonstration break down each joint and discusses movement in both the open and closed chain environments. A few take home points:
-Movement at the talocrural joint is primarily in the sagittal plane, resulting in dorsiflexion and plantarflexion. -Movement at the subtalar joint consists of pronation and supination & changes whether it is occuring in open chain or closed chain. -Open-chain pronation: dorsiflexion, eversion, and abduction of the calcaneous -Open-chain supination: plantarflexion, inversion, and adduction of the calcaneous -Closed-chain pronation: calcaneal eversion with plantarflexion and adduction -Closed-chain supination: calcaneal inversion with dorsiflexion and abduction  Stress fractures account for approximately 10% of all athletic injuries. Due to the high amount of impact force, 80-90% of all stress fractures occur in the lower extremities, most commonly seen in the running population. Knowing the high prevalence of stress fractures, it is important to also understand the diagnostic accuracy of the clinical tests one uses to rule-in or rule-less likely a stress fracture. This research article, The Ability of Clinical Tests to Diagnose Stress Fractures: A systematic Review and Meta-analysis, assesses the reliability of both therapeutic ultrasound and the tuning fork test. The review discusses when, why, and how these tests should be implemented. As Schneiders et al, points out "clinically lower-limb stress fractures can be difficult to diagnose, due to a wide range of potential differential diagnoses." This differential diagnosis process should include (but not be limited to) compartment syndrome, muscular strain, tendinitis, tendinosis, infection, and nerve entrapment. Additionally, it is important to know the gold standard for ruling in stress fractures. Currently, a triple phase technium-99 bone scan (scintigraphy) is the most accurate method of diagnosing stress fractures with a sensitivity of 100% and specificity of 76%. MRI has also shown to be highly reliable, but due to its expensive cost, they are less frequently used. Additionally, the single photon-emission CT scan is receiving a lot of attention for it's accuracy in diagnosing stress fractures, but further research is needed. As therapists (excluding the military), we do not have the power to order the gold standard tests mentioned above, so we must rely on our own diagnostic tests to help us interpret our patient's clinical presentation. Clinical tests that are currently used and accepted include therapeutic US, the tuning fork test, superficial palpation, and palpable thickening or swelling of periosteum. This review looked at therapeutic US and the tuning fork.
Unfortunately this systematic review concluded that neither test should be used as stand alone measures for diagnosing stress fractures. Therapeutic US pooled sensitivity (64%) and specificity (63%) revealed a low to moderate performance of the test. A meta-analysis was unable to be performed on the tuning fork test. However, one article by Lesho reported high sensitivity (75%) an moderate specificity (67%) when using the 128 Hz tuning fork. Limitations to this study include an inability to perform heterogenity on the articles and a limitation in the time frame of articles reviewed. Reference:
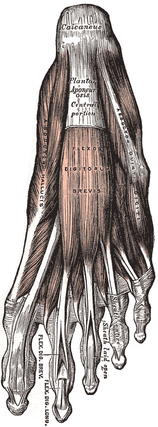
Scneiders A, et al. (2012). The ability of clinical tests to diagnose stress fractures: a systematic review and meta-analysis. JOSPT. 2012; 42.9: 760-771. Web. 1 May 2013.  As physical therapists, we will commonly be asked about running shoes. What is the best shoe on the market? Should I try a minimalist shoe? In this gait guys blog post, they discuss the Dual Density Foam Running Shoe. The authors, Shawn and Ivo, go into detail on what a patient's static posture in a Dual Density shoe could potentially indicate. You need to ask yourself.... Is the person a supinator in a stiff shoe? Is the person an over-pronator that statically stands in excessive supination for support? Could a Tibial Varum be influencing the position of the foot? Where exactly is the pronation occuring? Rearfoot or Midfoot/ Forefoot Pronation? These are all valid questions and performing that differential diagnosis is important! The answer is, it all depends on that individual patient. You must do a complete evaluation with the shoe on and shoe off to see how the patient reacts in both circumstances. Note: Since the Gait Guys have a continuous, running blog, you might have to scroll down to November 21 Post (look for dates on the left side of the blog to see the specific article we are discussing. Look for the title "Dual Density Foam Running Shoes."  It has been estimated that Plantar Fasciitis occurs in approximately 2 million people and can account for between 8% and 15% of all foot pain complaints. While the term "-itis" is often associated with inflammation, there is growing evidence that there might not be an inflammatory state, but rather a degenerative process occurring in the plantar fascia. Because of this growing belief, authors are saying a more appropriate term would be "plantar fasciopathy" or "plantar heel pain." Plantar heel pain is best described as a sharp pain in the patient's rear foot that is worse in the morning (usually the first step out of bed) and at the beginning of a weight bearing activities. The pain typically lessens with continued activity, but often increases toward the end of the day. Individuals most susceptible to developing heel pain are middle-aged women, obese individuals, athletes, and runners. Clinically, you will see excessive pronation and a depressed longitudinal arch in many of these clients. Some extrinsic factors contributing to the pathology include training surfaces, shoe wear, and poor training methods. Understanding the anatomy makes it clear why this population is at an increased risk. The plantar fascia runs from the medial tuberosity of the calcaneus and inserts into the metatarsophalangeal joints, the proximal phalanges, and the flexor tendon sheaths. The fascia is responsible for supporting the longitudinal arch of the foot and assisting in dynamic shock absorption. The attachment of the plantar fascia to the medial calcaneal tuberosity explains why patients often experience pain upon palpation of that area. Diagnosis of plantar fasciopathy is often made on a clinical basis. Due to degenerative changes and tendon thickening, the diagnosis may be made with an ultrasound as well. Current treatment methods include rest, modalities, stretching, strengthening, manual therapy, splinting, orthotics, surgery, and more. New research is constantly being published due to the high incidence of the injury. This review will take an in depth look at several of the available treatment techniques for plantar fasciopathy. Many of the studies we looked at included strengthening and stretching in the treatment plans along with some other intervention. Improvement was often shown in both groups, but we were unable to find any studies that specifically looked at one type of strengthening exercise compared to another. Some of the most common barefoot exercises seen in the clinic include towel scrunching and picking up marbles. Due to the biomechanical theory of the plantar fascia aiding in the support of the medial arch, it would seem logical to include strengthening of the posterior tibialis in rehabilitation. The posterior tibialis is the prime muscle for raising the medial longitudinal arch and can take stress off the plantar fascia. As noted in our previous posts, the exercise to most effectively activate the posterior tibialis is resisted forefoot adduction.
Another study we reviewed compared a new calcaneal taping technique versus a sham taping group, a stretching group, and a no treatment group. The calcaneal taping technique inverted the heel to raise the medial longitudinal arch. A first piece of tape pulled the calcaneus medially. Pieces 2 and 3 followed the same pattern, overlapping 1/3 of each prior piece of tape. Piece 4 wrapped around the heel lateral to medial, supporting the arch and anchoring pieces 1-3. This 4 piece technique was considered quick and cost effective. This calcaneal taping intervention resulted in significantly greater reductions in pain compared to the sham taping, stretching, and no treatment groups. Additionally, a study comparing Medial Arch Support to Low-Dye Taping found that both groups had improvements in pain, but the Medial Arch Support had significantly greater improvements. These interventions should be considered for short-term relief, so that the patient can be pain-free for more intense therapy or activities. A third intervention we reviewed assessed the effects of low level laser therapy in the treatment of plantar fasciitis. Laser treatments were given 3 times per week for 4 weeks with a 30mW . 83 um continuous-wave IR diode laser. The goal of the laser therapy was to alter cellular metabolism, protein synthesis, and create an immune response. The conclusions of randomized controlled evaluation found that low level laser therapy was not beneficial in the treatment of plantar heel pain. A study we looked at compared the effects of stretching and orthotics vs. e-stim, stretching, and orthotics. Both groups improved, but there was not difference between the two groups, so e-stim appears to have no additional benefit. With the recent boom in barefoot running, there has been a movement to begin incorporating barefoot or minimalist exercises/training into rehabilitation of plantar fasciitis. The theory involves placing increased forces on the intrinsic muscles of the foot, so that they can be retrained to support the arch and take stress off the plantar fascia. A study we looked at how the addition of Nike Free 5.0 shoes could affect the patients' complaints. The Nike Free 5.0 shoes offer a flexible midsole that somewhat mimics barefoot training. In the study, two groups were assigned an exercise protocol that involved balance training, stretching and strengthening exercises. One group wore conventional shoes, while the other wore the Nike Free 5.0 shoes. At the end of the study, both groups had a significant decrease in pain, the Nike Free 5.0 shoes more so. Due to the poor design, the results of this study must be looked at closely. At 24 participants, it was a small sample size and there may have been a psychological effect, since the Nike group received new shoes, while the conventional group used old shoes. Along with other factors, it is not clear if minimalist shoes can enhance rehabilitation for individuals with plantar fasciitis. It would be interesting to see the effect of more minimalist-type shoes (New Balance Minimus, Vibram Five Finger, etc.) could have on therapy in a properly done study.
One of the more common interventions that is performed is stretching. A study we looked at compared the results of the standard achilles tendon stretch to a sitting plantar fascia stretch. For the plantar fascia stretch, the patient would cross his/her legs and place the affected foot on the opposite knee. The patient then grasps the toes (especially the big toe) and maximally dorsiflexes them until a stretch is felt in the foot. In the study, the patients would perform their stretch first thing in the morning and before getting up after sitting for awhile. The study found both interventions to be successful, but the plantar fascia specific stretch more so. It should be noted that the study had no true control to rule out the patients' improvements due to natural healing processes. Dry needling is still a limited treatment technique for physical therapists; however, patients can have access to acupuncture on a wider basis. One article compared two groups to see the effect of acupuncture on plantar fasciitis. Both groups received standard treatments, such as icing, stretching, intrinsic foot strengthening, and NSAIDs. One group received acupuncture, additionally. Both groups found improvements in pain. There was no difference between the two groups after 4 weeks, but the acupuncture group was slightly better after 8 weeks. A treatment technique that is gaining popularity involves Instrument Assisted Soft Tissue Mobilization (IASTM). There are many products out there that fall under the category of IASTM: Graston Technique, ASTYM, Edge Tool, etc. The theory is generally the same behind them in that, through use of the tools, a healing inflammatory phase can be initiated by stimulating blood flow, nutrients, and fibroblasts to the area. Through proliferation of the fibroblasts, healing and formation of collagen can begin. The soft tissue mobilization can additionally aide in reorganization of the collagen fibers to proper orientation. This study in particular was a preliminary look at Graston Technique, discussing the theory, protocol, initial evidence, and some case studies. As plantar fasciitis is a soft tissue pathology, IASTM could have useful implications for patients with this disorder. When further research is performed on the subject, it may be found that IASTM has a very important place in treating these patients. References:
Abd El Salam MS, Abd Elhafz YN. "Low-dye taping versus medial arch support in managing pain and pain-related disability in patients with plantar fasciitis." Foot Ankle Spec. 2011 Apr;4(2):86-91. Web. 10/13/12. Bassford, Jeffrey. "A Randomized Controlled Evaluation of Low Level Laser Therapy: Plantar Fasciitis." Arch Phys Med Rehabil. 79. (1998): n. page. Web. 8 Oct. 2012. Beyzadeoğlu T, Gökçe A, Bekler H. "[The effectiveness of dorsiflexion night splint added to conservative treatment for plantar fasciitis]." Acta Orthop Traumatol Turc. 2007;41(3):220-4. Web. 10/13/12. Digiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, Baumhauer JF. "Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up." J Bone Joint Surg Am. 2006 Aug;88(8):1775-81. Web. 10/12/12. Hammer, WI. "The effect of mechanical load on degenerated soft tissue." J body Mov Ther. 12.3 (2008): 246-256. Web. 8 Oct. 2012. Hyland, Matthew. "Randomized Control Trial of Calcaneal Taping, Sham Taping, and Plantar Fascia Stretching for the Short-term Management of Plantar Heel Pain." Journal of Orthopaedic and Sports Physical Therapy. 36.6 (2006): n. page. Web. 8 Oct. 2012. Karagounis P, Tsironi M, Prionas G, Tsiganos G, Baltopoulos P. "Treatment of plantar fasciitis in recreational athletes: two different therapeutic protocols." Foot Ankle Spec. 2011 Aug;4(4):226-34. Web. 10/13/12. Lee SY, McKeon P, Hertel J. "Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis." Phys Ther Sport. 2009 Feb;10(1):12-8. Web. 10/10/2012. Renan-Ording, Romulo. "Effectiveness of Myofascial Trigger Point Manual Therapy Combined with a Self-stretching Protocol for the Management of Plantar Heel Pain: A Randomized Control Trial." Journal of Orthopedic and Sports Physical Therapy. 41.2 (2011): 43-51. Web. 8 Oct. 2012. Ryan, M, S Fraser, K McDonald, and J Taunton. "Examining the degree of pain reduction using a multielement exercise model with a conventional training shoe versus an ultraflexible training shoe for treating plantar fasciitis." Phys Sportsmed. 37.4 (2009): 67-84. Web. 10 Oct. 2012. Stratton M, McPoil TG, Cornwall MW, Patrick K. "Use of low-frequency electrical stimulation for the treatment of plantar fasciitis." J Am Podiatr Med Assoc. 2009 Nov-Dec;99(6):481-8. Web. 10/13/12. |
Dr. Brian Schwabe's NEW Book in partner with PaleoHacks!
Learn residency-level content on our
Insider Access pages We value quality PT education & CEU's. Click the MedBridge logo below for TSPT savings!Archives
July 2019
Categories
All
|









 RSS Feed
RSS Feed